Central Nervous System Infectious Inflammation
Revision as of 12:52, 8 March 2011 by Bara (talk | contribs) (Created page with "==Routes of Entry== * CNS inflammation is usually the result of infection. ** This may be caused by: *** Bacteria *** Fungi *** Protozoa *** Viruses * Organisms must first enter...")
Routes of Entry
- CNS inflammation is usually the result of infection.
- This may be caused by:
- Bacteria
- Fungi
- Protozoa
- Viruses
- This may be caused by:
- Organisms must first enter the CNS in order to establish infection.
- There are several routes of entry that allow this:
- Haematogenous entry
- This is the most common route.
- Entry via the peripheral nerves
- Organisms track within the axoplasm of axons.
- For example, Listeria monocytogenes.
- Penetrating trauma
- For example, dehorning wounds, skull fracture or tail docking.
- Direct spread of infection
- From the nasal cavity, middle ear or paranasal sinuses.
- Haematogenous entry
- There are several routes of entry that allow this:
Localisation of Infectious Organisms
- After entry, organisms may establish in one or more of four main areas:
- Epidural space
- Infection tends to manifest as abscess formation.
- Subdural space
- Manifests as abscess formation.
- Fairly uncommon.
- Leptomeninges
- Causes leptomeningitis, which may be:
- Suppurative
- The most common form.
- Neutrophils are the predominant cell type.
- Caused by bacteria
- E.g. E. coli and Streptococcus
- There are often no gross lesions, but the brain may appear swollen and the meninges opaque.
- Usually results in death.
- Eosinophilic meningoencephalitis
- The classic example of this is porcine salt poisoning, when water has been restricted and the suddenly replenished.
- Perivascular eosinophilic cuffing is seen in the cerebrum and meninges.
- Lymphocytic
- Usually of viral origin.
- Granulomatous
- Caused by fungal diseases and Mycobacteriosis.
- Suppurative
- Causes leptomeningitis, which may be:
- CNS parenchyma
- Epidural space
Bacterial Infections
- Bacterial infections typically result in abscesses.
- These may be single or multiple depending on the route of entry, and vary in size.
- They contain a central, liquefied cavity.
- There are differences between cerebral abscesses and those occuring elsewhere.
- Encapsulation is slow.
- This is due to a lack of fibroblasts.
- There is therefore less collagen in the capsule.
- Astrocytic glial fibers are not as strong as collagen
- Encapsulation is slow.
- Other organisms may cause similar infections:
- Rickettsial organisms
- E.g. Ehrlichia
- Spirochates
- E.g. Leptospirosis
- Rickettsial organisms
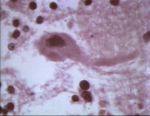
Viral Infections
- Viral infections tend to reach the CNS by haematogenous spread and via peripheral nerves.
- There are three hallmark lesions of CNS viral infections:
- Neuronal necrosis
- Gliosis
- Vascular changes
- Several types of virus may cause inflammation in the CNS.
- Neurotropic, e.g.
- Rabies (rhabdovirus)
- Aujesky’s disease (herpesvirus)
- Visna (ovine lentivirus)
- Endotheliotropic, e.g.
- Infectious canine hepatitis (canine adenovirus)
- Classical swine fever (pestivirus)
- Equine herpesvirus type 1 (herpes)
- Pantropic
- Infectious canine distemper (morbillivirus)
- Infectious bovine rhinotracheitis (bovine herpesvirus type 1)
- Neurotropic, e.g.
- Other examples of viruses affecting the CNS:
- Distemper
- Parvovirus
- Parainfluenza
- Herpes
- FIP
- FIV
- FeLV
- Pseudorabies
- Rabies