Recurrent Airway Obstruction
| This article is still under construction. |
Also known as: RAO, chronic obstructive pulmonary disease, COPD, heaves.
Do not confuse with: summer pasture associated obstructive pulmonary disease.
Description
Recurrent airway obstruction (RAO) is an inflammatory, obstructive respiratory disease of horses. Disease is induced by the exposure of susceptible animals to organic dust, which gives neutrophil influx to the airways, bronchospasm and mucus accumulation1. This causes a cough, nasal discharge, and respiratory difficulty. When exposure to the allergen is eliminated, obstruction and clinical signs resolove or attenuate. However, animals are susceptible to reccurent episodes of airway obstruction throughout their lives, and so management is essential.
Since disease required exposure to organic dust, recurrent airway obstruction occurs in stabled horses that are, for example, bedded on straw and fed hay. The condition is therefore most prevalent in the northern hemisphere because horses tend to be stabled for large parts of their lives2. Summer pasture-associated obstructive pulmonary disease (SPAOD) is a similar condition that occurs when horses kept on pasture are sensitive to environmental allergens, and may be considered the same disease as RAO but with different inciting factors1.
Pathogenesis
When a horse with a history of RAO is moved from pasture to a stable, the hay it is fed and the straw it is bedded on harbour organic dusts. These dusts contain components which are capable of causing inflammation of the lungs, such as specific allergens, endotoxin, moulds and small particulate matter1. Although small particles and endotoxin are known to cause pulmonary inflammation, there is evidence to suggest that there is an allergic component to recurrent airway obstruction. For example, bronchoalveolar lavage fluid in RAO has been shown to have increased levels of IgE specific for various mouldshaliwell, and the cytokine response appaears to be skewed towards TH2lavoi: both of these facts are suggestive of an allergic mechanism.
On exposure to dust, neutrophils accumulate in the lung and quickly invade the lumen of the airway1. Aiway obstruction then develops due to several mechanisms. Mucus becomes more viscous and accumulates in the luman, and bronchospasm is initiated by the actions of inflammatory mediators on airway smooth muscle and cholinergic nervesOlszewski. Oedema of the airway wall also contributes to narrowing, and in horses suffering chronic disease, the wall remodels to give mucus metaplasia, smooth muscle hypertrophy and peribronchial fibrosis1, allen.
Signalment
RAO usually becomes apparent in middle-aged and older horses, and persists for lifeallen. There is some evidence that there may be a genetic component to the disease, as many horses do not suffer RAO when they are housed in environments that can provoke clinical disease in othersmarti.
Diagnosis
A presumptive diagnosis may be made on the basis of the history and clinical examination.
Clinical Signs
Mildly affected horses generally present with a history of occasional coughing and exercise intolerance. Signs become more obvious as the disease progresses. Tachypnoea is often seen, and there may be a mucopurulent nasal discharge. Severely affected animals show signs of respiratory distress at rest. These can include flared nostrils, wheezing, paroxysmal bouts of coughing and a laboured abdominal component to expiration. Chronically, marked dyspnoea increases energy expenditure and the animal may lose condition, as well as developing a "heave line" due to hypertrophy of the external abdominal oblique muscleallen, merck, ivis. Fever does not normally develop unless there are secondary bacterial complications.
On physical examination, thoracic auscultation typically reveals a prolonged expiratory phase of respiration and adventitious respiratory noises. Wheezes are most pronounced during expiration, and crackles are associated with the excessive mucus productionmerck. However, the airways are so obstructed in some severely affected animals that there is insufficient air movement to generate audible breath sounds, and the lungs are very quiet on auscultation1. In mildly affected horses, a rebreathing bag can be used to aid auscultation, but this should never be performed in dyspnoeic animals1, allen. There may be an increased sensitivity of the cough reflex on tracheal compression.
Diagnostic Imaging
Endoscopy reveals excessive mucopurulent secretions in the trachea. Thoracic radiographs may be useful in cases that are not typical in their presentation or response to treatment, as they may help rule out other differentials such as including interstitial pneumonia, pulmonary fibrosis, or bacterial pneumonia1, allen.
merck Radiographic findings in horses with RAO are peribronchial infiltration and overexpanded pulmonary fields (flattening of the diaphragm). Thoracic radiographs are of little benefit in confirming the diagnosis of RAO and may not be necessary in horses with characteristic clinical signs, unless there is no response to standard treatment after 14 days of therapy. However, they may be helpful in identifying the most important differential diagnoses, i
Laboratory Tests
Routine haematology and biochemistry are usually within normal limits.
fluids obtained from tracheal wash (TW) and BAL are characterised by a marked neutrophilia. BAL should not be performed if the horse is markedly dyspnoeic and should be postponed until the dyspnoea is controlled. There is little evidence to support the use of serum and intradermal allergy testing in the diagnosis of RAO.
merck Bronchoalveolar lavage is rarely required for diagnosis of fulminant RAO, and is not innocuous in horses that are dyspneic at rest. It is indicated in horses with mild to moderate disease with poor performance and coughing during exercise. Neutrophilic inflammation (20-90% of total cell count) confirms the presence of lower airway inflammation and differentiates horses with eosinophilic pneumonitis, fungal pneumonia, or lungworm infestation from horses with heaves. Curschmann’s spirals may be observed on cytologic evaluation and represent inspissated mucus/cellular casts from obstructed small airways
ivis The severity of lung inflammation can be evaluated by cytological evaluation of bronchoalveolar lavage fluid (BALF; see chapter by Viel and Hewson for lavage and cytology techniques). In normal horses, lymphocytes and macrophages form the majority of cells in BALF and neutrophils comprise less than ten percent of cells. In horses with RAO or SPAOD, there is an increase in the percentage of neutrophils and, in severely affected animals, neutrophils comprise over 50 percent of cells and are not degenerate. Despite the large number of neutrophils in BALF, there is no evidence of bacterial infection. Aspiration of tracheal mucus or a tracheal lavage can also be used to evaluate lung inflammation but it is less reliable than BALF. Because there can be increased numbers of neutrophils in the tracheal wash but not in BALF [52], it is wiser to base evaluation of peripheral lung inflammation on the cytology of BALF. Presumably increased numbers of neutrophils in the tracheal secretions reflect local tracheal inflammation that does not extend deeper into the lung. Mixed populations of bacteria are common in a tracheal wash and usually are of no significance.
Other Tests
Reduction of respiratory distress after the administration of a bronchodilator confirms the presence of bronchospasm1, allen. To test this, intravenous atropine can be administered at 0.02mg/kg. Horses with RAO (or SPAOD) should respond within 15 minutes1. The dose of atropine should not be repeated as there is a risk of intestinal stasis.
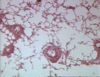
Pathology
Treatment
Links
References
- Robinson, N E (2001) Recurrent Airway Obstruction. In Equine Respiratory Diseases, IVIS.
- Robinson N E et al (1995) The pathogenesis of chronic obstructive pulmonary disease of horses. The British Veterinary Journal, 152, 283-306.
- Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition), Merial.
- Allen, K and Franklin, S (2007) RAO and IAD: respiratory disease in horses revisited. In Practice, 29(2), 76-82.
- Halliwell R E W et al (1993) Local and systemic antibody production in horses affected with chronic obstructive pulmonary disease. Veterinary Immunology and Immunopathology, 38, 201-215.
- Lavoie J P et al(2001) Neutrophilic Airway Inflammation in Horses with Heaves Is Characterized by a Th2-type Cytokine Profile. American Journal of Respiratory and Critical Care Medicine, 164, 1410-1413.
- Marti, E et al (1991) The genetic basis of equine allergic diseases 1. Chronic hypersensitivity bronchitis. The Equine Veterinary Journal, 23, 457-460.
- Olszewski M A et al (1999) Pre- and postjunctional effects of inflammatory mediators in horse airways. American Journal of Physiology, 277, 327-333.
- McGorum, B et al (2007) Equine respiratory medicine and surgery, Elsevier Health Sciences.
- Durham, A (2001) Update on therapeutics for obstructive pulmonary diseases in horses. In Practice, 23(8), 474-481.