Muscle Regeneration
Jump to navigation
Jump to search
Response to injury
- Limited array of ways in which to respond to injury
- Degeneration
- Necrosis
- Regeneration
- Atrophy
- Hypertrophy
- Large number of factors indicing the changes above, e.g.:
- Trauma
- Toxins
- Infectious agents
- Nutritional deficiencies
- Ichaemia
- Hereditary diseases
- Specific diagnosis is often not possible based on morphological or histological features alone
- Additional tests, clinical information and history are often required
Regeneration
- Skeletal muscle myofibres have substantial regenerative ability
- Success depends on:
- An intact sarcolemmal tube - to act as a support and guide
- Availability of satellite cells - to act as progenitor cells for new sarcoplasm production
- Macrophages to clear up cell debris
- If these conditions are not met (e.g. severe thermal damage) fibrosis will occur
- Stages:
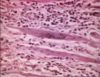
- Nuclei in necrotic segement disappear, hyalinased sarcoplasm due to loss of normal myofibrillar structure, may separate from adjacent normal myofibrils and/or mineralise
- Monocytes from capillaries -> macrophages in necrotic portion, satellite cells swell -> vesicular with prominent nucleoli -> mitosis (within 1-4 days after initial injury)
- Satellite cells move to centre
- Macrophages clear the sacrolemmal tube, plasmalemma disappears, shape maintained by basal lamina
- Satellite cells -> myoblasts (contain myosin) -> fuse forming myotubes with row of central nuclei; cytoplasmic processes fusing
- Growing and differentiating fibre, striations appear - formation of sarcomeres
- Nuclei move to peripheral position (2-3 weeks after initial injury)
- Regeneration by budding
- When conditions are not optimal, disrupted sacrolemma
- E.g. injection of irritating substance, trauma, infarction
- Myoblasts proliferate -> sacrolamma bulges from cut part -> club-shaped with numerous central nuclei = muscle giant cells
- Monophasic lesions - all at same phase above