Respiratory System General Introduction - Pathology
Jump to navigation
Jump to search
Invasion of respiratory system
- The most common respiratory diseases seen in domestic animals are those caused by microbiological agents (particularly viruses, bacteria and mycoplasma), parasites, secondary neoplasia and cardiovascular abnormalities.
- There are three main routes of invasion into the respiratory tract: - AEROGENOUS (via airways), HAEMATOGENOUS (via blood), TRANSCOELOMIC (direct).
Aerogenous
- Infection reaches the lung as inhaled droplets or larger food particles or fluid
- Particles > 10um will usually be deposited above the larynx
- Many smaller particles will also interact with the mucosa of the nasal cavity and nasopharynx
- Hence many viral and bacterial diseases initially replicate in the epithelium and lymphoid tissue of the upper respiratory tract - before either spreading systemically or being redistributed to the lower respiratory tract
- As particle size decreases, aerodynamic properties increase hence an increased proportion of particles will pass down the respiratory tract
- Irritant/ infectious particles that are ~ 1-2 um in size will deposit mostly at the bronchiolar-alveolar junction
- Due to mechanics of air flow in this area:
- Total air space area suddenly increases -> air stream velocity rapidly drops -> time for particles to settle by gravity
- Major reason why the bronchiolar-alveolar junction is vulnerable to damage caused by inhaled irritants
- Total air space area suddenly increases -> air stream velocity rapidly drops -> time for particles to settle by gravity
Haematogenous
- Distribution tends to be to caudal lobes
- But all lobes are affected when number of particles is high
- There is no orientation on the airways
Transcoelomic
- Infection via extension from pleura or mediastinum, or traumatic penetration from chest wall (e.g. bite), diaphragm (e.g. bovine traumatic reticulitis) or oesophagus (e.g. foreign body).
Repair in the respiratory tract
Functional anatomy
Mucosa
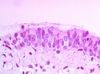
- Mucosal epithelium
- Nares and epiglottis- stratified squamous
- Nasal cavity, paranasal sinuses, larynx, trachea - pseudostratified, columnar, cilliated, olfactory
- Submucosa
- Submucosal glands
- Lymphoid tissue
- Blood vessels, lymphatics and nerves
- Very rich blood supply to nasal mucosa
Nasal chambers and turbinates
- Scrolls of turbinate bone - increase surface area
- Arrangements vary with species
- Remove particels above 10-20um in size
- Humidifies and warms incoming air
- Detects noxious irritants
Nasal septum
- Full length of nasal chamber in horses
- 2 openings into pharynx
- Partial length in other species
- Single opening into pharynx
Sinuses
- Size, arrangement and number vary with species
- Poorly developed in carnivores
- Poor communication of frontal sinus in cats with nasal cavity
- Predisposed to frontal sinus bacterial infections
- Maxillary sinus opening very large - 'maxillary recess'
- Maxillary sinus infections very uncommon in carnivores
- Highly developed in horses
- Slit-like, high openings in horses
- Predisposed to bacterial infections
- Cheek teeth embedded within the maxillary sinuses
- Maxillary sinusitis secondary to tooth root abscesses
- Poor communication of frontal sinus in cats with nasal cavity
Nasopharynx
- Ciliated pseudostratified epithelium
- Many lymphoid nodules in submucosa
Larynx
- Epiglottis prevents entry of food into the trachea
Guttural pouch
- Horses
- Diverticulaof the eustachian tubes with thin slit-like openings (ostia) at the rostroventral aspect into the pharynx
- Ostia open during geglutition
- Mucous secretions drain out of the pouch when the horse lowers its head
- Each pouch is divided into lateral and medial compartments by the stylohyoid bone
- Medial compartment bordered by:
- Internal carotid artery
- Cranial sympathetic nerves
- Cranial cervical ganglion
- Cranial nerves: glossopharyngeal (IX), vagus (X), accessory (XII) and hypoglossal (XII)
- Lateral compartment bordered by:
- External carotid and maxillary arteries
- Cranial nerve: facial (VII)
- Lined by respiratory epithelium
Larynx
- Stratified squamous epithelium and ciliated respiratory epithelium
- Supported by cartilage
Trachea
- Most domestic animals - pseudostratified epithelium, ciliated, non-ciliated and mucous cells
Bronchi
- Cartilage, smooth muscle seromucous glands, and ciliated epithelium with goblet cells.
- Defence mechanisms therefore are the same as the URT mucosa but also include:
- Coughing
- Bronchial associated lymphoid tissue (BALT) covered by M cells (microfold cells) where there is professional APC and lymphocytes trafficking.
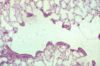
Bronchioles
- The bronchioles form a transition zone between the airway conducting system and the alveoli (gas-exchange region).
- A number of anatomical features of the bronchioles render them vulnerable to insult.
- Diminished mucociliary defences due to:
- No goblet cells in the mucosal epithelium
- No submucosal seromucous glands (except in the cat)
- Smaller and fewer cilia present on the respiratory epithelium
- No supporting cartilage rings
- Clara cells (non-cilliated columnar epithelial cells) are present that are metabolically active (rich in cytochrome p450 enzymes ie: just like the liver), with a role in bioactivation or detoxification of metabolites/drugs.
- Can produce reactive metabolites that result in further pulmonary damage eg: fog fever in cattle
- Alveolar macrophages and neutrophils accumulate at the terminal bronchioles
- Activation during inflammation and may result in release of free radicals, resulting in oxidative damage to adjacent bronchiolar cells.
- More prone to obstruction than bronchi when inflamed
Lungs
- The lung receives half of the cardiac output and must rapidly exchange gases with this large blood volume through a vast alveolar membranous surface
- This makes the lung vulnerable to circulatory disturbances, most notably pulmonary oedema
- Normally, mechanisms are in place to protect the lung from the entry of circulatory fluid into alveolar spaces
- Alveolar epithelium and its intercellular junctions are highly impermeable to fluid and seal off alveolar spaces
- Interstitium of alveolar septa is at lower pressure than intra-alveolar pressure
- Interstitial pressure becomes increasingly sub-atmospheric (negative) toward the fascia surrounding vessels and airways and towards the pulmonary hilus
- The net effect is that liquid moves from the alveolar interstitum towards lymphatics in the fascia and then the hilus of the lung and mediastinum
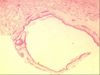
Pleural membranes
- Lined with mesothelial cells
Defense mechanisms
Particle deposition
- Coiled nature of turbinates promotes turbulent airflow and impaction of large particles >10 μm in diameter onto the nasal mucosa
Mucociliary escalator
- Extends from terminal bronchioles to larynx
- Cilia on the respiratory epithelium beat in a co-ordinated manner
- Cilia beat in a caudal direction in nasal cavity
- Cilia beat in a cranial direction in trachea and lower airways
- Mucus is swallowed when it reaches the nasopharynx
- Constant movement reduces chances that pathogens can adhere to the respiratory epithelium
Mucus
- Produced by the goblet cells of the respiratory epithelium and the submucosal glands with contribution from lacrimal glands draining into the nose
- Traps particles for transportation away and subsequent swallowing
- Physical barrier against mucosal damage
- Prevents dessication of the mucosal epithelium
- Contains antimicrobial substances
- Immunoglobulin - IgA
- Lysosyme
- Direct action on bacterial cell walls
- Lactoferrin
- Inhibits bacterial growth as sequesters iron, an essential co-factor for many bacteria
- This mucous blanket is contributed to by the secretions of the Clara cells in the terminal and respiratory bronchioles
- Also contained in these secretions in the respiratory tract are: IgA, IgG, and Interferon
- At all levels of the tract, and especially at bifurcations, there are subepithelial leukocytes which have the potential to develop into lymphoid follicles under a persistent antigenic challenge
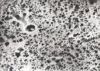
Alveolar macrophages
- Phagocytes resident within the alveolus
- There is normally one sentinel macrophage per alveolus and they ingest particles which reach the alveolus
- When activated by such irritants, they have increased phagocytic and bactericidal capability and are able to recruit further macrophages (monocytes from the blood), and also to attract neutrophils and other leukocytes to the site
- Removal of phagocytosed irritants may be via the mucociliary escalator or carried to the interstitium for sequestration in the connective tissue
Commensal bacteria
- The normal bacterial flora of the nasal cavity, pharynx, larynx and proximal portion of the trachea compete with potentially pathogenic bacteria and help to prevent their colonisation (competitive exclusion).
- The airway environment distal to the mid-portion of the trachea is effectively sterile.
- Gram positive bacteria
Reflexes
- Sneezing
- Coughing