Difference between revisions of "Bronchiectasis"
Jump to navigation
Jump to search
| (One intermediate revision by the same user not shown) | |||
| Line 5: | Line 5: | ||
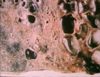
*Permanent, abnormal saccular or cylindrical dilation of bronchi | *Permanent, abnormal saccular or cylindrical dilation of bronchi | ||
*Accumulation of exudate within the lumen and partial rupture of bronchial walls | *Accumulation of exudate within the lumen and partial rupture of bronchial walls | ||
| − | *Sequel to [[Bronchitis#Chronic bronchitis|chronic bronchitis]] as result of an unresolved persistent [[Bronchopneumonia|bronchopneumonia]] | + | *Sequel to [[Bronchitis#Chronic bronchitis|chronic bronchitis]] as result of an unresolved persistent [[Lungs Inflammatory - Pathology#Bronchopneumonia|bronchopneumonia]] |
*Chronic inflammation within the bronchial mucosa and wall -> release of proteolytic enzymes from [[Neutrophils|neutrophils]] and macrophages -> destruction of supporting structures in the bronchial walls (eg: cartilage, connective tissue) -> weakens the bronchial walls and damages lining mucosal epithelial cells and their cilia (damage to mucociliary escalator) | *Chronic inflammation within the bronchial mucosa and wall -> release of proteolytic enzymes from [[Neutrophils|neutrophils]] and macrophages -> destruction of supporting structures in the bronchial walls (eg: cartilage, connective tissue) -> weakens the bronchial walls and damages lining mucosal epithelial cells and their cilia (damage to mucociliary escalator) | ||
| − | *[[Atelectasis|Atelectasis]] in the surrounding lung parenchyma results in increased inspiratory effort and increased intrathoracic negative pressure during inspiration | + | *[[Lungs Ventilation - Pathology#Atelectasis|Atelectasis]] in the surrounding lung parenchyma results in increased inspiratory effort and increased intrathoracic negative pressure during inspiration |
*The weakened bronchial walls are less able to 'resist' the negative pressure and therefore dilate excessively. | *The weakened bronchial walls are less able to 'resist' the negative pressure and therefore dilate excessively. | ||
*With time this dilation becomes permanent as a viscous cycle of exudate pooling in the lumen and increased contact of the bronchial walls with the leukocytes further weakens the bronchial walls. | *With time this dilation becomes permanent as a viscous cycle of exudate pooling in the lumen and increased contact of the bronchial walls with the leukocytes further weakens the bronchial walls. | ||
Revision as of 16:32, 19 February 2011
- Permanent, abnormal saccular or cylindrical dilation of bronchi
- Accumulation of exudate within the lumen and partial rupture of bronchial walls
- Sequel to chronic bronchitis as result of an unresolved persistent bronchopneumonia
- Chronic inflammation within the bronchial mucosa and wall -> release of proteolytic enzymes from neutrophils and macrophages -> destruction of supporting structures in the bronchial walls (eg: cartilage, connective tissue) -> weakens the bronchial walls and damages lining mucosal epithelial cells and their cilia (damage to mucociliary escalator)
- Atelectasis in the surrounding lung parenchyma results in increased inspiratory effort and increased intrathoracic negative pressure during inspiration
- The weakened bronchial walls are less able to 'resist' the negative pressure and therefore dilate excessively.
- With time this dilation becomes permanent as a viscous cycle of exudate pooling in the lumen and increased contact of the bronchial walls with the leukocytes further weakens the bronchial walls.
- Most severe in cattle (complete lobular septation and lack of collateral ventilation), least severe in dogs (good colateral ventilation), also seen in sheep, goats and pigs
- In very severe cases, the bronchial wall is completely destroyed and unrecognisable - an abscess