Bronchitis
Acute bronchitis/bronchiolitis
- Inflammation of the bronchi - bronchitis
- Inflammation of the bronchioles - bronchiolitis
- Types... as expected, depending on the severity and type of insult/injury:
- serous
- catarrhal
- purulent
- fibrinous
- necrotizing
- granulomatous
- Acute inflammation passes through the same stages as in rhinitis
- Evolution to chronic inflammation may occur following chronic or repeated infections or irritation by parasitic, allergic agents or inhaled substances.
Chronic bronchitis
- The quantity of mucus is increased following mucus gland and goblet cell hyperplasia
- The mucosa is thickened due to:
- mucus gland hyperplasia
- leukocytic infiltrates
- lymphocytes, plasma cells, macrophages, eosinophils
- squamous metaplasia of the lining epithelium (ciliated epithelium replaced by more resistent but relatively non-functional squamous epithelium) - affects mucociliary clearance
- In dogs
- Bronchial irritation and mucus hypersectretion causes chronic intractable cough
- At post-mortem, trachea and lower airways are full of mucoid or mucopurulent exudate
- Underlying bronchial mucos is thickened, hyperaemic and oedematous
- May be a coexisting bronchopneumonia
- Smooth muscle hypertrophy in pulmonary arteries -> pulmonary hypertension -> cor pulmonale
Chronic bronchiolitis
- Alterations in the bronchiolar fluid and wall, depending on the severity and chronicity of the injury.
- Normal serous, bronchiolar fluid may become mucoid because of a goblet cell metaplasia associated with the epithelial hyperplasia
- Mucous is more viscous than serous fluid and therefore may not be cleared from the airways by the usual clearance mechanisms (eg: cystic fibrosis in people - the underlying cause of the airway pathology is the decreased water content of the airway mucous, leading to airway plugging, and increased risk of secondary infection)
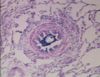
- The normally thin bronchiolar walls can become thickened with fibrous connective tissue and infiltrated by leukocytes (macrophages, lymphocytes, plasma cells, +/- eosinophils).
- Potential aetiologies
- Infectious agents by either
- Extension from an upper airway infection
- Lower respiratory tract infections
- Bronchiolitis often occurs with many causes of pneumonia
- Foreign bodies eg: grass seeds
- Irritants
- Parasites
- Allergens
- Metabolic activation of compounds by Clara cells in the bronchioles (eg: Fog Fever in cattle)
- Infectious agents by either
- Bronchioles are more susceptible to obstruction than bronchi and the epithelium is highly susceptible to injury due to changed anatomy
Sequelae of bronchitis or bronchiolitis
- Resolution of inflammation, removal of cellular debris and lumenal exudate with minimal mural fibrosis ... return to normal function.
- Obstruction of the airways following:
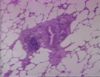
- Plugging of the lumen by mucus, neutrophils and cellular debris
- Severe thickening of the airway walls
- Bronchoconstriction following contraction of smooth muscle surrounding the airways eg: hypersensitivity response, asthma +/- hypertrophy of airway smooth muscle
- Depending on severity can result in:
- Dyspnoea
- Increased respiratory noise (crackles, wheezes)
- Reduced oxygenation, exercise intolerance, lethargy
- Collapse of areas of the lung (atelectasis)
- Overinflation of other parts of the lung (emphysema)
- Chronic cough
- Pneumonia following inhalation of inflammatory exudate/infectious material within it
Infectious causes of bronchitis or bronchiolitis