Difference between revisions of "Hyperparathyroidism"
Jump to navigation
Jump to search
| (24 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
| − | + | [[Image:parathyroidadeoma.jpg|thumb|right|100px|Parathyroid adenoma. Image courtesy of Biomed Archive.]] | |
| − | + | ===Primary=== | |
| + | * Primary hyperparathyroidism is caused by glandular hyperplasia or neoplasia. [[Image:parathyroidhyperplasia.jpg|thumb|right|100px|Parathyroid hyperplasia. Image courtesy of Biomed Archive.]] | ||
| + | * Rare. | ||
| + | ===Secondary=== | ||
| + | * Secondary hyperparathyroidism causes [[Hyperparathyroidism|fibrous osteodystrophy or "rubber jaw"]]. | ||
| + | * In secondary hyperparathyroidism, the gland is overactive due to another condition coexisting in the body, rather than a primary parathyroid gland defect. | ||
| + | * There are two common forms of secondary hyperparathyroisism: | ||
| + | *# [[Hyperparathyroidism#Nutritional Hyperparathyroidism|'''Nutritional Hyperparathyroidism''']] | ||
| + | *#* This includes [[Metabolic Bone Disease|Metabolic Bone Disease]]. | ||
| + | *# [[Hyperparathyroidism#Renal Hyperparathyroidism|'''Renal Hyperparathyroidism''']] | ||
| + | * Both forms result in increased osteoclastic resorption of bone and deposition of fibro-osteoid matrix that fails to mineralise. | ||
| + | ** Flat bones of the skull swell. | ||
| + | ** Fibrous tissue is seen around the tooth roots. | ||
| + | ** Bone softens in adult animals. | ||
| + | *** This is what gives rise to the term "rubber jaw". | ||
| + | *** Long bones become soft with thin cortices. | ||
| + | **** These fracture easily. | ||
| + | ====Nutritional Hyperparathyroidism==== | ||
| + | [[Image:secondaryhyperparathyroidism.jpg|thumb|right|100px|Secondary hyperparathyroidism - "rubber jaw". Image courtesy of Biomed Archive.]] | ||
| + | * Nutritional hyperparathyroidism is also known as nutritional osteodystrophy. | ||
| + | * This occurs most commonly in: | ||
| + | ** Young, fast-growing animals | ||
| + | ** Animals with a poor diet, for example: | ||
| + | *** Swine fed unsupplemented cereal grain | ||
| + | *** Dogs and cats fed all-meat diets | ||
| + | *** Horses fed bran | ||
| + | **** In this case, nutritional hyperparathyroidism is known as "bran disease". | ||
| + | =====Pathogenesis===== | ||
| + | * Pathogenesis follows low calcium/high phosphate diets. | ||
| + | ** These lead to decreased serum calcium levels, stimulating [[Calcium#Parathyroid Hormone (PTH)|PTH]] release. | ||
| + | ** The increase in PTH gives an increase in bone resorption, causing pathology. | ||
| − | == | + | =====Pathology===== |
| − | [[ | + | * '''Gross''' |
| − | [[Image: | + | ** Severe cases may show: |
| − | + | *** Maxillary and mandibular swelling | |
| − | [[Image:Renal_osteodystrophy.jpg|thumb|right| | + | *** [[:Category:Teeth - Anatomy & Physiology|Teeth]] lost or buried in soft tissue |
| − | + | *** Nasal and frontal bone enlargement, leading to dyspnoea | |
| − | + | *** Long bone fracture | |
| + | *** Detatchment tendons and ligaments | ||
| + | ** Early or less severe cases are characterised by shifting lameness and ill thrift. | ||
| + | * '''Histological''' | ||
| + | ** Osteoclastic resorption | ||
| + | ** Fibrous replacement | ||
| + | =====Metabolic Bone Disease===== | ||
| + | * Metabolic bone disease affects lizards in captivity, particularly young green iguanas | ||
| + | * The condition is caused by: | ||
| + | ** Dietary deficiency of calcium and vitamin D | ||
| + | *** For example, due to poor lighting (which diminishes viatmin D production). | ||
| + | ** Dietary excess of phosphorus | ||
| + | ** Certain toxicities | ||
| + | ** Diseases of the kidneys, [[Liver - Anatomy & Physiology|liver]] or parathyroid | ||
| + | *** This aetiology is rare | ||
| + | * Clinical signs include: | ||
| + | ** Lethargy | ||
| + | ** Inability to support weight | ||
| + | ** Rounded skull | ||
| + | ** Spontaneous fractures | ||
| + | ** Adult animals also show signs of [[Hypocalcaemia|hypocalcaemia]] | ||
| + | * The skeleton shows reduced density on radiography. | ||
| + | ====Renal Hyperparathyroidism==== | ||
| + | * Renal Hyerparathyroidism is mostly seen in the dog as an expression of chronic renal disease. | ||
| + | =====Pathogenesis===== | ||
| + | [[Image:renalhyperparathyroidism.jpg|thumb|right|100px|Parathyroid hyperplasia in renal hyperparathyroidism. Image courtesy of Biomed Archive.]] | ||
| + | # Chronic renal disease results in reduced glomerular filtration. | ||
| + | # As glomerular filtration is reduced, phosphate is retained. Chronic renal failure also causes inadequate vitamin D production in the kidneys. | ||
| + | # Hyperphosphataemia develops due to phosphate retention. | ||
| + | #* Hypocalcaemia also occurs, as high levels of phosphate depress calcium levels. | ||
| + | # PTH is released in an attempt to maintain the correct blood calcium:phosphorous ratio. This can have several effects: | ||
| + | #* Parathyroid hyperplasia | ||
| + | #** I.e. '''renal secondary hyperparathyroidism'''. | ||
| + | #* Soft tissue mineralisation | ||
| + | #** Particularly seen in dogs | ||
| + | #** Calcium is commonly deposited in the subpleural connective tissue of the intercostal spaces. | ||
| + | #** Calcification also occurs in other sites, e.g. [[Monogastric Stomach - Anatomy & Physiology|stomach]] wall, lungs, kidneys. | ||
| + | #* Increased bone resorption | ||
| + | #** This causes fibrous osteodystrophy, or "rubber jaw". | ||
| + | =====Pathology===== | ||
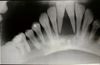
| + | [[Image:Renal_osteodystrophy.jpg|thumb|right|100px|"Rubber jaw" in renal osteodystrophy. Image courtesy of Biomed Archive.]] | ||
| + | * Pathology seen in renal hyperparathyroidism is very similar to that seen in nutritional hyperparathyroidism. | ||
| + | * '''Gross''' | ||
| + | ** The major gross presentation is a fibrous osetodystrophy, or rubber jaw. | ||
| + | *** The maxillae and mandible appear swollen. | ||
| + | *** Radiographically, bone shows reduced density, and [[:Category:Teeth - Anatomy & Physiology|teeth]] hence appear embedded in soft tissue. | ||
| + | *** However, only a few cases of chronic renal disease show such severe bone lesions. | ||
| + | ** Other lesions may also be seen. | ||
| + | *** Intercostal muscles may be calcified. | ||
| + | *** Bone marrow lesions may cause anaemia. | ||
| + | *** The lung may show oedema, and have calcified alveolar walls. | ||
| + | * '''Histological''' | ||
| + | ** Osteoclastic resorption | ||
| + | ** Fibrous replacement | ||
| − | |||
| + | ==From musculoskeletal== | ||
| − | + | *Can arise in a number of ways but single common factor is elevated PTH | |
| + | *Results in increased resorption of bone and replacement by fibrous connective tissue | ||
| − | + | =====<u>'''Primary hyperparathyroidism'''</u>===== | |
| − | + | *This is increased production of PTH not related to calcium or phosphorus levels | |
| + | *Due to parathyroid neoplasia or bilateral idiopathic parathyroid hyperplasia | ||
| + | *Rare | ||
| − | == | + | =====<u>'''Secondary hyperparathyroidism'''</u>===== |
| − | |||
| − | ''' | + | *Regardless of pathogenesis, the result is: |
| + | **Increased osteoclastic resorption of bone and deposition of fibro-osteoid matrix that fails to mineralise | ||
| + | **Flat bones of the skull swell, including maxillary and nasal bones | ||
| + | **Long bones become soft with thin cortices which fracture easily | ||
| + | [[Image:Renal osteodystrophy.jpg|right|thumb|100px|<small><center>Renal osteodystrophy (Image sourced from Bristol Biomed Image Archive with permission)</center></small>]] | ||
| + | *'''Renal hyperparathyroidism''' | ||
| + | **Pathogenesis: | ||
| + | ***[[Chronic Renal Failure|Chronic renal failure]] | ||
| + | ****-> Retention of phosphate (due to reduced glomerular filtration) and inadequate production of vitamin D by kidneys | ||
| + | *****-> Hyperphosphataemia and hypocalcaemia (high P depresses Ca) | ||
| + | ******-> Increased PTH output | ||
| + | *******-> Increased bone resorption | ||
| + | ********-> '''Fibrous osteodystrophy''' - increased osteoclastic resorption of cancellous and cortical bone + proliferation of fibrous tissue | ||
| + | **Mainly in dogs | ||
| + | **Affects whole skeleton but mainly skull | ||
| + | **Bones soft and pliable | ||
| + | **Canine teeth easily removed - rubber jaw | ||
| + | **Microscopically - ''Osteodystrophia fibrosa'' (above = fibrous osteodystrophy) +/- [[Osteomalacia|osteomalacia]] | ||
| − | |||
| − | |||
| − | + | *'''Nutritional hyperparathyroidism''' (nutritional osteodystrophy) | |
| + | **Also called '''fibrous osteodystrophy, “rubber jaw”''' or '''“bran disease”''' | ||
| + | **More common in young, fast-growing animals | ||
| + | **Pathogenesis: | ||
| + | ***Low calcium / high phosphate diets | ||
| + | ****-> Decreased calcium levels in serum | ||
| + | *****-> Parathyroid gland stimulated (may become enlarged) | ||
| + | ******-> Increased PTH | ||
| + | *******-> Increased bone resorption | ||
| + | **Caused by poor diet | ||
| + | ***Cattle and sheep - usually mild disease | ||
| + | ***'''Swine''' fed un-supplemented cereal grain, usually mild disease | ||
| + | ***'''Dogs/cats''' fed all-meat or offal diets (Ca:P often as high as 1:20) | ||
| + | ****Few weeks after weaning | ||
| + | ****Provision of calcium alone correct the problem | ||
| + | ****Very brittle bones -> sponataneous fractures | ||
| + | ****Extreme porosity of the whole skeleton on radioghraphs | ||
| + | ***'''Horses''' fed bran | ||
| + | ****Very susceptible to high phosphorus diet | ||
| + | ****Any time after weaning, susceptibility declines after seventh year | ||
| + | ****Early signs: | ||
| + | *****Mild changes of gait | ||
| + | *****Stiffness | ||
| + | *****Transient shifting lameness | ||
| + | ****Advanced signs: | ||
| + | *****Swelling of mandible and maxilla - 'Big head' | ||
| + | *****Dyspnoea caused by swelling of nasal and frontal bones | ||
| + | *****Teeth lost or buried in softened jaw | ||
| + | *****Fractures from mild trauma | ||
| + | *****Detached tendons and ligaments | ||
| + | *****Histologically: | ||
| + | ******Marked loss of bone | ||
| + | ******Replacement by proliferative tissue | ||
| + | ****Often called '''''Osteodystrophia fibrosa''''' | ||
| − | |||
| − | |||
| − | + | [[Category:Bones - Metabolic Pathology]] | |
| − | + | [[Category:Parathyroid Glands - Pathology]] | |
| − | + | [[Category:To Do - Clinical]] | |
| − | + | [[Category:To Do - Steph]] | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Revision as of 14:11, 26 July 2011
Primary
- Primary hyperparathyroidism is caused by glandular hyperplasia or neoplasia.
- Rare.
Secondary
- Secondary hyperparathyroidism causes fibrous osteodystrophy or "rubber jaw".
- In secondary hyperparathyroidism, the gland is overactive due to another condition coexisting in the body, rather than a primary parathyroid gland defect.
- There are two common forms of secondary hyperparathyroisism:
- Both forms result in increased osteoclastic resorption of bone and deposition of fibro-osteoid matrix that fails to mineralise.
- Flat bones of the skull swell.
- Fibrous tissue is seen around the tooth roots.
- Bone softens in adult animals.
- This is what gives rise to the term "rubber jaw".
- Long bones become soft with thin cortices.
- These fracture easily.
Nutritional Hyperparathyroidism
- Nutritional hyperparathyroidism is also known as nutritional osteodystrophy.
- This occurs most commonly in:
- Young, fast-growing animals
- Animals with a poor diet, for example:
- Swine fed unsupplemented cereal grain
- Dogs and cats fed all-meat diets
- Horses fed bran
- In this case, nutritional hyperparathyroidism is known as "bran disease".
Pathogenesis
- Pathogenesis follows low calcium/high phosphate diets.
- These lead to decreased serum calcium levels, stimulating PTH release.
- The increase in PTH gives an increase in bone resorption, causing pathology.
Pathology
- Gross
- Severe cases may show:
- Maxillary and mandibular swelling
- Teeth lost or buried in soft tissue
- Nasal and frontal bone enlargement, leading to dyspnoea
- Long bone fracture
- Detatchment tendons and ligaments
- Early or less severe cases are characterised by shifting lameness and ill thrift.
- Severe cases may show:
- Histological
- Osteoclastic resorption
- Fibrous replacement
Metabolic Bone Disease
- Metabolic bone disease affects lizards in captivity, particularly young green iguanas
- The condition is caused by:
- Dietary deficiency of calcium and vitamin D
- For example, due to poor lighting (which diminishes viatmin D production).
- Dietary excess of phosphorus
- Certain toxicities
- Diseases of the kidneys, liver or parathyroid
- This aetiology is rare
- Dietary deficiency of calcium and vitamin D
- Clinical signs include:
- Lethargy
- Inability to support weight
- Rounded skull
- Spontaneous fractures
- Adult animals also show signs of hypocalcaemia
- The skeleton shows reduced density on radiography.
Renal Hyperparathyroidism
- Renal Hyerparathyroidism is mostly seen in the dog as an expression of chronic renal disease.
Pathogenesis
- Chronic renal disease results in reduced glomerular filtration.
- As glomerular filtration is reduced, phosphate is retained. Chronic renal failure also causes inadequate vitamin D production in the kidneys.
- Hyperphosphataemia develops due to phosphate retention.
- Hypocalcaemia also occurs, as high levels of phosphate depress calcium levels.
- PTH is released in an attempt to maintain the correct blood calcium:phosphorous ratio. This can have several effects:
- Parathyroid hyperplasia
- I.e. renal secondary hyperparathyroidism.
- Soft tissue mineralisation
- Particularly seen in dogs
- Calcium is commonly deposited in the subpleural connective tissue of the intercostal spaces.
- Calcification also occurs in other sites, e.g. stomach wall, lungs, kidneys.
- Increased bone resorption
- This causes fibrous osteodystrophy, or "rubber jaw".
- Parathyroid hyperplasia
Pathology
- Pathology seen in renal hyperparathyroidism is very similar to that seen in nutritional hyperparathyroidism.
- Gross
- The major gross presentation is a fibrous osetodystrophy, or rubber jaw.
- The maxillae and mandible appear swollen.
- Radiographically, bone shows reduced density, and teeth hence appear embedded in soft tissue.
- However, only a few cases of chronic renal disease show such severe bone lesions.
- Other lesions may also be seen.
- Intercostal muscles may be calcified.
- Bone marrow lesions may cause anaemia.
- The lung may show oedema, and have calcified alveolar walls.
- The major gross presentation is a fibrous osetodystrophy, or rubber jaw.
- Histological
- Osteoclastic resorption
- Fibrous replacement
From musculoskeletal
- Can arise in a number of ways but single common factor is elevated PTH
- Results in increased resorption of bone and replacement by fibrous connective tissue
Primary hyperparathyroidism
- This is increased production of PTH not related to calcium or phosphorus levels
- Due to parathyroid neoplasia or bilateral idiopathic parathyroid hyperplasia
- Rare
Secondary hyperparathyroidism
- Regardless of pathogenesis, the result is:
- Increased osteoclastic resorption of bone and deposition of fibro-osteoid matrix that fails to mineralise
- Flat bones of the skull swell, including maxillary and nasal bones
- Long bones become soft with thin cortices which fracture easily
- Renal hyperparathyroidism
- Pathogenesis:
- Chronic renal failure
- -> Retention of phosphate (due to reduced glomerular filtration) and inadequate production of vitamin D by kidneys
- -> Hyperphosphataemia and hypocalcaemia (high P depresses Ca)
- -> Increased PTH output
- -> Increased bone resorption
- -> Fibrous osteodystrophy - increased osteoclastic resorption of cancellous and cortical bone + proliferation of fibrous tissue
- -> Increased bone resorption
- -> Increased PTH output
- -> Hyperphosphataemia and hypocalcaemia (high P depresses Ca)
- -> Retention of phosphate (due to reduced glomerular filtration) and inadequate production of vitamin D by kidneys
- Chronic renal failure
- Mainly in dogs
- Affects whole skeleton but mainly skull
- Bones soft and pliable
- Canine teeth easily removed - rubber jaw
- Microscopically - Osteodystrophia fibrosa (above = fibrous osteodystrophy) +/- osteomalacia
- Pathogenesis:
- Nutritional hyperparathyroidism (nutritional osteodystrophy)
- Also called fibrous osteodystrophy, “rubber jaw” or “bran disease”
- More common in young, fast-growing animals
- Pathogenesis:
- Low calcium / high phosphate diets
- -> Decreased calcium levels in serum
- -> Parathyroid gland stimulated (may become enlarged)
- -> Increased PTH
- -> Increased bone resorption
- -> Increased PTH
- -> Parathyroid gland stimulated (may become enlarged)
- -> Decreased calcium levels in serum
- Low calcium / high phosphate diets
- Caused by poor diet
- Cattle and sheep - usually mild disease
- Swine fed un-supplemented cereal grain, usually mild disease
- Dogs/cats fed all-meat or offal diets (Ca:P often as high as 1:20)
- Few weeks after weaning
- Provision of calcium alone correct the problem
- Very brittle bones -> sponataneous fractures
- Extreme porosity of the whole skeleton on radioghraphs
- Horses fed bran
- Very susceptible to high phosphorus diet
- Any time after weaning, susceptibility declines after seventh year
- Early signs:
- Mild changes of gait
- Stiffness
- Transient shifting lameness
- Advanced signs:
- Swelling of mandible and maxilla - 'Big head'
- Dyspnoea caused by swelling of nasal and frontal bones
- Teeth lost or buried in softened jaw
- Fractures from mild trauma
- Detached tendons and ligaments
- Histologically:
- Marked loss of bone
- Replacement by proliferative tissue
- Often called Osteodystrophia fibrosa