Difference between revisions of "Pulmonary Hypertension"
| (4 intermediate revisions by 3 users not shown) | |||
| Line 19: | Line 19: | ||
==Signalment== | ==Signalment== | ||
| − | Some diseases predispose animals to secondary pulmonary hypertension. Predisposed breeds include brachycephalic dogs (chronic obstructive pulmonary disease); small breeds ([[Mitral Valve | + | Some diseases predispose animals to secondary pulmonary hypertension. Predisposed breeds include brachycephalic dogs (chronic obstructive pulmonary disease); small breeds ([[Degenerative Mitral Valve Disease|mitral endocardiosis]]) and West Highland White Terriers (pulmonary fibrosis). |
| − | |||
== Clinical Signs == | == Clinical Signs == | ||
| Line 35: | Line 34: | ||
:Complete Blood Count will show an eosinophilia if ther is parasitic involvement. (Serology or Fecal Baermann tests would confirm parasitic involvement). | :Complete Blood Count will show an eosinophilia if ther is parasitic involvement. (Serology or Fecal Baermann tests would confirm parasitic involvement). | ||
:Biochemistry would show hyperglobulinemia in chronic inflammation. | :Biochemistry would show hyperglobulinemia in chronic inflammation. | ||
| + | :A biomarker for a pulmonary hypertension is an elevated NT-proBNP. | ||
'''Urinalysis''' may show the presence of proteinuria if systemic disease is present. | '''Urinalysis''' may show the presence of proteinuria if systemic disease is present. | ||
| − | '''Radiography''' is best performed with a DV view. Signs will include | + | '''Radiography''' is best performed with a DV view. Signs will include right atrial and ventricular enlargement, pulmonary arteries enlargement, enlargement of the V. cava caudalis, congested pulmonary veins and signs of pulmonary disease. |
'''Electrocardiography''' may show the presence of right ventricular hypertrophy (deep S-waves) and signs of myocardial hypoxia (ST segment abnormalities). | '''Electrocardiography''' may show the presence of right ventricular hypertrophy (deep S-waves) and signs of myocardial hypoxia (ST segment abnormalities). | ||
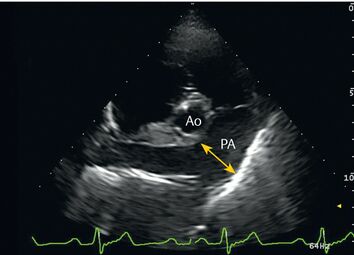
| − | '''Echocardiography''' may be used to calculate pulmonary arterial pressures. It may also show enlargement of the right-side of the heart and enable visualisation of mitral or tricuspid regurgitation. | + | '''Echocardiography''' may be used to calculate pulmonary arterial pressures. It may also show enlargement of the right-side of the heart and enable visualisation of mitral or tricuspid regurgitation.<gallery caption="[[File:Enlarged pulmonary artery.jpg|thumb|354x354px|Enlarged pulmonary artery]]"> |
| − | + | </gallery> | |
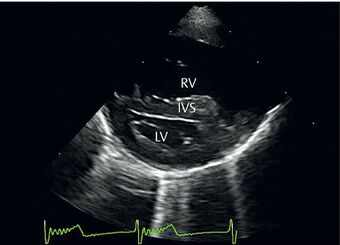
| + | <gallery caption="[[File:Diagnosis of Pulmonary Hypertension.jpg|thumb|340x340px|Enlarged right atrium and ventricle]]"> | ||
| + | </gallery> | ||
== Treatment == | == Treatment == | ||
| Line 67: | Line 69: | ||
[[Category:Lungs_-_Circulatory_Pathology]] [[Category:Vascular_Diseases_-_Dog]] [[Category:Vascular_Diseases_-_Cat]] [[Category:Arterial_Pathology]] [[Category:Expert_Review]] | [[Category:Lungs_-_Circulatory_Pathology]] [[Category:Vascular_Diseases_-_Dog]] [[Category:Vascular_Diseases_-_Cat]] [[Category:Arterial_Pathology]] [[Category:Expert_Review]] | ||
| + | [[Category:Cardiology Section]] | ||
Latest revision as of 13:45, 23 June 2021
Introduction
Hypertension is defined as the pathological elevation of arterial blood pressure.There are two main types of hypertension, systemic hypertension (affects the systemic circulation) and pulmonary hypertension (affects the pulmonary circulation). Blood pressure in veterinary patients is not measured routinely; therefore hypertension is usually only diagnosed after clinical signs become apparent.
Pulmonary hypertension = increase in pulmonary arterial pressure.
There are two types of pulmonary hypertension:
1. Primary pulmonary hypertension = idiopathic pulmonary hypertension (contributing factors: drugs, toxins, genetic predisposition and infections)
2. Secondary pulmonary hypertension = pulmonary hypertension resulting from an identifiable underlying condition
Cor pulmonale = right sided heart failure resulting from pulmonary hypertension.
The hypoxic conditions at high elevations or animals with chronic airway disease contribute to pulmonary hypertension through hypoxia-induced vasoconstriction.
Signalment
Some diseases predispose animals to secondary pulmonary hypertension. Predisposed breeds include brachycephalic dogs (chronic obstructive pulmonary disease); small breeds (mitral endocardiosis) and West Highland White Terriers (pulmonary fibrosis).
Clinical Signs
Clinical signs may vary and also may be disguised by other signs of the underlying, causative disease. There is often signs of right sided heart failure, such as exercise intolerance, dyspnoea, coughing, syncope, cyanosis, abdominal distension and distended jugular veins.
Diagnosis
Physical examination, depending on any underlying conditions, may show a heart murmur (mitral or tricuspid regurgitation), presence of a gallop rhythm, increased lung sounds and splitting of S2 heart sounds (see arrhythmias).
Blood tests:
- Arterial blood gases may show hypoxemia if there are low oxygen conditions.
- Complete Blood Count will show an eosinophilia if ther is parasitic involvement. (Serology or Fecal Baermann tests would confirm parasitic involvement).
- Biochemistry would show hyperglobulinemia in chronic inflammation.
- A biomarker for a pulmonary hypertension is an elevated NT-proBNP.
Urinalysis may show the presence of proteinuria if systemic disease is present.
Radiography is best performed with a DV view. Signs will include right atrial and ventricular enlargement, pulmonary arteries enlargement, enlargement of the V. cava caudalis, congested pulmonary veins and signs of pulmonary disease.
Electrocardiography may show the presence of right ventricular hypertrophy (deep S-waves) and signs of myocardial hypoxia (ST segment abnormalities).
Echocardiography may be used to calculate pulmonary arterial pressures. It may also show enlargement of the right-side of the heart and enable visualisation of mitral or tricuspid regurgitation.
Treatment
Treat the underlying conditions:
- Treat right sided heart failure
- Treat pulmonary thromboembolism with heparin and then warfarin
- Treat chronic obstructive pulmonary disease
Prognosis
Depends on the disease condition causing pulmonary hypertension and the ability to control it. Prognosis is poor when pulmonary drainage is irreversible.
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
Error in widget FBRecommend: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt697944058b4938_03263572 Error in widget google+: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt697944059385e3_66526315 Error in widget TwitterTweet: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt697944059e9950_86663254
|
| WikiVet® Introduction - Help WikiVet - Report a Problem |