Difference between revisions of "Feline Infectious Anaemia"
RebekahMCB (talk | contribs) |
|||
| (37 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
| − | + | {{OpenPagesTop}} | |
| + | {{Summary | ||
| + | |cause = ''Mycoplasma haemofelis'' | ||
| + | |signalment = Male cats with outdoor access | ||
| + | |associated = Feline retroviruses | ||
| + | |differentials = Other causes of anaemia | ||
| + | |diagnosis = PCR, blood smear examination | ||
| + | |treatment = Doxycycline | ||
| + | }} | ||
| + | Also known as: '''''FIA — Haemoplasmosis — Hemoplasmosis'''''; previously known as: ''Haemobartonellosis'' | ||
| − | Caused by: '''''Mycoplasma haemofelis''''' | + | Caused by: '''''Mycoplasma haemofelis (Mhf)''''' (previously known as ''Haemobartonella felis''), '''''Candidatus M. haemominutum (Mhm) — Candidatus M. turicensis (Mtc)''''' |
==Introduction== | ==Introduction== | ||
| − | Feline Infectious Anaemia | + | Feline Infectious Anaemia is a [[Regenerative_and_Non-Regenerative_Anaemias|regenerative anaemia]] of cats caused by '''''Mycoplasma haemofelis''''' (Mhf). The disease occurs worldwide and should be considered as a differential diagnosis for any cat presenting with anaemia. |
==Aetiology== | ==Aetiology== | ||
| − | Mhf is one of a group of organisms known as haemotropic mycoplasmas which infect | + | Mhf is one of a group of organisms known as haemotropic [[Mycoplasmas|mycoplasmas]] which infect many mammalian species. The causative organism was previously called ''Haemobartonella felis'' and thus the disease was known as haemobartonellosis. [[Polymerase_Chain_Reaction|Polymerase chain reaction]] (PCR) assays allowing DNA analysis resulted in the reclassification of the organism as a mycoplasma in 2001<ref name="Niemark">Niemark H, Johansson KE, Rikihisa Y, et al (2001) Proposal to transfer some members of the genera ''Haemobartonella'' and ''Eperythrozoon'' to the genus ''Mycoplasma'' with descriptions of Candidatus ''Mycoplasma haemofelis'', Candidatus ''Mycoplasma haemomuris'', Candidatus ''Mycoplasma haemosuis'' and Candidatus ''Mycoplasma wenyonii'' '''Int J Sys Evol Microbiol 51(3) pp891-9</ref>. Two other haemotropic mycoplasmas (''Candidatus M. haemominutum'' (Mhm) and ''Candidatus M. turicensis'' (Mtc)) have also been identified in cats but appear to be less pathogenic<ref name="Sykes">Sykes, JE (2010) Feline Hemotropic Mycoplasmas '''Vet Clinics of North America: Small Animal Practice''' pp. 1157-1170</ref>. |
| + | |||
| + | |||
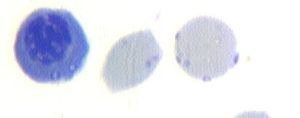
| + | Mhf can vary in shape from cocci to rods and is sometimes present as chains of organisms on the surface of [[Erythrocyte|erythrocytes]]. | ||
| + | [[File:M haemofelis2.jpg|thumb|''Mycoplasma haemofelis'' on the surface of an erythrocyte]] | ||
| − | + | ==Transmission== | |
| + | The mode of transmission of Mhf is poorly understood. Several possibilities have been proposed but none have been able to be reliably demonstrated. These include: | ||
| + | * Biting and fighting activities. Infection by this route has not been able to be demonstrated experimentally. | ||
| + | *[[Fleas|Fleas]]. The fact that Mhf infection can be prevalent in areas where fleas are uncommon makes this less likely.<ref name="Jensen"> Jensen WA, Lappin MR, Kamkar S et al (2001) Use of a polymerase chain reaction assay to detect and differentiate two strains of ''Haemobartonella felis'' in naturally infected cats. '''Am J Vet Res''' 62(4):604-8 </ref> | ||
| + | *[[Arthropods|Arthropods]]. Geographic variation in rates of Mhf infection does exist and could be due to transmission by an arthropod. <ref name="Willi">Willi B, Boretti FS, Baumgartner C et al (2006) Prevalence, risk factor analysis and follow-up of infections caused by three feline haemoplasma species in Switzerland. '''J Clin Microbiol''' 44(3):961-9</ref> | ||
| − | + | ||
| + | As transmission has been shown to occur through blood transfusion due to the ability of the organism to survive in stored blood products for up to 7 days <ref name="Gary">Gary AT, Richmond HL, Tasker S etal (2006) Survival of ''Mycoplsma haemofelis'' and ''Candidatus'' Mycolplasma haemominitum in blood of cats used for transfusions '''J Feline Med Surg''' 8(5):321-6</ref>, it is recommended that blood donors be screened.<ref name="Wardrop">Wardrop J, Reine N, Birkenheuer A et al (2005) Canine and feline blood donor screening for infectious disease '''J Vet Intern Med''' 19(1) pp.135-42.</ref> | ||
==Signalment== | ==Signalment== | ||
| − | The major group at risk for Mhf infection are young male cats who spend time outdoors. In many areas of the world an association has been shown between Mhf and retroviral infections< | + | The major group at risk for Mhf infection are young male cats who spend time outdoors. In many areas of the world an association has been shown between Mhf and [[Retroviridae|retroviral infections]]<ref name="Sykes" />. It has been demonstrated that cats infected with Mhf and [[Feline_Leukaemia_Virus|feline leukaemia virus (FeLV)]] are likely to develop more severe anaemia that cats infected only with Mhf <ref name="Wardrop"></ref>. |
==Pathogenesis== | ==Pathogenesis== | ||
| − | The pathogenesis of Mhf is not fully understood. It is thought that the presence of the parasite on the surface of the | + | The pathogenesis of Mhf is not fully understood. It is thought that the presence of the parasite on the surface of the erythrocytes may induce [[Immunoglobulins_-_Overview|antibody production]]<ref name="Hagiwara"></ref>, resulting in [[Regenerative_and_Non-Regenerative_Anaemias#Haemolysis|haemolysis]] which is primarily extravascular. The haemolysis may be due to direct damage of erythrocytes by the organism or as a result of the antibodies produced by the infected animal <ref name="Wardrop"></ref>. |
| + | |||
| + | Cats can produce an immune response which results in the disappearance of organisms from the blood. Production of uninfected erythrocytes can then result in an increase in [[haematocrit]]. | ||
| + | |||
| + | It is thought that recovered cats can become subclinical carriers, with the potential for the disease to recrudesce if the animal is in a stressed state eg pregnancy, illness.<ref name = "Harvey">Harvey JW and Gaskin JM (1978)Feline haemobartonellosis;attempts to induce relapses of clinical disease in chronically infected cats.'''J Am Anim Hosp Assoc'''14:453</ref> | ||
| + | |||
| + | [[File:M haemofelis.jpg|thumb|''Mycoplasma haemofelis'' on the surface of blood cells]] | ||
==Clinical signs== | ==Clinical signs== | ||
| − | Infected cats most commonly present for lethargy and decreased appetite. Physical examination findings are non-specific and can include signs of anaemia, such as mucous membrane pallor, tachypnoea and tachycardia, pyrexia, and occasionally | + | Infected cats most commonly present for lethargy and decreased appetite. Physical examination findings are non-specific and can include signs of anaemia, such as mucous membrane pallor, tachypnoea and tachycardia, pyrexia, and occasionally splenomegaly and [[Icterus|jaundice]]. Pyrexia is frequently intermittent and spikes when parasite numbers are highest <ref name="Wardrop"></ref>. The anaemia can be severe and rapidly fatal in some cases. |
==Differential diagnosis== | ==Differential diagnosis== | ||
| − | There are multiple causes of both regenerative and non-regenerative anaemia in cats which must be considered as differential diagnoses | + | There are multiple causes of both [[Regenerative and Non-Regenerative Anaemias|regenerative and non-regenerative anaemia]] in cats which must be considered as differential diagnoses. |
For cats showing signs of regeneration, causes of blood loss or haemolysis must be considered: | For cats showing signs of regeneration, causes of blood loss or haemolysis must be considered: | ||
| − | *primary immune-mediated haemolytic anaemia | + | *[[Immune_Mediated_Haemolytic_Anaemia|primary immune-mediated haemolytic anaemia]] |
| − | *Heinz body haemolytic anaemia (onions, garlic,propofol) | + | *Heinz body haemolytic anaemia (onions, garlic, [[propofol]]) |
| − | *other infectious causes such as | + | *other infectious causes such as [[Babesia|''Babesia felis'']] and [[Cytauxzoon#Cytauxzoon_felis|''Cytauxzoon felis'']] |
| − | *neoplasia | + | *[[Neoplasia_-_Pathology|neoplasia]] |
| Line 39: | Line 63: | ||
*neoplasia | *neoplasia | ||
*chronic inflammatory conditions | *chronic inflammatory conditions | ||
| − | *underlying conditions such as diabetes mellitus and renal disease | + | *underlying conditions such as [[Diabetes_Mellitus|diabetes mellitus]] and [[Chronic_Renal_Failure|renal disease]] |
| − | *Feline Immunodeficiency Virus (FIV) and FeLV infections | + | *[[FIV|Feline Immunodeficiency Virus(FIV)]] and [[FeLV]] infections |
| − | *bone marrow diseases | + | *[[Regenerative_and_Non-Regenerative_Anaemias#Failure_of_the_bone_marrow_stem_cells_to_produce_erythroid_cells|bone marrow diseases]] |
| − | |||
==Diagnosis== | ==Diagnosis== | ||
| − | The most commmon findings from complete blood counts from cats with Mhf infections are a | + | The most commmon findings from complete blood counts from cats with Mhf infections are a '''macrocytic, hypochromic regenerative anaemia'''. [[Reticulocyte|Reticulocytes]] and [[Howell-Jolly Bodies|Howell-Jolly bodies]] may be identified on cytologic examination. |
| − | Mhf infection can be | + | Mhf infection can be definitively diagnosed by identification of organisms on a blood smear, appearing as cocci or rods and sometimes forming short chains of organisms. However, examination of a single blood smear is less than 50% sensitive <ref name="Hagiwara"> Hagiwara, MK (2009) Anemia in Cats: Is It Mycoplasma? '''Proceedings of the 34th World Small Animal Veterinary Congress'''</ref> as the animal's immune response causes organisms to disappear from the blood stream for several days, often to reappear a few days later. One study found that smears should be examined every four days over a minimum of three four day cycles<ref name="Ettinger>Ettinger, S.J, Feldman, E.C. (2005) Textbook of Veterinary Internal Medicine (6th edition, volume 2) W.B. Saunders Company</ref>, making it possible to have eight days between presentation and diagnosis. It also has the potential for misidentification of organisms. |
| − | The gold standard for diagnosis of Mhf infection is polymerase chain reaction (PCR), which detects the 16S RNA gene. The test is widely available through veterinary diagnostic laboratories. There are two types of PCR tests; conventional PCR which uses the presence or absence of bands on a gel to assess infection, and real-time PCR assays which uses fluoresence to mark a segment of DNA unique to the organism, making it highly sensitive and species-specific and thus the test of choice<ref name="Sykes"></ref>. Treatment with antimicrobials may result in false negatives on PCR so collecting before beginning therapy is | + | The gold standard for diagnosis of Mhf infection is polymerase chain reaction (PCR), which detects the 16S RNA gene. The test is widely available through veterinary diagnostic laboratories. There are two types of PCR tests; conventional PCR which uses the presence or absence of bands on a gel to assess infection, and real-time PCR assays which uses fluoresence to mark a segment of DNA unique to the organism, making it highly sensitive and species-specific and thus the test of choice <ref name="Sykes"></ref>. Treatment with antimicrobials may result in false negatives on PCR so collecting before beginning therapy is preferable. |
==Treatment== | ==Treatment== | ||
| − | The treatment of choice is doxycycline | + | The treatment of choice for Mhf infection is [[Tetracyclines|doxycycline]] for at least two weeks. Only cats who are anaemic and have clinical signs and laboratory results consistent with haemoplasmosis should be treated as the drug does not reliably eliminate the organism<ref name="Sykes"></ref>. For this reason a PCR-positive cat may not become negative despite treatment and therapy cannot be used to ensure blood donor cats are free from infection. |
| − | [[Fluoroquinolones|Enrofloxacin]] is also a | + | [[Fluoroquinolones|Enrofloxacin]] is also an effective treatment <ref name="Tasker">Tasker, S, Helps CR, Day MJ et al.(2004) Use of a Taqman PCR to determine the response to ''Mycoplasma haemofelis'' infection to antibiotic treatment. '''JMicrobiol Methods''' 56(1):63-71</ref> but is a second choice due to the risk of acute retinal damage in cats. |
A [[:Category:Transfusion Medicine|blood transfusion]] may also be required in cases of severe anaemia. | A [[:Category:Transfusion Medicine|blood transfusion]] may also be required in cases of severe anaemia. | ||
| − | + | Antimicrobial therapy and blood transfusions should be initiated before PCR results are known, as this may take several days. In cats testing negative for Mhf and failing to respond to therapy, alternative diagnoses should be considered. | |
| − | + | The use of [[Steroids|glucocorticoids]] to suppress immune-mediated damage to erythrocytes has been suggested. However, as this treatment may cause reactivation of a latent infection it is recommended that they only be used in cats not responding to doxycycline and/or for whom there is no definitive diagnosis. | |
==Prognosis== | ==Prognosis== | ||
| − | + | Prognosis for infected cats is related to the severity of the anaemia at presentation. If an animal survives the initial anaemia prognosis for clinical recovery is good. However, antibiotics do not clear the infection so many cats become carriers of the organism. Affected animals may also have intercurrent disease, such as retroviral infections, which will also affect the prognosis. | |
{{Learning | {{Learning | ||
| Line 76: | Line 99: | ||
[http://www.cabi.org/cabdirect/FullTextPDF/2007/20073119573.pdf ''' Bartonellosis and hemoplasmosis in dogs and cats: emerging issues.''' Lappin, M. R.; The North American Veterinary Conference, Gainesville, USA, Small animal and exotics. Proceedings of the North American Veterinary Conference, Volume 21, Orlando, Florida, USA, 2007, 2007, pp 629-631] | [http://www.cabi.org/cabdirect/FullTextPDF/2007/20073119573.pdf ''' Bartonellosis and hemoplasmosis in dogs and cats: emerging issues.''' Lappin, M. R.; The North American Veterinary Conference, Gainesville, USA, Small animal and exotics. Proceedings of the North American Veterinary Conference, Volume 21, Orlando, Florida, USA, 2007, 2007, pp 629-631] | ||
| + | |Vetstream = [https://www.vetstream.com/felis/Content/Disease/dis60170 Feline infectious anemia] | ||
}} | }} | ||
| − | == | + | ==References== |
<references/> | <references/> | ||
| − | == | + | ==Extra references== |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Merck & Co (2008) '''The Merck Veterinary Manual''' (Eighth Edition) ''Merial'' | Merck & Co (2008) '''The Merck Veterinary Manual''' (Eighth Edition) ''Merial'' | ||
| − | {{ | + | {{Rebekah Brown |
| − | [[Category:Anaemia]] | + | |date = July 3, 2012 }} |
| + | |||
| + | {{OpenPages}} | ||
| + | |||
| + | [[Category:Anaemia|5]] | ||
[[Category:Lymphoreticular and Haematopoietic Diseases - Cat]][[Category:Cat Bacteria]] | [[Category:Lymphoreticular and Haematopoietic Diseases - Cat]][[Category:Cat Bacteria]] | ||
[[Category:Expert_Review - Small Animal]] | [[Category:Expert_Review - Small Animal]] | ||
Latest revision as of 10:15, 8 March 2022
| Summary | |
|---|---|
| Cause: | Mycoplasma haemofelis |
| Signalment: | Male cats with outdoor access |
| Associated conditions: | Feline retroviruses |
| Differential diagnoses: | Other causes of anaemia |
| Diagnosis: | PCR, blood smear examination |
| Treatment: | Doxycycline |
Also known as: FIA — Haemoplasmosis — Hemoplasmosis; previously known as: Haemobartonellosis
Caused by: Mycoplasma haemofelis (Mhf) (previously known as Haemobartonella felis), Candidatus M. haemominutum (Mhm) — Candidatus M. turicensis (Mtc)
Introduction
Feline Infectious Anaemia is a regenerative anaemia of cats caused by Mycoplasma haemofelis (Mhf). The disease occurs worldwide and should be considered as a differential diagnosis for any cat presenting with anaemia.
Aetiology
Mhf is one of a group of organisms known as haemotropic mycoplasmas which infect many mammalian species. The causative organism was previously called Haemobartonella felis and thus the disease was known as haemobartonellosis. Polymerase chain reaction (PCR) assays allowing DNA analysis resulted in the reclassification of the organism as a mycoplasma in 2001[1]. Two other haemotropic mycoplasmas (Candidatus M. haemominutum (Mhm) and Candidatus M. turicensis (Mtc)) have also been identified in cats but appear to be less pathogenic[2].
Mhf can vary in shape from cocci to rods and is sometimes present as chains of organisms on the surface of erythrocytes.
Transmission
The mode of transmission of Mhf is poorly understood. Several possibilities have been proposed but none have been able to be reliably demonstrated. These include:
- Biting and fighting activities. Infection by this route has not been able to be demonstrated experimentally.
- Fleas. The fact that Mhf infection can be prevalent in areas where fleas are uncommon makes this less likely.[3]
- Arthropods. Geographic variation in rates of Mhf infection does exist and could be due to transmission by an arthropod. [4]
As transmission has been shown to occur through blood transfusion due to the ability of the organism to survive in stored blood products for up to 7 days [5], it is recommended that blood donors be screened.[6]
Signalment
The major group at risk for Mhf infection are young male cats who spend time outdoors. In many areas of the world an association has been shown between Mhf and retroviral infections[2]. It has been demonstrated that cats infected with Mhf and feline leukaemia virus (FeLV) are likely to develop more severe anaemia that cats infected only with Mhf [6].
Pathogenesis
The pathogenesis of Mhf is not fully understood. It is thought that the presence of the parasite on the surface of the erythrocytes may induce antibody production[7], resulting in haemolysis which is primarily extravascular. The haemolysis may be due to direct damage of erythrocytes by the organism or as a result of the antibodies produced by the infected animal [6].
Cats can produce an immune response which results in the disappearance of organisms from the blood. Production of uninfected erythrocytes can then result in an increase in haematocrit.
It is thought that recovered cats can become subclinical carriers, with the potential for the disease to recrudesce if the animal is in a stressed state eg pregnancy, illness.[8]
Clinical signs
Infected cats most commonly present for lethargy and decreased appetite. Physical examination findings are non-specific and can include signs of anaemia, such as mucous membrane pallor, tachypnoea and tachycardia, pyrexia, and occasionally splenomegaly and jaundice. Pyrexia is frequently intermittent and spikes when parasite numbers are highest [6]. The anaemia can be severe and rapidly fatal in some cases.
Differential diagnosis
There are multiple causes of both regenerative and non-regenerative anaemia in cats which must be considered as differential diagnoses.
For cats showing signs of regeneration, causes of blood loss or haemolysis must be considered:
- primary immune-mediated haemolytic anaemia
- Heinz body haemolytic anaemia (onions, garlic, propofol)
- other infectious causes such as Babesia felis and Cytauxzoon felis
- neoplasia
Major differential diagnoses for cats with non-regenerative anaemia include:
- neoplasia
- chronic inflammatory conditions
- underlying conditions such as diabetes mellitus and renal disease
- Feline Immunodeficiency Virus(FIV) and FeLV infections
- bone marrow diseases
Diagnosis
The most commmon findings from complete blood counts from cats with Mhf infections are a macrocytic, hypochromic regenerative anaemia. Reticulocytes and Howell-Jolly bodies may be identified on cytologic examination.
Mhf infection can be definitively diagnosed by identification of organisms on a blood smear, appearing as cocci or rods and sometimes forming short chains of organisms. However, examination of a single blood smear is less than 50% sensitive [7] as the animal's immune response causes organisms to disappear from the blood stream for several days, often to reappear a few days later. One study found that smears should be examined every four days over a minimum of three four day cycles[9], making it possible to have eight days between presentation and diagnosis. It also has the potential for misidentification of organisms.
The gold standard for diagnosis of Mhf infection is polymerase chain reaction (PCR), which detects the 16S RNA gene. The test is widely available through veterinary diagnostic laboratories. There are two types of PCR tests; conventional PCR which uses the presence or absence of bands on a gel to assess infection, and real-time PCR assays which uses fluoresence to mark a segment of DNA unique to the organism, making it highly sensitive and species-specific and thus the test of choice [2]. Treatment with antimicrobials may result in false negatives on PCR so collecting before beginning therapy is preferable.
Treatment
The treatment of choice for Mhf infection is doxycycline for at least two weeks. Only cats who are anaemic and have clinical signs and laboratory results consistent with haemoplasmosis should be treated as the drug does not reliably eliminate the organism[2]. For this reason a PCR-positive cat may not become negative despite treatment and therapy cannot be used to ensure blood donor cats are free from infection.
Enrofloxacin is also an effective treatment [10] but is a second choice due to the risk of acute retinal damage in cats.
A blood transfusion may also be required in cases of severe anaemia.
Antimicrobial therapy and blood transfusions should be initiated before PCR results are known, as this may take several days. In cats testing negative for Mhf and failing to respond to therapy, alternative diagnoses should be considered.
The use of glucocorticoids to suppress immune-mediated damage to erythrocytes has been suggested. However, as this treatment may cause reactivation of a latent infection it is recommended that they only be used in cats not responding to doxycycline and/or for whom there is no definitive diagnosis.
Prognosis
Prognosis for infected cats is related to the severity of the anaemia at presentation. If an animal survives the initial anaemia prognosis for clinical recovery is good. However, antibiotics do not clear the infection so many cats become carriers of the organism. Affected animals may also have intercurrent disease, such as retroviral infections, which will also affect the prognosis.
| Feline Infectious Anaemia Learning Resources | |
|---|---|
To reach the Vetstream content, please select |
Canis, Felis, Lapis or Equis |
 Test your knowledge using flashcard type questions |
Small Animal Emergency and Critical Care Medicine Q&A 12 |
 Search for recent publications via CAB Abstract (CABI log in required) |
Mycoplasma haemofelis publications |
 Full text articles available from CAB Abstract (CABI log in required) |
Diagnosis and management of Hemoplasma infections. Lappin, M. R.; The North American Veterinary Conference, Gainesville, USA, Small animal and exotics. Proceedings of the North American Veterinary Conference, Orlando, Florida, USA, 17-21 January, 2009, 2009, pp 655-656, 23 ref. |
References
- ↑ Niemark H, Johansson KE, Rikihisa Y, et al (2001) Proposal to transfer some members of the genera Haemobartonella and Eperythrozoon to the genus Mycoplasma with descriptions of Candidatus Mycoplasma haemofelis, Candidatus Mycoplasma haemomuris, Candidatus Mycoplasma haemosuis and Candidatus Mycoplasma wenyonii Int J Sys Evol Microbiol 51(3) pp891-9
- ↑ 2.0 2.1 2.2 2.3 Sykes, JE (2010) Feline Hemotropic Mycoplasmas Vet Clinics of North America: Small Animal Practice pp. 1157-1170
- ↑ Jensen WA, Lappin MR, Kamkar S et al (2001) Use of a polymerase chain reaction assay to detect and differentiate two strains of Haemobartonella felis in naturally infected cats. Am J Vet Res 62(4):604-8
- ↑ Willi B, Boretti FS, Baumgartner C et al (2006) Prevalence, risk factor analysis and follow-up of infections caused by three feline haemoplasma species in Switzerland. J Clin Microbiol 44(3):961-9
- ↑ Gary AT, Richmond HL, Tasker S etal (2006) Survival of Mycoplsma haemofelis and Candidatus Mycolplasma haemominitum in blood of cats used for transfusions J Feline Med Surg 8(5):321-6
- ↑ 6.0 6.1 6.2 6.3 Wardrop J, Reine N, Birkenheuer A et al (2005) Canine and feline blood donor screening for infectious disease J Vet Intern Med 19(1) pp.135-42.
- ↑ 7.0 7.1 Hagiwara, MK (2009) Anemia in Cats: Is It Mycoplasma? Proceedings of the 34th World Small Animal Veterinary Congress
- ↑ Harvey JW and Gaskin JM (1978)Feline haemobartonellosis;attempts to induce relapses of clinical disease in chronically infected cats.J Am Anim Hosp Assoc14:453
- ↑ Ettinger, S.J, Feldman, E.C. (2005) Textbook of Veterinary Internal Medicine (6th edition, volume 2) W.B. Saunders Company
- ↑ Tasker, S, Helps CR, Day MJ et al.(2004) Use of a Taqman PCR to determine the response to Mycoplasma haemofelis infection to antibiotic treatment. JMicrobiol Methods 56(1):63-71
Extra references
Merck & Co (2008) The Merck Veterinary Manual (Eighth Edition) Merial
| This article has been provided and expert reviewed by Rebekah Brown BAnimSci BVSc DipVetClinStuds Date reviewed: July 3, 2012 |
Error in widget FBRecommend: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt69551c6bedac25_17639119 Error in widget google+: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt69551c6bf2a8e3_35812824 Error in widget TwitterTweet: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt69551c6c03a872_22140630
|
| WikiVet® Introduction - Help WikiVet - Report a Problem |