Difference between revisions of "Pancreas - Anatomy & Physiology"
(→Links) |
|||
| (44 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
| − | + | <big><center>[[Alimentary - Anatomy & Physiology|'''BACK TO ALIMENTARY - ANATOMY & PHYSIOLOGY''']]</center></big> | |
| + | |||
==Introduction== | ==Introduction== | ||
| + | The pancreas is a tubuloalveolar gland and has '''exocrine''' and '''[[Endocrine System - Anatomy & Physiology|endocrine]]''' tissues. The '''exocrine''' part secretes pancreatic juice; a solution containing enzymes for carbohydrate, protein and triacylglycerol digestion. Pancreatic juice drains into the [[Small Intestine - Anatomy & Physiology|small intestine]] where it is functional. It is the larger of the two parts of the pancreas. The '''endocrine''' part secretes hormones for the regulation of blood glucose concentration, including insulin, glucagon and somatostatin. The functional units of the exocrine part are the ''islets of Langerhans''. | ||
| − | |||
===Development=== | ===Development=== | ||
| − | The pancreas develops from endoderm, except for the connective tissue which develops from splanchnic mesoderm. Development begins with evaginations of the digestive tube caudal to the [[ | + | The pancreas develops from endoderm, except for the connective tissue which develops from splanchnic mesoderm. Development begins with evaginations of the digestive tube caudal to the [[Forestomach - Anatomy & Physiology|stomach]]. Two pancreatic buds form, one in the dorsal mesogastrium and one in the ventral mesogastrium. Some epithelial cells lose their connections to the developing duct system of the exocrine pancreas and develop into the islets of Langerhans of the endocrine pancreas. As the [[Forestomach - Anatomy & Physiology|stomach]] rotates, the ventral bud moves to become more dorsal. The two buds then fuse; the left lobe is derived from the dorsal bud and the right lobe from the ventral bud. The duct of the ventral lobe ('''pancreatic duct''') joins with the bile duct to form the '''common bile duct''' which opens into the duodenum at the '''major duodenal papilla'''. The duct of the dorsal lobe ('''accessory duct''') enters the [[Duodenum - Anatomy & Physiology|duodenum]] at the '''minor duodenal papilla'''. There is [[#Species Differences|species variation]] in the persistance of each duct. |
==Structure== | ==Structure== | ||
| − | [[Image:Sheep Pancreas.jpg|thumb|right| | + | [[Image:Sheep Pancreas.jpg|thumb|right|150px|Pancreas (Sheep) - © RVC 2008]] |
| − | + | *Located in the craniodorsal part of the abdomen in close association with the [[Duodenum - Anatomy & Physiology|duodenum]]. | |
| + | *Divided into three parts; a body and left and right lobes. | ||
| + | **The lobes are losely united by interlobular connective tissue. | ||
| + | ***Connective tissue contains blood vessels, nerves and lymphatics. | ||
| + | **Generally, the portal vein runs between the left and right lobes. (see [[#Species Differences|species differences]]). | ||
| + | *Rougly "V" shaped in all species. | ||
| + | *As mentioned in the [[#Development|development]] section, there are two ducts present in the pancreas. Their presence reflects the convergent development pattern of the pancreas. However in some [[#Species Differences|species]] one or other of the ducts may atrophy. | ||
| + | **The '''pancreatic duct''' is the biggest of the two and opens into the [[Duodenum - Anatomy & Physiology|duodenum]] with the bile duct at the major duodenal papilla. | ||
| + | **The '''accessory duct''' opens on the opposite aspect of the [[Duodenum - Anatomy & Physiology|duodenum]] at the minor duodenal papilla. | ||
==Exocrine Function== | ==Exocrine Function== | ||
'''Alkaline Secretion''' | '''Alkaline Secretion''' | ||
| − | + | *The pancreas produces an alakaline secretion. | |
| − | Pancreatic juice discharges into the duodenum through ducts. | + | *Pancreatic juice discharges into the [[Duodenum - Anatomy & Physiology|duodenum]] through ducts. |
| + | *Pancreatic juice is alkaline as it contains '''bicarbonate''' and '''chloride ions'''. | ||
| + | **Bicarbonate ions are actively transported into the duct lumen. | ||
| + | **Water follows passively by osmosis. | ||
| + | *Osmolarity of the pancreatic juice is equivalent to the osmolarity of the blood. | ||
| + | *Pancreatic juice is alkaline to neutralise the acidic gastric juice. This is advantageous because: | ||
| + | **It provides an optimal pH for the pancreatic enzymes. | ||
| + | **It prevents damage to the thin, absorptive mucosa of the [[Duodenum - Anatomy & Physiology|duodenum]]. | ||
| + | *Its alkalinity also helps to buffer the [[Large Intestine - Anatomy & Physiology|large intestine]] which is important in [[Hindgut Fermenters - Anatomy & Physiology|hindgut fermenters]] | ||
'''Enzymatic Digestion''' | '''Enzymatic Digestion''' | ||
| − | + | *The alkaline secretion contains digestive enyzmes that can digest protein, carbohydrates and lipids. Digestion is discussed in the [[Small Intestine - Anatomy & Physiology|small intestine]]. | |
| − | The alkaline secretion contains digestive | + | *The following table lists the enzymes secreted by the pancreas and their effects: |
| − | |||
| − | The following table lists the enzymes secreted by the pancreas and their effects: | ||
| Line 34: | Line 49: | ||
| '''Trypsin, Chymotrypsin, Elastase''' | | '''Trypsin, Chymotrypsin, Elastase''' | ||
| Peptides | | Peptides | ||
| − | | Endopeptidases; | + | | Endopeptidases; cleaves bonds between amino acids |
|- | |- | ||
| '''Carboxypeptidase and Aminopeptidase''' | | '''Carboxypeptidase and Aminopeptidase''' | ||
| Peptides | | Peptides | ||
| − | | Exopeptidases; | + | | Exopeptidases; cleaves bonds at the terminus of a peptide |
|- | |- | ||
| '''α - amylase''' | | '''α - amylase''' | ||
| Line 50: | Line 65: | ||
==Endocrine Function== | ==Endocrine Function== | ||
| + | *Functional units are the '''islets of Langerhans''', which are embedded throughout the exocrine tissue. | ||
| + | *Cells of the islets produce hormones that maintain normoglycaemia. | ||
| + | *Glucagon raises the blood glucose level. | ||
| + | *Insulin decreses the blood glucose level. | ||
| + | *Somatostatin acts in a paracrine fashion to inhibit both glucagon and insulin secretion. | ||
| + | *Pancreatic polypeptide is thought to be a cholecystokinin antagonist, and thus inhibits secretion of pancreatic juice. | ||
| − | + | ===Glucagon=== | |
| + | *Glucagon secretion is stimulated under conditions of hypoglycaemia and inhibited under conditions of hyperglycaemia. Parasympathetic innervation via the vagus nerve also stimulates release of glucagon. | ||
| + | *Glucagon has a ''catabolic'' effect on body reserves. | ||
| + | *The main target tissue is the [[Liver - Anatomy & Physiology|liver]]. | ||
| + | **Here it acts primarily to increase the degradation of glycogen via glycogenolysis and to increase the synthesis of glucose from amino acids via gluconeogenesis. | ||
| + | ***Glycogen regulates the reaction in glycolysis which converts phosphoenolpyruvate (PEP) to pyruvate. This reaction is catalysed by the enzyme '''pyruvate kinase''' and produces a molecule of ATP. Glucagon ''inactivates'' this enzyme by phosphorylation via protein kinase A (PKA). | ||
| + | **It increases the β oxidation of fatty acids to provide energy for gluconeogenesis. | ||
| + | *Glucagon also acts on other tissues, including adipose tissue where it increases the rate of lipolysis and, [[Muscles - Anatomy & Physiology|skeletal muscle]] where it increases the rate of protein catabolism. | ||
| + | *Glucagon reduces basal metabolic rate. | ||
| + | *Glucagon predominates during fasting metabolism. | ||
| + | **During fasting, the citric acid cycle turns slowly as oxaloacetate is removed to make glucose. Therefore, acetyl CoA (produced from lipolyis and protein catabolism) builds up and is converted to ketone bodies. [[Liver - degenerative#Ketosis|Ketosis]] may occur if the situation is prolonged. | ||
| − | + | ===Insulin=== | |
| + | [[Image:Pancreatic Beta Cell.jpg|thumb|right|150px|Pancreatic Beta Cell - © RVC 2008]] | ||
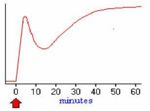
| + | [[Image:Insulin Secretion Pattern.jpg|thumb|right|150px|Insulin Secretion Pattern - © RVC 2008]] | ||
| + | *Insulin secretion is stimulated under conditions of hyperglycaemia and inhibited under conditions of hypoglycaemia. | ||
| + | *It has an ''anabolic'' effect on energy sources. | ||
| + | *It is a small polypeptide consisting of two chains; A and B; which are linked by disulphide bonds. | ||
| + | **It is synthesised inactively as a pre-pro-hormone which undergoes cleavage to produce the active form. | ||
| + | *Insulin is released when blood glucose levels are high. The process of insulin release occurs as follows: | ||
| + | **GLUT 2, which only operate at high glucose concentrations, are present in the plasma membranes of β cells. | ||
| + | **After a meal, glucose concentrations in the blood rise and glucose is taken into the cell. | ||
| + | **Glucose is metabolised inside the β cell which produces ATP. | ||
| + | **ATP inhibits potassium channels which depolarises the plasma membrane. | ||
| + | **Depolarisation causes calcium signalling, which stimulates insulin to be released. | ||
| + | *Pre-formed granules of insulin are release initially, but this supply soon diminishes. This produces a decrease in plasma insulin levels. Insulin levels are restored as de novo insulin is synthesised and secreted. | ||
| + | *Insulin exerts it's anabolic effect on the liver, adipocytes and skeletal muscle. | ||
| + | **It binds to receptors on the cell membrane, which triggers an intracellular signalling cascade. | ||
| + | **This causes preformed granules containing GLUT 4 receptors to be transported and expressed at the cell membrane. | ||
| + | **Cells can now take up glucose from the blood and store it as glycogen or fat. | ||
| + | *Increased glucose levels inside the cell increases the rate of glycogenesis and an increase in the rate of production of triacylglycerides. | ||
| + | *There is an increase in basal metabolic rate in other tissues. | ||
| + | **Insulin regulates the reaction in glycolysis where PEP is converted into pyruvate. This reaction is regulated by the enzyme pyruvate kinase. Insulin '''activates''' this enzyme by ''dephosphorylation'' via protein phosphatase 1 (PP1). This increases metabolism. | ||
===[[DM|Diabetes Mellitus]]=== | ===[[DM|Diabetes Mellitus]]=== | ||
| − | [[Image:NIDDM cat.jpg|thumb|right| | + | [[Image:NIDDM cat.jpg|thumb|right|150px|An obese cat with NIDDM - © RVC 2008]] |
| − | + | *A condition characterised by an inability to maintain normoglycaemia, with persistent hyperglycaemia observed. | |
| − | A condition characterised by an inability to maintain normoglycaemia, with persistent hyperglycaemia observed. | + | *Clinical signs include: |
| − | Clinical signs include: glucosuria, polyuria and polydipsia - blood glucose concentration exceeds the renal threshold (~10mmol/l) and is excreted into the urine. The increased osmotic potential of the filtrate draws water into the filtrate which is lost in the urine. The animal drinks more to compensate for water loss. | + | **glucosuria, polyuria and polydipsia - blood glucose concentration exceeds the renal threshold (~10mmol/l) and is excreted into the urine. The increased osmotic potential of the filtrate draws water into the filtrate which is lost in the urine. The animal drinks more to compensate for water loss. |
| − | + | **polyphagia and weight loss - the animal compensates for persistent loss of glucose | |
| − | + | **ketosis and ketonuria - ketones are released for energy. | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | ''' | + | '''Types of diabetes in dogs''' |
| + | *β cell deficiency - The majority of cases of [[DM|diabetes mellitus]] seen in dogs are of this kind. It causes an inability to produce insulin. | ||
| + | **Can be caused by congenital defects, pancreatitis and autoimmunity. | ||
| + | *Insulin antagonism - Seen in females in dioestrus, or in animals with [[General Pathology - Neoplasia|Cushing's]] (hyperadrenocorticism). | ||
| + | **[[Endocrine System - Ovaries - Anatomy & Physiology|Progesterone]], [[Endocrine System - Pituitary Growth Hormone - Anatomy & Physiology|growth hormone]] and cortisol are insulin antagonists. | ||
| − | '''Non Insulin Dependant Diabetes Mellitus (NIDDM) | + | '''Types of diabetes in cats''' |
| + | *Insulin Dependant Diabetes Mellitus (IDDM); insulin deficiency - similar to human diabetes type 1. There is a failure to produce insulin. | ||
| + | **Can be caused by islet-specific amyloidosis or chronic pancreatitis leading to β cell destruction. | ||
| + | *Non Insulin Dependant Diabetes Mellitus (NIDDM); insulin antagonism - similar to human diabetes type 2. | ||
| + | **Caused by obesity which leads to carbohydrate intolerance. | ||
==Vasculature== | ==Vasculature== | ||
| − | + | *Recieves blood supply from the '''coeliac''' and '''cranial mesenteric''' as branches from the splenic, hepatic and superior mesenteric arteries. | |
| + | **The right lobe recieves blood from the '''cranial pancreatoduodenal artery'''; a branch of the hepatic artery. | ||
| + | **The left lobe recieves blood from the splenic artery and '''caudal pancreatoduodenal artery'''; a branch of the cranial mesenteric artery. | ||
| + | *Vessels aborize within the connective tissure septa. | ||
| + | **Give off rich capillary networks that surround each acini and invade each islet. | ||
| + | **The endothelium in the exocrine pancreas is continuous, whereas the endothelium of capillaries surrounding the islets in the endocrine pancreas are fenestrated. | ||
| + | *Drained by veins that open into the portal vein. | ||
| + | *The islets recieve ample blood supply to enable an appropriate response to blood glucose level. | ||
==Innervation== | ==Innervation== | ||
| − | + | *Receives sypathetic and parasympathetic supply. | |
| − | + | **Parasympathetic is supplied by the dorsal vagal trunk. | |
| + | **Sympathetic is supplied by the solar plexus (splanchnic nerves). | ||
| + | *Parasympathetic and sympathetic stimulation results in exocytosis and accumulation of secretory vesicles in the lumen and ducts of the acini. | ||
| + | *Nervous regulation is thought to be of less importance than hormonal control. | ||
| + | *Hormones that increase pancreatic secretion: | ||
| + | **Cholecystokinin (CCK) | ||
| + | **Secretin | ||
| + | **Gastrin | ||
| + | *There is some negative feedback from somatostatin and enkephalins. | ||
==Lymphatics== | ==Lymphatics== | ||
| − | Blind ending lymphatic vessels drain into larger lymphatic vessels that follow the course of the blood vessels in the connective tissue. Lymph drains into the '''pancreaticoduodenal''' lymph nodes. It then drains into the coeliac centre, which surrounds the coeliac artery. | + | *Blind ending lymphatic vessels drain into larger lymphatic vessels that follow the course of the blood vessels in the connective tissue. |
| + | *Lymph drains into the '''pancreaticoduodenal''' lymph nodes. | ||
| + | *It then drains into the coeliac centre, which surrounds the coeliac artery. | ||
==Histology== | ==Histology== | ||
| + | |||
===Exocrine=== | ===Exocrine=== | ||
| − | [[Image:Islet and acini.jpg|thumb|right| | + | [[Image:Islet and acini.jpg|thumb|right|150px|Acini and islet of Langerhans - © RVC 2008]] |
| − | + | *Consists of acini, which resemble bunches of grapes. | |
| − | + | *Each acinus consists of a single layer of 40 - 50 pyramidal epithelial cells surrounding a lumen. | |
| − | The lumen of the acini drain into the | + | *The epithelial cells produce the secretion (pancreatic juice) containing enzymes, ions and water. |
| + | **Cells become wider during active secretion. | ||
| + | *The base of the acinar cells are strongly basophilic owing to the presence of endoplasmic reticulum where there is a high concentraion of RNA. This part of the cell therefore stains darker with haematoxylin and eosin. | ||
| + | *The apex of the cells is abundant with secretory granules containing the zymogen precursors of the pancreatic enzymes. | ||
| + | **The number of secretory granules increases after fasting and decreases after a meal. | ||
| + | *The lumen of the acini drain into the intercalated duct. | ||
| + | **Intercalated ducts converge to make larger interlobular ducts, which in turn converge to make interlobar ducts. | ||
| + | ***Interlobar ducts are found in the connective tissue septa between lobules. | ||
| + | ***Interlobar ducts join to form either the pancreatic or the accessory duct. | ||
| + | ****These ducts drain into the [[Duodenum - Anatomy & Physiology|duodenum]]. | ||
| + | ****In some cases the pancreatic duct unites with the bile duct, and bile and pancreatic juice enter the [[Duodenum - Anatomy & Physiology|duodenum]] together. | ||
===Endocrine=== | ===Endocrine=== | ||
| − | [[Image:Islet cell types.jpg|thumb|right| | + | [[Image:Islet cell types.jpg|thumb|right|150px|Islet of Langerhans - © RVC 2008]] |
| − | + | *Islets of Langerhans are embedded in the exocrine tissue. | |
| − | + | *Each islet is composed of 2 - 3 thousand epithelial cells. | |
| − | + | *Epithelial cells are arranged in a compact structure that is pervaded by a capillary network. | |
| − | + | *A thin layer of reticular fibres seperates the islets from surrounding exocrine tissue. | |
| − | + | *There are ''four'' different cell types within the islets of Langerhans that each produce different hormones. | |
| − | + | **α cells produce glucagon. Typically located at the periphery of the islet. Not present in all islets. | |
| − | + | **β cells produce insulin. The predominant cell type, located in the centre of the islet and contributing to 70% of all cells. | |
| − | + | **δ cells produce somatostatin. Low numbers in all islets. | |
| − | + | **F cells produce pancreatic polypeptide and are few in number, and may be present in the exocrine tissue also. | |
==Species Differences== | ==Species Differences== | ||
===Carnivore=== | ===Carnivore=== | ||
| − | + | *Clearly distinguishable as a body and left and right lobes. | |
| − | + | *Portal vein runs dorsally between the left and right lobes. | |
| − | + | *'''Left lobe''' is smaller than the right. | |
| − | In cats, the distal part of the accessory duct atrophies during development, so only the pancreatic duct persists. Cats normally have pacinian corpuscles in the interlobular tissue | + | *Tip of the left lobe contacts the left kidney and lies in the greater omentum. |
| + | *'''Right lobe''' follows the descending duodenum and lies in the mesoduodenum. | ||
| + | **Dorsally, it is related to the visceral surface of the [[Liver - Anatomy & Physiology|liver]], the ventral surface of the right kidney. | ||
| + | **Ventrally, it is related to the descending [[Duodenum - Anatomy & Physiology|duodenum]]. | ||
| + | **Laterally it is related to the ascending [[Colon - Anatomy & Physiology|colon]]. | ||
| + | *In dogs, both pancreatic and accessory ducts persist throughout development. | ||
| + | **However, the pancreatic duct is smaller. It joins the bile duct just before opening into the major duodenal papilla which lies 3-6cm distal to the pylorus of the [[Forestomach - Anatomy & Physiology|stomach]]. | ||
| + | **The accessory duct is the bigger duct and opens 3-5cm further distal to the pancreatic duct. | ||
| + | ***The two ducts communicate inside the pancreas. | ||
| + | *In cats, the distal part of the accessory duct atrophies during development, so only the pancreatic duct persists. | ||
| + | *Cats normally have pacinian corpuscles in the interlobular tissue and are visible grossly as 1-3cm in diameter. | ||
| + | *Dogs and cats produce little pancreatic juice between meals, but lots during a meal. | ||
===Ruminant=== | ===Ruminant=== | ||
| + | *Consists of a distinguishable short body and left and right lobes. | ||
| + | *The '''left lobe''' lies in the retroperitoneal space and is in contact with the [[Liver - Anatomy & Physiology|liver]], diaphragm and major vessels dorsally. | ||
| + | **Ventrally, it is in contact with intestines and dorsal sac of the [[The Rumen|rumen]]. | ||
| + | *The '''right lobe''' is larger and lies in the mesoduodenum against the flank of the animal and runs part of the length of the descending [[Duodenum - Anatomy & Physiology|duodenum]]. | ||
| + | *Portal vein passes dorsally at the pancreatic notch between the left and right lobes. | ||
| + | *In the ox, the distal part of the pancreatic duct atrophies during development, so only the accessory duct persists. | ||
| + | **The accessory duct enters the duodenum 20 to 25cm distal to the entry of the bile duct. | ||
| + | *In sheep and goats the distal part of the accessory duct atrophies during development, so only the pancreatic duct persists. | ||
| + | **It unifies with the bile duct so that both enter via a common duct. | ||
| + | *Constant secretion of pancreatic juice. | ||
| − | + | ===Equine=== | |
| + | *Lies mainly on the right, in the very dorsal part of the abdomen. | ||
| + | *It is triangular in shape and lies within the sigmoid flexure of the [[Duodenum - Anatomy & Physiology|duodenum]]. | ||
| + | *Lobes are less distinguishable compared to the dog. | ||
| + | *Ventral surface is directly attached to the right dorsal [[Colon - Anatomy & Physiology|colon]] and base of the [[Caecum - Anatomy & Physiology|caecum]]. | ||
| + | *Dorsal surface is directly attached to the right kidney and [[Liver - Anatomy & Physiology|liver]]. | ||
| + | *Portal vein perforates the pancreas at the '''pancreatic ring'''. | ||
| + | *Both pancreatic and accessory ducts persist throughout development. | ||
| + | *Constant secretion of pancreatic juice, which increases after feeding. This provides the caecum and [[Colon - Anatomy & Physiology|colon]] with a constant supply of buffered solution, which maintains a stable environment important for microbe survival. | ||
| − | === | + | ===Porcine=== |
| + | *Consists of a large body and left lobe, with a much smaller right lobe. | ||
| + | *Portal vein perforates the pancreas. | ||
| + | *The distal part of the pancreatic duct atrophies during development, so only the accessory duct persists. | ||
| + | *Two thirds lie to the left of the midline. | ||
| + | *Right portion lies adjacent to the descending [[Duodenum - Anatomy & Physiology|duodenum]] and it's cranial border contacts the [[Liver - Anatomy & Physiology|liver]]. | ||
| + | *Left portion is related to the [[Spleen - Anatomy & Physiology|spleen]], cranial pole of the [[Urinary System - Anatomy & Physiology|left kidney]] and the fundus of the [[Forestomach - Anatomy & Physiology|stomach]]. | ||
| − | + | ==Links== | |
| + | *[[Pancreas|Pathology of the pancreas]] | ||
| + | *[[Pancreas - Anatomy & Physiology - Flashcards|Pancreas Revision Flashcards]] | ||
| − | |||
| − | + | ===Videos=== | |
| − | + | *[http://stream2.rvc.ac.uk/Anatomy/feline/pot0357.mp4 Pot 357 The Feline Abdomen] | |
| + | *[http://stream2.rvc.ac.uk/Anatomy/bovine/Pot0061.mp4 Pot 61 The Bovine Liver] | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | [[ | + | <big><center>[[Alimentary - Anatomy & Physiology|'''BACK TO ALIMENTARY - ANATOMY & PHYSIOLOGY''']]</center></big> |
| − | |||
| − | |||
| − | |||
Revision as of 15:11, 26 July 2008
Introduction
The pancreas is a tubuloalveolar gland and has exocrine and endocrine tissues. The exocrine part secretes pancreatic juice; a solution containing enzymes for carbohydrate, protein and triacylglycerol digestion. Pancreatic juice drains into the small intestine where it is functional. It is the larger of the two parts of the pancreas. The endocrine part secretes hormones for the regulation of blood glucose concentration, including insulin, glucagon and somatostatin. The functional units of the exocrine part are the islets of Langerhans.
Development
The pancreas develops from endoderm, except for the connective tissue which develops from splanchnic mesoderm. Development begins with evaginations of the digestive tube caudal to the stomach. Two pancreatic buds form, one in the dorsal mesogastrium and one in the ventral mesogastrium. Some epithelial cells lose their connections to the developing duct system of the exocrine pancreas and develop into the islets of Langerhans of the endocrine pancreas. As the stomach rotates, the ventral bud moves to become more dorsal. The two buds then fuse; the left lobe is derived from the dorsal bud and the right lobe from the ventral bud. The duct of the ventral lobe (pancreatic duct) joins with the bile duct to form the common bile duct which opens into the duodenum at the major duodenal papilla. The duct of the dorsal lobe (accessory duct) enters the duodenum at the minor duodenal papilla. There is species variation in the persistance of each duct.
Structure
- Located in the craniodorsal part of the abdomen in close association with the duodenum.
- Divided into three parts; a body and left and right lobes.
- The lobes are losely united by interlobular connective tissue.
- Connective tissue contains blood vessels, nerves and lymphatics.
- Generally, the portal vein runs between the left and right lobes. (see species differences).
- The lobes are losely united by interlobular connective tissue.
- Rougly "V" shaped in all species.
- As mentioned in the development section, there are two ducts present in the pancreas. Their presence reflects the convergent development pattern of the pancreas. However in some species one or other of the ducts may atrophy.
Exocrine Function
Alkaline Secretion
- The pancreas produces an alakaline secretion.
- Pancreatic juice discharges into the duodenum through ducts.
- Pancreatic juice is alkaline as it contains bicarbonate and chloride ions.
- Bicarbonate ions are actively transported into the duct lumen.
- Water follows passively by osmosis.
- Osmolarity of the pancreatic juice is equivalent to the osmolarity of the blood.
- Pancreatic juice is alkaline to neutralise the acidic gastric juice. This is advantageous because:
- It provides an optimal pH for the pancreatic enzymes.
- It prevents damage to the thin, absorptive mucosa of the duodenum.
- Its alkalinity also helps to buffer the large intestine which is important in hindgut fermenters
Enzymatic Digestion
- The alkaline secretion contains digestive enyzmes that can digest protein, carbohydrates and lipids. Digestion is discussed in the small intestine.
- The following table lists the enzymes secreted by the pancreas and their effects:
| Enzyme | Substrate | Action |
|---|---|---|
| Trypsin, Chymotrypsin, Elastase | Peptides | Endopeptidases; cleaves bonds between amino acids |
| Carboxypeptidase and Aminopeptidase | Peptides | Exopeptidases; cleaves bonds at the terminus of a peptide |
| α - amylase | Polysaccharides: starch and glycogen | Endoglycosidase; cleaves bonds between carbohydrate monomers to produce maltose and short carbohydrate chains. |
| Pancreatic lipase | Triacylglycerols and 1,2 - diacylglycerols | Fatty acids, glycerol and 2 - monoacylglycerol |
Endocrine Function
- Functional units are the islets of Langerhans, which are embedded throughout the exocrine tissue.
- Cells of the islets produce hormones that maintain normoglycaemia.
- Glucagon raises the blood glucose level.
- Insulin decreses the blood glucose level.
- Somatostatin acts in a paracrine fashion to inhibit both glucagon and insulin secretion.
- Pancreatic polypeptide is thought to be a cholecystokinin antagonist, and thus inhibits secretion of pancreatic juice.
Glucagon
- Glucagon secretion is stimulated under conditions of hypoglycaemia and inhibited under conditions of hyperglycaemia. Parasympathetic innervation via the vagus nerve also stimulates release of glucagon.
- Glucagon has a catabolic effect on body reserves.
- The main target tissue is the liver.
- Here it acts primarily to increase the degradation of glycogen via glycogenolysis and to increase the synthesis of glucose from amino acids via gluconeogenesis.
- Glycogen regulates the reaction in glycolysis which converts phosphoenolpyruvate (PEP) to pyruvate. This reaction is catalysed by the enzyme pyruvate kinase and produces a molecule of ATP. Glucagon inactivates this enzyme by phosphorylation via protein kinase A (PKA).
- It increases the β oxidation of fatty acids to provide energy for gluconeogenesis.
- Here it acts primarily to increase the degradation of glycogen via glycogenolysis and to increase the synthesis of glucose from amino acids via gluconeogenesis.
- Glucagon also acts on other tissues, including adipose tissue where it increases the rate of lipolysis and, skeletal muscle where it increases the rate of protein catabolism.
- Glucagon reduces basal metabolic rate.
- Glucagon predominates during fasting metabolism.
- During fasting, the citric acid cycle turns slowly as oxaloacetate is removed to make glucose. Therefore, acetyl CoA (produced from lipolyis and protein catabolism) builds up and is converted to ketone bodies. Ketosis may occur if the situation is prolonged.
Insulin
- Insulin secretion is stimulated under conditions of hyperglycaemia and inhibited under conditions of hypoglycaemia.
- It has an anabolic effect on energy sources.
- It is a small polypeptide consisting of two chains; A and B; which are linked by disulphide bonds.
- It is synthesised inactively as a pre-pro-hormone which undergoes cleavage to produce the active form.
- Insulin is released when blood glucose levels are high. The process of insulin release occurs as follows:
- GLUT 2, which only operate at high glucose concentrations, are present in the plasma membranes of β cells.
- After a meal, glucose concentrations in the blood rise and glucose is taken into the cell.
- Glucose is metabolised inside the β cell which produces ATP.
- ATP inhibits potassium channels which depolarises the plasma membrane.
- Depolarisation causes calcium signalling, which stimulates insulin to be released.
- Pre-formed granules of insulin are release initially, but this supply soon diminishes. This produces a decrease in plasma insulin levels. Insulin levels are restored as de novo insulin is synthesised and secreted.
- Insulin exerts it's anabolic effect on the liver, adipocytes and skeletal muscle.
- It binds to receptors on the cell membrane, which triggers an intracellular signalling cascade.
- This causes preformed granules containing GLUT 4 receptors to be transported and expressed at the cell membrane.
- Cells can now take up glucose from the blood and store it as glycogen or fat.
- Increased glucose levels inside the cell increases the rate of glycogenesis and an increase in the rate of production of triacylglycerides.
- There is an increase in basal metabolic rate in other tissues.
- Insulin regulates the reaction in glycolysis where PEP is converted into pyruvate. This reaction is regulated by the enzyme pyruvate kinase. Insulin activates this enzyme by dephosphorylation via protein phosphatase 1 (PP1). This increases metabolism.
Diabetes Mellitus
- A condition characterised by an inability to maintain normoglycaemia, with persistent hyperglycaemia observed.
- Clinical signs include:
- glucosuria, polyuria and polydipsia - blood glucose concentration exceeds the renal threshold (~10mmol/l) and is excreted into the urine. The increased osmotic potential of the filtrate draws water into the filtrate which is lost in the urine. The animal drinks more to compensate for water loss.
- polyphagia and weight loss - the animal compensates for persistent loss of glucose
- ketosis and ketonuria - ketones are released for energy.
Types of diabetes in dogs
- β cell deficiency - The majority of cases of diabetes mellitus seen in dogs are of this kind. It causes an inability to produce insulin.
- Can be caused by congenital defects, pancreatitis and autoimmunity.
- Insulin antagonism - Seen in females in dioestrus, or in animals with Cushing's (hyperadrenocorticism).
- Progesterone, growth hormone and cortisol are insulin antagonists.
Types of diabetes in cats
- Insulin Dependant Diabetes Mellitus (IDDM); insulin deficiency - similar to human diabetes type 1. There is a failure to produce insulin.
- Can be caused by islet-specific amyloidosis or chronic pancreatitis leading to β cell destruction.
- Non Insulin Dependant Diabetes Mellitus (NIDDM); insulin antagonism - similar to human diabetes type 2.
- Caused by obesity which leads to carbohydrate intolerance.
Vasculature
- Recieves blood supply from the coeliac and cranial mesenteric as branches from the splenic, hepatic and superior mesenteric arteries.
- The right lobe recieves blood from the cranial pancreatoduodenal artery; a branch of the hepatic artery.
- The left lobe recieves blood from the splenic artery and caudal pancreatoduodenal artery; a branch of the cranial mesenteric artery.
- Vessels aborize within the connective tissure septa.
- Give off rich capillary networks that surround each acini and invade each islet.
- The endothelium in the exocrine pancreas is continuous, whereas the endothelium of capillaries surrounding the islets in the endocrine pancreas are fenestrated.
- Drained by veins that open into the portal vein.
- The islets recieve ample blood supply to enable an appropriate response to blood glucose level.
Innervation
- Receives sypathetic and parasympathetic supply.
- Parasympathetic is supplied by the dorsal vagal trunk.
- Sympathetic is supplied by the solar plexus (splanchnic nerves).
- Parasympathetic and sympathetic stimulation results in exocytosis and accumulation of secretory vesicles in the lumen and ducts of the acini.
- Nervous regulation is thought to be of less importance than hormonal control.
- Hormones that increase pancreatic secretion:
- Cholecystokinin (CCK)
- Secretin
- Gastrin
- There is some negative feedback from somatostatin and enkephalins.
Lymphatics
- Blind ending lymphatic vessels drain into larger lymphatic vessels that follow the course of the blood vessels in the connective tissue.
- Lymph drains into the pancreaticoduodenal lymph nodes.
- It then drains into the coeliac centre, which surrounds the coeliac artery.
Histology
Exocrine
- Consists of acini, which resemble bunches of grapes.
- Each acinus consists of a single layer of 40 - 50 pyramidal epithelial cells surrounding a lumen.
- The epithelial cells produce the secretion (pancreatic juice) containing enzymes, ions and water.
- Cells become wider during active secretion.
- The base of the acinar cells are strongly basophilic owing to the presence of endoplasmic reticulum where there is a high concentraion of RNA. This part of the cell therefore stains darker with haematoxylin and eosin.
- The apex of the cells is abundant with secretory granules containing the zymogen precursors of the pancreatic enzymes.
- The number of secretory granules increases after fasting and decreases after a meal.
- The lumen of the acini drain into the intercalated duct.
- Intercalated ducts converge to make larger interlobular ducts, which in turn converge to make interlobar ducts.
- Interlobar ducts are found in the connective tissue septa between lobules.
- Interlobar ducts join to form either the pancreatic or the accessory duct.
- Intercalated ducts converge to make larger interlobular ducts, which in turn converge to make interlobar ducts.
Endocrine
- Islets of Langerhans are embedded in the exocrine tissue.
- Each islet is composed of 2 - 3 thousand epithelial cells.
- Epithelial cells are arranged in a compact structure that is pervaded by a capillary network.
- A thin layer of reticular fibres seperates the islets from surrounding exocrine tissue.
- There are four different cell types within the islets of Langerhans that each produce different hormones.
- α cells produce glucagon. Typically located at the periphery of the islet. Not present in all islets.
- β cells produce insulin. The predominant cell type, located in the centre of the islet and contributing to 70% of all cells.
- δ cells produce somatostatin. Low numbers in all islets.
- F cells produce pancreatic polypeptide and are few in number, and may be present in the exocrine tissue also.
Species Differences
Carnivore
- Clearly distinguishable as a body and left and right lobes.
- Portal vein runs dorsally between the left and right lobes.
- Left lobe is smaller than the right.
- Tip of the left lobe contacts the left kidney and lies in the greater omentum.
- Right lobe follows the descending duodenum and lies in the mesoduodenum.
- In dogs, both pancreatic and accessory ducts persist throughout development.
- However, the pancreatic duct is smaller. It joins the bile duct just before opening into the major duodenal papilla which lies 3-6cm distal to the pylorus of the stomach.
- The accessory duct is the bigger duct and opens 3-5cm further distal to the pancreatic duct.
- The two ducts communicate inside the pancreas.
- In cats, the distal part of the accessory duct atrophies during development, so only the pancreatic duct persists.
- Cats normally have pacinian corpuscles in the interlobular tissue and are visible grossly as 1-3cm in diameter.
- Dogs and cats produce little pancreatic juice between meals, but lots during a meal.
Ruminant
- Consists of a distinguishable short body and left and right lobes.
- The left lobe lies in the retroperitoneal space and is in contact with the liver, diaphragm and major vessels dorsally.
- Ventrally, it is in contact with intestines and dorsal sac of the rumen.
- The right lobe is larger and lies in the mesoduodenum against the flank of the animal and runs part of the length of the descending duodenum.
- Portal vein passes dorsally at the pancreatic notch between the left and right lobes.
- In the ox, the distal part of the pancreatic duct atrophies during development, so only the accessory duct persists.
- The accessory duct enters the duodenum 20 to 25cm distal to the entry of the bile duct.
- In sheep and goats the distal part of the accessory duct atrophies during development, so only the pancreatic duct persists.
- It unifies with the bile duct so that both enter via a common duct.
- Constant secretion of pancreatic juice.
Equine
- Lies mainly on the right, in the very dorsal part of the abdomen.
- It is triangular in shape and lies within the sigmoid flexure of the duodenum.
- Lobes are less distinguishable compared to the dog.
- Ventral surface is directly attached to the right dorsal colon and base of the caecum.
- Dorsal surface is directly attached to the right kidney and liver.
- Portal vein perforates the pancreas at the pancreatic ring.
- Both pancreatic and accessory ducts persist throughout development.
- Constant secretion of pancreatic juice, which increases after feeding. This provides the caecum and colon with a constant supply of buffered solution, which maintains a stable environment important for microbe survival.
Porcine
- Consists of a large body and left lobe, with a much smaller right lobe.
- Portal vein perforates the pancreas.
- The distal part of the pancreatic duct atrophies during development, so only the accessory duct persists.
- Two thirds lie to the left of the midline.
- Right portion lies adjacent to the descending duodenum and it's cranial border contacts the liver.
- Left portion is related to the spleen, cranial pole of the left kidney and the fundus of the stomach.
Links
Videos