Difference between revisions of "Parathyroid Glands - Pathology"
Jump to navigation
Jump to search
m |
m |
||
| Line 8: | Line 8: | ||
<br> | <br> | ||
==Anatomy and Physiology== | ==Anatomy and Physiology== | ||
| − | Anatomy and Physiology of the Parathyroid glands can be found [[ | + | Anatomy and Physiology of the Parathyroid glands can be found [[Parathyroid Glands - Anatomy & Physiology|here]]. |
==Hypercalcaemia== | ==Hypercalcaemia== | ||
* Hypercalcaemia should not be ignored in an unwell animal. | * Hypercalcaemia should not be ignored in an unwell animal. | ||
Revision as of 16:48, 3 September 2008
|
|
Anatomy and Physiology
Anatomy and Physiology of the Parathyroid glands can be found here.
Hypercalcaemia
- Hypercalcaemia should not be ignored in an unwell animal.
- The consequences of hypercalcaemia may be serious: prolonged untreated hypercalcaemia can lead to irreversible damage to many organs, particularly the kidneys.
- There are multiple causes of hypercalcaemia, but if it is caught early a specific diagnosis and treatment are often possible.
- The clinical signs of hypercalcaemia are often vague.
- Signs commonly include:
- PU/PD
- Anorexia
- Dehydration
- Weakness or lethargy
- Vomiting
- Prerenal azotaemia
- More uncommonly, hypercalcaemia may present with:
- Constipation
- Cardiac arrhythmia
- Seizures or twitching
- Acute renal failure
- Death
- Signs commonly include:
- Causes of hypercalcaemia may be:
- Nonpathologic
- This may be due to:
- Age - young animals have naturally higher calcium levels.
- Lab error
- Lipaemia
- It is important to establish whether hypercalcaemia is true before persuing further diagnosis and treatment.
- This may be due to:
- Transient...
- ...hypoadrenocorticism
- ...haemoconcentration
- ...hyperproteinaemia
- Pathological
- Malignancy
- Lymphoma
- Anal sac adenocarcinoma
- Renal failure
- Hypervitaminosis D
- Granulomatous disease
- E.g fungal infections
- Primary hyperparathyroidism
- Skeletal lesions
- Nonpathologic
Hypocalcaemia
- Hypocalcaemia is a relatively common finding in
- Small animals
- Most often associated with decreased albumin concentrations.
- Usually clinically insignificant.
- Farm animals
- For example, dairy cows following parturition.
- More clinically significant.
- For example, dairy cows following parturition.
- Small animals
- Clinical signs may not always be present (i.e. clinically insignificant).
- Clinical signs are most often seen in associated with lactation or post-operative causes.
- When they seen, signs commonly include:
- Facial rubbing
- Muscle tremors or cramps
- Stiff gait
- Behavioural changes
- The following are seen less commonly:
- Panting
- Pyrexia
- Lethargy
- Anorexia
- Tachycardia or ECG abnormalities
- Hypotension
- Death
- Some causes of hypocalcaemia are also more common than others.
- Common causes are:
- Chronic renal failure
- Hypoalbuminaemia
- Eclampsia
- Acute pancreatitis
- Iatrogenic
- Post thyroidectomy
- Post parathyroidectomy
- Blood transfusion
- More uncommonly:
- Lab error
- Ethylene glycol toxicity
- NaHCO3 administration
- Hypovitaminosis D
- Hypomagnesaemia
- Intestinal malabsorption
- Primary hypoparathyroidism
- Common causes are:
Hyperparathyroidism
Primary
- Primary hyperparathyroidism is caused by glandular hyperplasia or neoplasia.
- Rare.
Secondary
- Secondary hyperparathyroidism causes fibrous osteodystrophy or "rubber jaw".
- In secondary hyperparathyroidism, the gland is overactive due to another condition coexisting in the body, rather than a primary parathyroid gland defect.
- There are two common forms of secondary hyperparathyroisism:
- Both forms result in increased osteoclastic resorption of bone and deposition of fibro-osteoid matrix that fails to mineralise.
- Flat bones of the skull swell.
- Fibrous tissue is seen around the tooth roots.
- Bone softens in adult animals.
- This is what gives rise to the term "rubber jaw".
- Long bones become soft with thin cortices.
- These fracture easily.
Nutritional Hyperparathyroidism
- Nutritional hyperparathyroidism is also known as nutritional osteodystrophy.
- This occurs most commonly in:
- Young, fast-growing animals
- Animals with a poor diet, for example:
- Swine fed unsupplemented cereal grain
- Dogs and cats fed all-meat diets
- Horses fed bran
- In this case, nutritional hyperparathyroidism is known as "bran disease".
Pathogenesis
- Pathogenesis follows low calcium/high phosphate diets.
- These lead to decreased serum calcium levels, stimulating PTH release.
- The increase in PTH gives an increase in bone resorption, causing pathology.
Pathology
- Gross
- Severe cases may show:
- Maxillary and mandibular swelling
- Teeth lost or buried in soft tissue
- Nasal and frontal bone enlargement, leading to dyspnoea
- Long bone fracture
- Detatchment tendons and ligaments
- Early or less severe cases are characterised by shifting lameness and ill thrift.
- Severe cases may show:
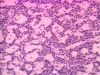
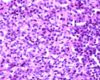
- Histological
- Osteoclastic resorption
- Fibrous replacement
Metabolic Bone Disease
- Metabolic bone disease affects lizards in captivity, particularly young green iguanas
- The condition is caused by:
- Dietary deficiency of calcium and vitamin D
- For example, due to poor lighting (which diminishes viatmin D production).
- Dietary excess of phosphorus
- Certain toxicities
- Diseases of the kidneys, liver or parathyroid
- This aetiology is rare
- Dietary deficiency of calcium and vitamin D
- Clinical signs include:
- Lethargy
- Inability to support weight
- Rounded skull
- Spontaneous fractures
- Adult animals also show signs of hypocalcaemia
- The skeleton shows reduced density on radiography.
Renal Hyperparathyroidism
- Renal Hyerparathyroidism is mostly seen in the dog as an expression of chronic renal disease.
Pathogenesis
- Chronic renal disease results in reduced glomerular filtration.
- As glomerular filtration is reduced, phosphate is retained. Chronic renal failure also causes inadequate vitamin D production in the kidneys.
- Hyperphosphataemia develops due to phosphate retention.
- Hypocalcaemia also occurs, as high levels of phosphate depress calcium levels.
- PTH is released in an attempt to maintain the correct blood calcium:phosphorous ratio. This can have several effects:
- Parathyroid hyperplasia
- I.e. renal secondary hyperparathyroidism.
- Soft tissue mineralisation
- Particularly seen in dogs
- Calcium is commonly deposited in the subpleural connective tissue of the intercostal spaces.
- Calcification also occurs in other sites, e.g. stomach wall, lungs, kidneys.
- Increased bone resorption
- This causes fibrous osteodystrophy, or "rubber jaw".
- Parathyroid hyperplasia
Pathology
- Pathology seen in renal hyperparathyroidism is very similar to that seen in nutritional hyperparathyroidism.
- Gross
- The major gross presentation is a fibrous osetodystrophy, or rubber jaw.
- The maxillae and mandible appear swollen.
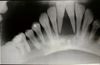
- Radiographically, bone shows reduced density, and teeth hence appear embedded in soft tissue.
- However, only a few cases of chronic renal disease show such severe bone lesions.
- Other lesions may also be seen.
- Intercostal muscles may be calcified.
- Bone marrow lesions may cause anaemia.
- The lung may show oedema, and have calcified alveolar walls.
- The major gross presentation is a fibrous osetodystrophy, or rubber jaw.
- Histological
- Osteoclastic resorption
- Fibrous replacement
Pseudo-Hyperparathyroidism
- Non-endocrine tumours may be capable of secreting hormones, or hormone-like factors.
- A parathormone-like substance may be secreted in such a manner.
Apocrine Gland Adenocarcinoma
- Malignant tumours of the anal sac apocrine glands can produce PTH-related peptide (PTHrp).
- This induces a pseudo-hyperparathyroidism and hypercalcaemia.
Lymphosarcoma
- 10 to 40% of cases in dogs may cause a pseudo-hyperparathyroidism.
Other Carcinomas
Some other carcinomas may also be capable of causing pseudo-hyperparathyroidism.
Hypoparathyroidism
- Hypoparathyroidism may result from primary gland hypofunction.
- Gland hypofunction occurs due to:
- Destruction of secretory cells by a disease process.
- For example, this may be immune mediated, or another inflammatory cause.
- A biochemical defect in synthetic pathway of the hormone.
- These are usually genetic aberrations.
- Defects in synthesis are not commonly identified in the veterinary species.
- Destruction of secretory cells by a disease process.
- Gland hypofunction occurs due to: