Difference between revisions of "Reabsorption and Secretion Along the Distal Tubule and Collecting Duct - Anatomy & Physiology"
(→Renin) |
|||
| (19 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
| − | {{ | + | {{toplink |
| + | |backcolour = C1F0F6 | ||
| + | |linkpage =Reabsorption and Secretion Along the Nephron - Anatomy & Physiology | ||
| + | |linktext =REABSORPTION AND SECRETION ALONG THE NEPHRON | ||
| + | |maplink = Urinary System (Content Map) - Anatomy & Physiology | ||
| + | |pagetype =Anatomy | ||
| + | }} | ||
| + | <br> | ||
| + | {|align="right" | ||
| + | |__TOC__ | ||
| + | |} | ||
| + | ==Distal Tubule== | ||
[[Image:disttubexch.jpg|right|thumb|250px|<small><center>Exchange in the Principal Cells of the Distal Tubule</center></small>]] | [[Image:disttubexch.jpg|right|thumb|250px|<small><center>Exchange in the Principal Cells of the Distal Tubule</center></small>]] | ||
| − | |||
[[Image:juxtaapp.jpg|right|thumb|250px|<small><center>Histology section showing the juxtaglomerular apparatus (© RVC 2008)</center></small>]] | [[Image:juxtaapp.jpg|right|thumb|250px|<small><center>Histology section showing the juxtaglomerular apparatus (© RVC 2008)</center></small>]] | ||
* Important site of regulation of ions and water | * Important site of regulation of ions and water | ||
| Line 11: | Line 21: | ||
** Potassium | ** Potassium | ||
** Acid / Base | ** Acid / Base | ||
| + | |||
| + | |||
* There are two cell types present each with different functions. They are similar to the cells of the collecting ducts | * There are two cell types present each with different functions. They are similar to the cells of the collecting ducts | ||
** Principal cells | ** Principal cells | ||
*** Absorb sodium | *** Absorb sodium | ||
*** Excrete potassium and hydrogen | *** Excrete potassium and hydrogen | ||
| − | *** Site of action of [[Aldosterone|Aldosterone]] | + | *** Site of action of [[Important Hormonal Regulators of the Kidney - Anatomy & Physiology#Aldosterone|Aldosterone]] |
** Intercalated cells | ** Intercalated cells | ||
*** ATP driven proton secretion | *** ATP driven proton secretion | ||
===Juxtaglomerular Apparatus=== | ===Juxtaglomerular Apparatus=== | ||
| + | |||
* The terminal portion of the straight distal tubule contacts the afferent and efferent vessels supplying its own glomerulus | * The terminal portion of the straight distal tubule contacts the afferent and efferent vessels supplying its own glomerulus | ||
* These vessels are said to embrace the distal tubule | * These vessels are said to embrace the distal tubule | ||
* Here a special apparatus called the Juxtaglomerular Apparatus has 3 different structures: | * Here a special apparatus called the Juxtaglomerular Apparatus has 3 different structures: | ||
| − | ** The tubular epithelial cells of the distal tubule which are in contact with the arterioles supplying the glomerulus of that nephron are called the '''macula densa'''. They play a vital role in the [[ | + | ** The tubular epithelial cells of the distal tubule which are in contact with the arterioles supplying the glomerulus of that nephron are called the '''macula densa'''. They play a vital role in the [[Autoregulation of GFR - Anatomy and Physiology#Tubuloglomerular Feedback (TGF)|regulation of the GFR]]. |
| − | ** The Juxtaglomerular Cells are smooth muscle cells which adjoin the macula densa in the capillary wall. | + | ** The [[Juxtaglomerular Cells of The Distal Tubule - Renal Physiology | Juxtaglomerular Cells]] are smooth muscle cells which adjoin the macula densa in the capillary wall. |
** The Extraglomerular Mesangium has an unclear function | ** The Extraglomerular Mesangium has an unclear function | ||
====Juxtaglomerular Cells==== | ====Juxtaglomerular Cells==== | ||
| + | |||
| + | =====Function===== | ||
| + | |||
* Smooth muscle cells | * Smooth muscle cells | ||
| − | * Synthesise [[ | + | * Synthesise [[Useful definitions - Renal Anatomy & Physiology#R| renin]] |
| − | * From the zymogen prerenin | + | * From the [http://en.wikipedia.org/wiki/Zymogen zymogen] prerenin |
* Described as intra-renal baroreceptors | * Described as intra-renal baroreceptors | ||
** Respond to stretch | ** Respond to stretch | ||
| Line 37: | Line 53: | ||
* Also respond to the sympathetic nervous system | * Also respond to the sympathetic nervous system | ||
** Increases renin output | ** Increases renin output | ||
| + | |||
| + | =====Renin===== | ||
| + | * A proteolytic enzyme synthesised in the kidney | ||
| + | * Renin affects blood pressure indirectly | ||
| + | * Part of the first stage of the [[Important Hormonal Regulators of the Kidney - Anatomy & Physiology#The Renin Angiotensin Aldosterone System (RAAS)| renin-angiotensin-aldosterone-system]] | ||
| + | ** Its effects are through its activation of this system | ||
===Developmental=== | ===Developmental=== | ||
| + | |||
Develops from metanephric tubule | Develops from metanephric tubule | ||
| Line 47: | Line 70: | ||
===Principal Cells=== | ===Principal Cells=== | ||
| + | |||
* [[Pituitary Gland - Anatomy & Physiology #Posterior Pituitary Gland | ADH]] acts on these cells inserting [[Aquaporins of the Kidney and Water Homeostasis - Anatomy & Physiology#What are Aquaporins|aquaporins]] into the cell membranes | * [[Pituitary Gland - Anatomy & Physiology #Posterior Pituitary Gland | ADH]] acts on these cells inserting [[Aquaporins of the Kidney and Water Homeostasis - Anatomy & Physiology#What are Aquaporins|aquaporins]] into the cell membranes | ||
* It is released from the [[Pituitary Gland - Anatomy & Physiology #Posterior Pituitary Gland | posterior pituitary gland]] | * It is released from the [[Pituitary Gland - Anatomy & Physiology #Posterior Pituitary Gland | posterior pituitary gland]] | ||
===Intercalated cells=== | ===Intercalated cells=== | ||
| + | |||
* The intercalated cells can be subdivided further to: | * The intercalated cells can be subdivided further to: | ||
** Alpha intercalated cells secrete H<sup>+</sup> | ** Alpha intercalated cells secrete H<sup>+</sup> | ||
| Line 56: | Line 81: | ||
===Developmental=== | ===Developmental=== | ||
| + | |||
* Develops from branched ureteric bud | * Develops from branched ureteric bud | ||
===The Concentrating Mechanism, Aquaporins and ADH=== | ===The Concentrating Mechanism, Aquaporins and ADH=== | ||
| + | |||
Water is drawn from the lumen of the tubule by the increasing hypertonicity of the surrounding tissue as the duct makes its way deeper into the medulla. However this reabsorption is only possible thanks to [[Aquaporins of the Kidney and Water Homeostasis - Anatomy & Physiology|ADH]] inserting [[Aquaporins of the Kidney and Water Homeostasis - Anatomy & Physiology#What are Aquaporins|aquaporins]] into the apical membrane. These channels are always present on the basolateral membrane of the epithelial cells but not on the apical membrane. The reabsorption would not be possible if the urine did not go back up the [[Reabsorption and Secretion Along the Loop of Henle - Anatomy & Physiology#Thick ascending limb| thick ascending limb]] of the loop of henle, where its concentration was decreased by the reabsorption of salt, but instead went straight into the collecting ducts. Although this would mean very concentrated urine it would result in massive salt losses. Thus the collecting duct allows for very concentrated urine with minimal salt loss. It also allows the concentration of the urine to vary from dilute to concentrated under the control of the hypothalamus and ADH concentrations. | Water is drawn from the lumen of the tubule by the increasing hypertonicity of the surrounding tissue as the duct makes its way deeper into the medulla. However this reabsorption is only possible thanks to [[Aquaporins of the Kidney and Water Homeostasis - Anatomy & Physiology|ADH]] inserting [[Aquaporins of the Kidney and Water Homeostasis - Anatomy & Physiology#What are Aquaporins|aquaporins]] into the apical membrane. These channels are always present on the basolateral membrane of the epithelial cells but not on the apical membrane. The reabsorption would not be possible if the urine did not go back up the [[Reabsorption and Secretion Along the Loop of Henle - Anatomy & Physiology#Thick ascending limb| thick ascending limb]] of the loop of henle, where its concentration was decreased by the reabsorption of salt, but instead went straight into the collecting ducts. Although this would mean very concentrated urine it would result in massive salt losses. Thus the collecting duct allows for very concentrated urine with minimal salt loss. It also allows the concentration of the urine to vary from dilute to concentrated under the control of the hypothalamus and ADH concentrations. | ||
==Ions and Compounds== | ==Ions and Compounds== | ||
| + | |||
The following ions and compounds are reabsorbed or secreted partly or completely in the distal tubules and collecting ducts: | The following ions and compounds are reabsorbed or secreted partly or completely in the distal tubules and collecting ducts: | ||
===Sodium=== | ===Sodium=== | ||
| + | |||
The remaining 10% is reabsorbed in the distal tubule. Although the transport capacity here is minimal the high resistance epithelia mean that very little back flow into the lumen occurs allowing the remaining sodium to be easily reabsorbed. Some of this reabsorption takes place using a sodium chloride co-transporter. The reabsorption of sodium from here and the collecting ducts is under hormonal control allowing "fine tuning" to occur. | The remaining 10% is reabsorbed in the distal tubule. Although the transport capacity here is minimal the high resistance epithelia mean that very little back flow into the lumen occurs allowing the remaining sodium to be easily reabsorbed. Some of this reabsorption takes place using a sodium chloride co-transporter. The reabsorption of sodium from here and the collecting ducts is under hormonal control allowing "fine tuning" to occur. | ||
'''See:''' | '''See:''' | ||
| − | * [[Aldosterone|Aldosterone]] | + | * [[Important Hormonal Regulators of the Kidney - Anatomy & Physiology#Aldosterone|Aldosterone]] |
| − | * [[Atrial Natriuretic Peptide|Atrial Natriuretic Peptide]] | + | * [[Important Hormonal Regulators of the Kidney - Anatomy & Physiology#Atrial Natriuretic Peptide|Atrial Natriuretic Peptide]] |
===Potassium=== | ===Potassium=== | ||
| Line 96: | Line 125: | ||
===Urea=== | ===Urea=== | ||
| + | |||
In the lower portion of the collecting duct urea freely diffuses across the epithelia. The permeability is also increased with ADH. This adds to the hypertonicity of the medulla and increases water reabsorption. | In the lower portion of the collecting duct urea freely diffuses across the epithelia. The permeability is also increased with ADH. This adds to the hypertonicity of the medulla and increases water reabsorption. | ||
=====Urea and Water Reabsorption===== | =====Urea and Water Reabsorption===== | ||
| + | |||
Water follows urea as it is reabsorbed from the collecting duct. This actually increases the concentration of urea in the tubular fluid despite some of it being reabsorbed. This means that urea concentration only drops moderately when the urine concentration falls due to increased reabsorption of water. | Water follows urea as it is reabsorbed from the collecting duct. This actually increases the concentration of urea in the tubular fluid despite some of it being reabsorbed. This means that urea concentration only drops moderately when the urine concentration falls due to increased reabsorption of water. | ||
| − | ===[[Calcium|Calcium]]=== | + | ===[[Calcium Homeostasis - Anatomy & Physiology|Calcium]]=== |
| − | The regulation of how much calcium is reabsorbed occurs in the ascending limb of the loop of henle, the distal tubule and collecting ducts. [[Calcium #Parathyroid Hormone (PTH)| Parathyroid hormone]] stimulates reabsorption. It is normal for a 1-2% excretion of calcium to occur | + | The regulation of how much calcium is reabsorbed occurs in the ascending limb of the loop of henle, the distal tubule and collecting ducts. [[Calcium Homeostasis - Anatomy & Physiology #Parathyroid Hormone (PTH)| Parathyroid hormone]] stimulates reabsorption. It is normal for a 1-2% excretion of calcium to occur |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Revision as of 17:48, 7 September 2008
|
|
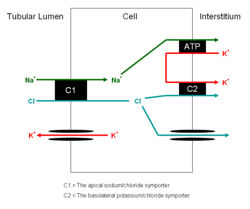
Distal Tubule
- Important site of regulation of ions and water
- Less emphasis on bulk transport compared with proximal tubule
- More emphasis on fine management
- It is able to do this as it has high resistance epithelia. Allowing it to maintain substantial gradients across it
- Very important for the homeostasis of:
- Sodium
- Potassium
- Acid / Base
- There are two cell types present each with different functions. They are similar to the cells of the collecting ducts
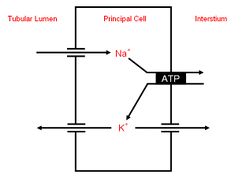
- Principal cells
- Absorb sodium
- Excrete potassium and hydrogen
- Site of action of Aldosterone
- Intercalated cells
- ATP driven proton secretion
- Principal cells
Juxtaglomerular Apparatus
- The terminal portion of the straight distal tubule contacts the afferent and efferent vessels supplying its own glomerulus
- These vessels are said to embrace the distal tubule
- Here a special apparatus called the Juxtaglomerular Apparatus has 3 different structures:
- The tubular epithelial cells of the distal tubule which are in contact with the arterioles supplying the glomerulus of that nephron are called the macula densa. They play a vital role in the regulation of the GFR.
- The Juxtaglomerular Cells are smooth muscle cells which adjoin the macula densa in the capillary wall.
- The Extraglomerular Mesangium has an unclear function
Juxtaglomerular Cells
Function
- Smooth muscle cells
- Synthesise renin
- From the zymogen prerenin
- Described as intra-renal baroreceptors
- Respond to stretch
- The secretion of renin from these cells depends on the stretch
- If stretch decreases - blood pressure has decreased - renin secretion increases
- Also respond to the sympathetic nervous system
- Increases renin output
Renin
- A proteolytic enzyme synthesised in the kidney
- Renin affects blood pressure indirectly
- Part of the first stage of the renin-angiotensin-aldosterone-system
- Its effects are through its activation of this system
Developmental
Develops from metanephric tubule
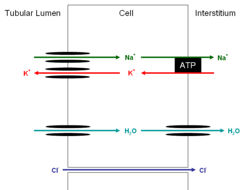
Collecting Duct
This part of the nephron has two cell types
Principal Cells
- ADH acts on these cells inserting aquaporins into the cell membranes
- It is released from the posterior pituitary gland
Intercalated cells
- The intercalated cells can be subdivided further to:
- Alpha intercalated cells secrete H+
- Beta intercalated cells secrete HCO3-
Developmental
- Develops from branched ureteric bud
The Concentrating Mechanism, Aquaporins and ADH
Water is drawn from the lumen of the tubule by the increasing hypertonicity of the surrounding tissue as the duct makes its way deeper into the medulla. However this reabsorption is only possible thanks to ADH inserting aquaporins into the apical membrane. These channels are always present on the basolateral membrane of the epithelial cells but not on the apical membrane. The reabsorption would not be possible if the urine did not go back up the thick ascending limb of the loop of henle, where its concentration was decreased by the reabsorption of salt, but instead went straight into the collecting ducts. Although this would mean very concentrated urine it would result in massive salt losses. Thus the collecting duct allows for very concentrated urine with minimal salt loss. It also allows the concentration of the urine to vary from dilute to concentrated under the control of the hypothalamus and ADH concentrations.
Ions and Compounds
The following ions and compounds are reabsorbed or secreted partly or completely in the distal tubules and collecting ducts:
Sodium
The remaining 10% is reabsorbed in the distal tubule. Although the transport capacity here is minimal the high resistance epithelia mean that very little back flow into the lumen occurs allowing the remaining sodium to be easily reabsorbed. Some of this reabsorption takes place using a sodium chloride co-transporter. The reabsorption of sodium from here and the collecting ducts is under hormonal control allowing "fine tuning" to occur.
See:
Potassium
Distal Tubule
- Here the potassium and chloride symporter actually excretes the two ions into the lumen of the tubule
- Na+ / K+ ATPases in the basolateral membrane move potassium into epithelial cells from the intercellular spaces in order to remove sodium. The potassium then diffuses into the lumen via channels
- The ability to secrete potassium here is vital in animals with high potassium diets such as herbivores where excreting only the amount filtered would not be suffice
Principal Cells of Collecting Duct
- Potassium transported into lumen
- Is both absorbed and secreted via paracellular route
- Na+ / K+ ATPases in the basolateral membrane move potassium into epithelial cells from the intercellular spaces in order to remove sodium and keep potassium concentrations high.
- Aldosterone works here
Intercalated Cells of Collecting Duct
- Potassium is absorbed here in exchange for hydrogen
H+ and HCO3-
- H+ ions are secreted in the cortical and medullary collecting tubules
- This is an active secretion using a H+ ATPase
- Also a H+/K+ ATPase antiporter
- The main function of this is maintaining potassium
- HCO3- is reabsorbed here
Urea
In the lower portion of the collecting duct urea freely diffuses across the epithelia. The permeability is also increased with ADH. This adds to the hypertonicity of the medulla and increases water reabsorption.
Urea and Water Reabsorption
Water follows urea as it is reabsorbed from the collecting duct. This actually increases the concentration of urea in the tubular fluid despite some of it being reabsorbed. This means that urea concentration only drops moderately when the urine concentration falls due to increased reabsorption of water.
Calcium
The regulation of how much calcium is reabsorbed occurs in the ascending limb of the loop of henle, the distal tubule and collecting ducts. Parathyroid hormone stimulates reabsorption. It is normal for a 1-2% excretion of calcium to occur