Difference between revisions of "Dermatophytosis"
Jump to navigation
Jump to search
Fiorecastro (talk | contribs) |
m |
||
| (40 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
| + | {{unfinished}} | ||
| − | + | {{toplink | |
| + | |backcolour = | ||
| + | |linkpage =Fungi | ||
| + | |linktext =FUNGI | ||
| + | |pagetype=Bugs | ||
| + | }} | ||
| + | <br> | ||
| + | [[Image:Dermatophyte arthrospore hair root.jpg|thumb|right|200px|Dermatophyte arthrospores on a hair root - Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] | ||
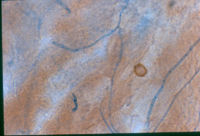
| + | [[Image:Dermatophyte mycelium in skin.jpg|thumb|right|200px|Dermatophytosis mycelium in skin - Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] | ||
| + | [[Image:Dermatophyte skin KOH.jpg|thumb|right|200px|Dermatophyte in skin using a KOH mount - Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] | ||
| + | [[Image:Ringworm on human arm.jpg|thumb|right|150px|Ringworm on a human arm - Wikimedia Commons]] | ||
| + | [[Image:Dermatophytosis in a dog.jpg|thumb|right|200px|Dermatophytosis in a dog - Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] | ||
| + | [[Image:Dermatophytosis in a cow.jpg|thumb|right|200px|Dermatophytosis in a cow - Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] | ||
| + | [[Image:Dermatophytosis in a chicken.jpg|thumb|right|200px|Dermatophytosis in a chicken - Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] | ||
| + | [[Image:Dermatophytosis dog foot.jpg|thumb|right|200px|Dermatophytosis lesion on a dog's leg - Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] | ||
| + | [[Image:Dermatophytosis in a horse.jpg|thumb|right|200px|Dermatophytosis in a horse - Copyright Professor Andrew N. Rycroft, BSc, PHD, C. Biol.F.I.Biol., FRCPath]] | ||
| + | |||
| + | ==General== | ||
| + | |||
| + | *Pigmented, saprophytic organisms called '''Phaeohyphomycetes''' | ||
| + | **Previously called 'Fungi Imperfecti' | ||
| − | + | *The two main species of veterinary interest are ''Microsporum'' and ''Trichophton'' | |
| − | |||
| − | |||
| − | + | *Worldwide | |
| − | + | *They are usually secondary invaders | |
| − | + | *Able to penetrate all layers of [[Skin - Anatomy & Physiology|skin]], but are generally restricted to the keratin layer and its appendages | |
| + | **Therefore, most often seen in subcuticular or cutaneous sites | ||
| + | **Lack of tolerance to body temperature and antifungal activity in serum and body fluids prevent the fungi invading subcutaneously | ||
| − | + | *Transmitted by direct or indirect contact | |
| − | |||
| − | + | *Immunuocompromised hosts may develop systemic infections | |
| − | + | *''Microsporum'' - zoophilic | |
| + | **Parasites of animals | ||
| − | + | *''Trichophyton'' - geophilic | |
| + | **Inhabits soil | ||
| − | + | *''Epidermophyton'' - anthropophilic | |
| + | **Parasites of people | ||
| − | + | *Common in many species, especially cats | |
| − | + | *Hot, humid environment predisposes to infection | |
| − | + | *More common in young animals | |
| − | + | *Produce proteolytic enzymes to penetrate surface lipid | |
| − | + | *Fungal hyphae invade keratin -> break into arthrospores | |
| − | + | *Phaeohyphomycosis: | |
| + | **Occurs sporadically in cats, horses, cattle, fish, reptiles, amphibians, birds, and rarely in dogs | ||
| + | **Examples include: ''Exophiala'' sp., ''Phialophora'' sp., ''Pseudomicrodochium'' sp., ''Bipolaris'' sp., ''Moniella'' sp., ''Cladosporium'' sp., ''Wangiella'' sp., ''Curvularia'' spp., ''Exserohilum'' sp., ''Alternaria'' sp., ''Staphylotrichum'' sp., and ''Xylohypha'' sp | ||
| + | **Culture is necessary for definitive diagnosis | ||
| − | + | ==Pathogenesis== | |
| − | [[ | + | *Epidermal hyperplasia ([[Skin Glossary - Pathology|hyperkeratosis, parakeratosis, acanthosis]]) and [[Inflammation - WikiBlood|inflammation]] |
| − | + | *Superficial perivascular dermatitis -> exocytosis (migration through epidermal layers) -> intracorneal microabscesses | |
| − | + | *Exocytosis -> folliculitis -> furunculosis | |
| − | + | *Highly variable lesions | |
| − | + | *Normal -> eruptive nodular -> pseudomycetoma -> onychomycosis | |
| − | + | *Secondary invasion by [[Staphylococcus spp.|''Staphylococcus aureus'']] and [[Staphylococcus spp.|''Staphylococcus intermedius'']] are common and cause pustules in the hair follicles | |
| − | + | *Grossly: | |
| − | + | **Circular or irregular lesion, may coalesce | |
| − | + | **Scaly to crusty patches | |
| − | + | **Alopecia due to broken hair shafts and hairs lost from inflammed follicles | |
| − | + | **Follicular papules and pustules | |
| − | + | **Peripheral red ring ('''ringworm''') due to dead fungi in areas of [[Inflammation - WikiBlood|inflammation]] at centre of lesions and viable fungi peripherally | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | *More common in housed animals, rather than animals turned out to pasture | |
| − | + | ||
| − | + | *Highest incidence of disease during the winter | |
| − | + | **May resolve spontaneously in the spring and summer | |
| + | |||
| + | ==Histology== | ||
| + | |||
| + | *Perifolliculitis, folliculitis or furunculosis | ||
| + | |||
| + | *Epidermal hyperplasia | ||
| + | |||
| + | *Intracorneal microabscesses | ||
| + | |||
| + | *Septate hyphae or spores may be found in stratum corneum and keratin of hair follicles | ||
| + | |||
| + | ==Diagnosis== | ||
| + | |||
| + | *Wood's Lamp | ||
| + | **UV light | ||
| + | **Florourescence if fungi present | ||
| + | *Samples can be examined in 10-20% KOH for the presence of hyphae or arthrospores | ||
| + | **Lactophenol Cotton Blue enhances visualisation | ||
| − | + | *Sabouraud's Dextrose agar containing cyclohexamide and [[Chloramphenicol|chloramphenicol]] at room temperature for a month for culture | |
| − | |||
| − | | | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | *Dermatophyte Test Medium | |
| + | **Saubouraud's Dextrose agar with phenol red indicator | ||
| + | **Medium changes from yellow to red if fungi present | ||
| − | + | ==Treatment== | |
| − | + | *Isolation of infected animal | |
| − | + | *Precautions should be taken to prevent human infection | |
| − | + | *[[Antifungal Drugs#Griseofluvin|Griseofulvin]] best method of treatment | |
| + | **Expensive | ||
| + | **Oral dosage | ||
| + | **Prolonged treatment required | ||
| − | + | *Whitfield's ointment | |
| + | **Salicylic and benzoic acid | ||
| − | + | *Other treatments: | |
| + | **Aqueous lime sulphur topically for dogs | ||
| + | **Iodine | ||
| + | **[[Antibiotics|Antibiotics]] | ||
| + | **[[Antifungal Drugs#Polyene Antifungals|Natamycin]] antifungal | ||
| + | **[[Antifungal Drugs#The Azoles|Imidiazole]] derivatives | ||
| − | + | ==Further Links== | |
| − | |||
| − | + | *Pathology of [[Mycotic skin infections - Pathology#Dermatophytoses|dermatophytosis]] | |
| − | |||
| − | [[ | + | *[[Antifungal Drugs]] |
| − | |||
Revision as of 16:57, 4 June 2009
| This article is still under construction. |
|
|
General
- Pigmented, saprophytic organisms called Phaeohyphomycetes
- Previously called 'Fungi Imperfecti'
- The two main species of veterinary interest are Microsporum and Trichophton
- Worldwide
- They are usually secondary invaders
- Able to penetrate all layers of skin, but are generally restricted to the keratin layer and its appendages
- Therefore, most often seen in subcuticular or cutaneous sites
- Lack of tolerance to body temperature and antifungal activity in serum and body fluids prevent the fungi invading subcutaneously
- Transmitted by direct or indirect contact
- Immunuocompromised hosts may develop systemic infections
- Microsporum - zoophilic
- Parasites of animals
- Trichophyton - geophilic
- Inhabits soil
- Epidermophyton - anthropophilic
- Parasites of people
- Common in many species, especially cats
- Hot, humid environment predisposes to infection
- More common in young animals
- Produce proteolytic enzymes to penetrate surface lipid
- Fungal hyphae invade keratin -> break into arthrospores
- Phaeohyphomycosis:
- Occurs sporadically in cats, horses, cattle, fish, reptiles, amphibians, birds, and rarely in dogs
- Examples include: Exophiala sp., Phialophora sp., Pseudomicrodochium sp., Bipolaris sp., Moniella sp., Cladosporium sp., Wangiella sp., Curvularia spp., Exserohilum sp., Alternaria sp., Staphylotrichum sp., and Xylohypha sp
- Culture is necessary for definitive diagnosis
Pathogenesis
- Epidermal hyperplasia (hyperkeratosis, parakeratosis, acanthosis) and inflammation
- Superficial perivascular dermatitis -> exocytosis (migration through epidermal layers) -> intracorneal microabscesses
- Exocytosis -> folliculitis -> furunculosis
- Highly variable lesions
- Normal -> eruptive nodular -> pseudomycetoma -> onychomycosis
- Secondary invasion by Staphylococcus aureus and Staphylococcus intermedius are common and cause pustules in the hair follicles
- Grossly:
- Circular or irregular lesion, may coalesce
- Scaly to crusty patches
- Alopecia due to broken hair shafts and hairs lost from inflammed follicles
- Follicular papules and pustules
- Peripheral red ring (ringworm) due to dead fungi in areas of inflammation at centre of lesions and viable fungi peripherally
- More common in housed animals, rather than animals turned out to pasture
- Highest incidence of disease during the winter
- May resolve spontaneously in the spring and summer
Histology
- Perifolliculitis, folliculitis or furunculosis
- Epidermal hyperplasia
- Intracorneal microabscesses
- Septate hyphae or spores may be found in stratum corneum and keratin of hair follicles
Diagnosis
- Wood's Lamp
- UV light
- Florourescence if fungi present
- Samples can be examined in 10-20% KOH for the presence of hyphae or arthrospores
- Lactophenol Cotton Blue enhances visualisation
- Sabouraud's Dextrose agar containing cyclohexamide and chloramphenicol at room temperature for a month for culture
- Dermatophyte Test Medium
- Saubouraud's Dextrose agar with phenol red indicator
- Medium changes from yellow to red if fungi present
Treatment
- Isolation of infected animal
- Precautions should be taken to prevent human infection
- Griseofulvin best method of treatment
- Expensive
- Oral dosage
- Prolonged treatment required
- Whitfield's ointment
- Salicylic and benzoic acid
- Other treatments:
- Aqueous lime sulphur topically for dogs
- Iodine
- Antibiotics
- Natamycin antifungal
- Imidiazole derivatives
Further Links
- Pathology of dermatophytosis