Difference between revisions of "Inflammatory Bowel Disease"
TestStudent (talk | contribs) |
|||
| (57 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
| − | {{ | + | {{unfinished}} |
| − | |||
| − | + | {{dog}} | |
| − | + | {{cat}} | |
| − | |||
==Signalment== | ==Signalment== | ||
| − | + | *No sex predisposition | |
| + | *There are contraditions with regard to age predisposition | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | == | + | ==Description== |
| − | + | '''Inflammatory bowel disease (IBD)''' is an idiopathic group of disorders characterised by intestinal inflammatory changes, associated with persistent or recurrent gastrointestinal signs. IBD can affect any part of the intestines and is classified according to the predominant cellular inflammatory infiltration. Several histological types have been recognised, which are: | |
| + | *[[Lymphocytic - Plasmacytic Enteritis - WikiClinical|Lymphocytic - Plasmacytic Enteritis]] (LPE) | ||
| + | *[[Eosinophilic Enteritis - WikiClinical|Eosinophilic Enteritis]] (EE) | ||
| − | + | There is no underlying cause of IBD in 75% of cases. They are thought to reflect an exaggerated or inappropriate response by the immune system to dietary, bacterial or self-antigens. IBD is a diagnosis of exclusion. Other differential diagnoses have to be investigated and ruled out before a diagnosis of IBD can be made. | |
| − | |||
| − | |||
| − | + | ==Diagnosis== | |
| + | ===Clinical Signs=== | ||
| + | *'''[[Stomach and Abomasum Consequences of Gastric Disease - Pathology|Vomiting]]'''; very common in cat, more common than diarrhoea | ||
| + | *'''[[Intestine Diarrhoea - Pathology|Diarrhoea]]'''; very common in dog, more common than vomiting, usually small intestinal | ||
| + | *'''Weight loss'''; nearly all cases of chronic small intestinal disease | ||
| + | *Variable appetite; increased or decreased which relates to severity | ||
| + | *Lethargy; common in severe cases | ||
| + | *Anorexia; common in severe cases | ||
| + | *[[Small Intestinal Bacterial Overgrowth and Antibiotic Responsive Diarrhoea - WikiClinical|Antibiotic responsive diarrhoea]] | ||
| + | *Abdominal discomfort or pain | ||
| + | *Excessive borborygmi | ||
| + | *Haematemesis or haematochezia (more severe cases) | ||
| + | *Hypoproteinaemia or ascites | ||
| + | *Thickened intestinal loop | ||
| − | |||
| − | + | ===Laboratory Tests=== | |
| + | ====Haematology==== | ||
| + | *[[Changes in Inflammatory Cells Circulating in Blood - Pathology#Neutrophilia|Neutrophilia]] ± mild left shift in [[Lymphocytic - Plasmacytic Enteritis - WikiClinical|LPE]] | ||
| + | *[[Changes in Inflammatory Cells Circulating in Blood - Pathology#Eosinophilia|Eosinophilia]] | ||
| + | **Not always present in [[Eosinophilic Enteritis - WikiClinical|EE]] | ||
| − | '''Serum folate | + | ====Biochemistry==== |
| + | *Panhypoproteinaemia | ||
| + | *Hypocholesterolaemia | ||
| + | *Mild increased in liver enzymes, secondary to intestinal [[Inflammation - Pathology|inflammation]] | ||
| + | |||
| + | ====Other Tests==== | ||
| + | *Faecal analysis should be carried out to rule out parasitic causes such as [[Trichuris vulpis|whipworms]], [[Uncinaria stenocephala|hookworms]] and [[Giardia|''Giardia'']]. | ||
| + | *Serum folate level decreases with proximal small intestinal [[Inflammation - Pathology|inflammation]]. | ||
| + | *Serum cobalamin level decreases with distal small intestinal [[Inflammation - Pathology|inflammation]]. | ||
===Diagnostic Imaging=== | ===Diagnostic Imaging=== | ||
| − | + | ====Radiography==== | |
Plain radiography is used to evaluate for anatomic abnormalities. Contrast study is only valuable if there is a severe mucosal disease. | Plain radiography is used to evaluate for anatomic abnormalities. Contrast study is only valuable if there is a severe mucosal disease. | ||
| − | + | ====Ultrasonography==== | |
| − | Ultrasonography may reveal mesenteric lymphadenopathy and thickening of the intestinal wall. | + | Ultrasonography may reveal mesenteric [[Lymph Nodes - Pathology|lymphadenopathy]] and thickening of the intestinal wall. |
| + | |||
===Histopathology=== | ===Histopathology=== | ||
| − | A biopsy of the intestine is required for a definitive diagnosis of IBD. A non-invasive biopsy may be taken via endoscopy. However, this limits where the samples can be taken from as the [[Jejunum - Anatomy & Physiology|jejunum]] and [[Ileum - Anatomy & Physiology|ileum]] | + | A biopsy of the intestine is required for a definitive diagnosis of IBD. A non-invasive biopsy may be taken via endoscopy. However, this limits where the samples can be taken from as the [[Jejunum - Anatomy & Physiology|jejunum]] and [[Ileum - Anatomy & Physiology|ileum]] is not easily accessible. Exploratory laparotomy and full thickness biopsy may be preferred at times. |
| − | + | ||
| − | |||
| − | |||
==Treatment== | ==Treatment== | ||
===Dietary modification=== | ===Dietary modification=== | ||
| − | An elimination diet should be instigated. The patient should be fed strictly on a novel protein source | + | *An elimination diet should be instigated. The patient should be fed strictly on a novel protein source that had not previously been exposed to. Clinical signs should resolve within 1-2 weeks. The patient should ideally be rechallenged to demonstrate a true dietary [[Hypersensitivity - WikiBlood|hypersensitivity]]. |
| − | Folate and cobalamin supplementation may be required if the levels are subnormal. | + | *Folate and cobalamin supplementation may be required if the levels are subnormal. |
===Antimicrobials=== | ===Antimicrobials=== | ||
| − | [[Nitroimidazoles| | + | *[[Nitroimidazoles|metronidazole]] can be given for 3-4 weeks |
| − | The mucosal damage caused by IBD may decrease the animal's ability to manage intestinal flora, resulting in secondary | + | *This may be suitable for mild to moderate cases, and especially in cats. |
| + | *The mucosal damage caused by IBD may decrease the animal's ability to manage to intestinal flora, resulting in secondary ARD has been reported. | ||
===Immunosuppressive=== | ===Immunosuppressive=== | ||
| − | This should be used if other treatments are inadequate. [[Steroids|Prednisolone]] | + | *This should be used if other treatments are inadequate. |
| + | *[[Steroids|Prednisolone]] | ||
| + | *Azathioprine or Cyclosporine can be given alternatively if the patient is non-responsive or unable to tolerate steroid. | ||
==Prognosis== | ==Prognosis== | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | == | + | =Pathology= |
| − | + | ===Introduction=== | |
| + | |||
| + | * Inflammatory bowel disease will result in malabsorption and in many cases, chronic diarrhoea. | ||
| + | * The small and/or [[Large Intestine - Anatomy & Physiology|large intestine]]s are affected. | ||
| + | ** The site determines whether diarrhoea is present. | ||
| + | * Additionally, can get extraintestinal abnormalities | ||
| + | ** Cholangiohepatitis | ||
| + | ** Nephritis | ||
| + | ** Pancreatitis | ||
| + | ** Polyarthropathy | ||
| + | ** Thrombocytopenia (uncommon) | ||
| + | *** Extent of thrombocytopenia not related to duration of IBD or to its resolution. | ||
| + | * The term "inflammatory bowel disease" covers several conditions characterised by the major inflammatory cell(s) present. | ||
| + | ** All have some common features: | ||
| + | *** Thickening of the mucosa. | ||
| + | *** Villus atrophy in advanced disease. | ||
| + | *** Significant inflammatory infiltrate in the mucosa and sometimes deeper layers. | ||
| + | |||
| + | |||
| + | ==Lymphocytic - Plasmacytic Enteritis== | ||
| + | |||
| + | ====Pathology==== | ||
| + | |||
| + | * Hypersensitivity reaction results in increased GIT permeablility and recruitment of inflammatory cells. | ||
| + | * Histologically: | ||
| + | ** Mucosal epithelial-glandular alterations. | ||
| + | ** Variably increased mucosal infiltrate of lymphocytes and plasma cells. | ||
| + | *** In these dogs there is an increase in the number of IgA and IgG containing cells and CD3+ T-cells. | ||
| + | **** Can develop into lymphoma. | ||
| + | *** Changes in the relative and absolute numbers of plasma cells and lymphocytes have been associated with IBD in humans. | ||
| + | |||
| + | ==Eosinophilic Enteritis== | ||
| + | |||
| + | * Can be either focal or diffuse. | ||
| + | |||
| + | ===Focal=== | ||
| + | |||
| + | * A disease of young dogs. | ||
| + | * Associated with [[Toxocara canis|''Toxocara canis'']] infection. | ||
| + | ** Pin-head sized white nodules can be seen under the serosa in the bowel. | ||
| + | *** Consist of of eosinophils and occasionally macrophages and plasma cells. | ||
| + | *** Can sometimes see [[Toxocara canis|''Toxocara'']] larvae in the nodules. | ||
| + | |||
| + | ===Diffuse=== | ||
| + | |||
| + | * Seen in the dog, cat and horse. | ||
| + | * Idiopathic | ||
| + | * Has a predilection for German Shepherd Dogs, but also occcurs in other breeds of dogs and in cats. | ||
| + | ** Recurrent episodes of diarrhoea with tissue and circulatory eosinophilia. | ||
| + | *** Eosinophils heavily infiltrate all layers of stomach and intestines. | ||
| + | **It has been suggested that it is a type of hypersensitivity reaction. | ||
| + | |||
| + | |||
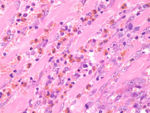
| + | [[Image:eosinophilic_enteritis.jpg|thumb|right|150px|Eosinophilic enteritis - horse(Courtesy of Susan Rhind, University of Edinburgh)]] | ||
| + | |||
| + | ==Idiopathic Eosinophilic Enteritis== | ||
| + | |||
| + | *Dairy cows | ||
| + | *Thickened [[Small Intestine - Anatomy & Physiology|small intestine]], mesenteric lymphadenopathy. | ||
| + | *[[Small Intestine - Anatomy & Physiology|small intestine]] | ||
| + | **Marked oedema, lymphangiectasia without vasculitis | ||
| + | **Eosinophilic infiltration of the intestinal mucosa (esp. at the villus tip). | ||
| + | *Eosinophilic enteritis associated with hypoalbuminaemia, hypoglobulinaemia and eosinophilia in other species. The extent of the biochemical changes reflect the extent of the histological changes in the gut. | ||
| + | **Not so in these cases. | ||
| + | *In man, eosinophilic enteritis called if ≥20 eosinophils per HPF in the gut. | ||
| + | *No cause in these cattle found … although loweed ingestion can cause eosinophilic gastroenteritis. | ||
| + | |||
| + | [Idiopathic eosinophilic enteritis in 4 cattle. JAVMA (1998) 212 258-61] | ||
| + | |||
| + | ==Granulomatous enteritis== | ||
| + | |||
| + | * Seen mainly in the dog. | ||
| + | ** Also in the cat and horse | ||
| + | * Idiopathic. | ||
| + | * Granulomatous inflammation | ||
| + | ** Macrophages and giant cells, but also [[Neutrophils - WikiBlood|neutrophils]], eosinophils, lymphocytes and plasma cells. | ||
| + | |||
| + | ==Idiopathic colitis== | ||
| − | + | * Affects the dog. | |
| − | + | ==Histiocytic Ulcerative Colitis== | |
| + | * Occurs in the dog and cat . | ||
| + | ** In the dog, animals less than two years old are most likely to be affected. | ||
| + | *** Particularly the boxer and French bulldog. | ||
| + | * Produces soft faeces containing mucous and blood. | ||
| − | + | ===Pathology=== | |
| − | + | * Produces raised ulcerative nodules in the colon. | |
| + | ** Due to an macrophage infiltration of the mucosa and submucosa | ||
| + | *** Macrophages are filled with PAS positive material. | ||
| + | *** Electron microscopy demonstrates macrophages to be filled with [[Escherichia coli|''E.coli'']] antigen. | ||
| + | * Accompanying lymphadenopathy. | ||
| − | |||
| − | |||
| − | + | =References= | |
| − | [[Category: | + | *Ettinger, S.J. and Feldman, E. C. (2000) '''Textbook of Veterinary Internal Medicine Diseases of the Dog and Cat Volume 2''' (Fifth Edition) ''W.B. Saunders Company''. |
| − | [[Category: | + | *Hall, E.J, Simpson, J.W. and Williams, D.A. (2005) '''BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition)''' ''BSAVA'' |
| + | *Nelson, R.W. and Couto, C.G. (2009) '''Small Animal Internal Medicine (Fourth Edition)''' ''Mosby Elsevier''. | ||
| + | [[Category:Intestine_-_Inflammatory_Pathology]][[Category:Dog]] | ||
Revision as of 22:47, 1 June 2010
| This article is still under construction. |
Signalment
- No sex predisposition
- There are contraditions with regard to age predisposition
Description
Inflammatory bowel disease (IBD) is an idiopathic group of disorders characterised by intestinal inflammatory changes, associated with persistent or recurrent gastrointestinal signs. IBD can affect any part of the intestines and is classified according to the predominant cellular inflammatory infiltration. Several histological types have been recognised, which are:
There is no underlying cause of IBD in 75% of cases. They are thought to reflect an exaggerated or inappropriate response by the immune system to dietary, bacterial or self-antigens. IBD is a diagnosis of exclusion. Other differential diagnoses have to be investigated and ruled out before a diagnosis of IBD can be made.
Diagnosis
Clinical Signs
- Vomiting; very common in cat, more common than diarrhoea
- Diarrhoea; very common in dog, more common than vomiting, usually small intestinal
- Weight loss; nearly all cases of chronic small intestinal disease
- Variable appetite; increased or decreased which relates to severity
- Lethargy; common in severe cases
- Anorexia; common in severe cases
- Antibiotic responsive diarrhoea
- Abdominal discomfort or pain
- Excessive borborygmi
- Haematemesis or haematochezia (more severe cases)
- Hypoproteinaemia or ascites
- Thickened intestinal loop
Laboratory Tests
Haematology
- Neutrophilia ± mild left shift in LPE
- Eosinophilia
- Not always present in EE
Biochemistry
- Panhypoproteinaemia
- Hypocholesterolaemia
- Mild increased in liver enzymes, secondary to intestinal inflammation
Other Tests
- Faecal analysis should be carried out to rule out parasitic causes such as whipworms, hookworms and Giardia.
- Serum folate level decreases with proximal small intestinal inflammation.
- Serum cobalamin level decreases with distal small intestinal inflammation.
Diagnostic Imaging
Radiography
Plain radiography is used to evaluate for anatomic abnormalities. Contrast study is only valuable if there is a severe mucosal disease.
Ultrasonography
Ultrasonography may reveal mesenteric lymphadenopathy and thickening of the intestinal wall.
Histopathology
A biopsy of the intestine is required for a definitive diagnosis of IBD. A non-invasive biopsy may be taken via endoscopy. However, this limits where the samples can be taken from as the jejunum and ileum is not easily accessible. Exploratory laparotomy and full thickness biopsy may be preferred at times.
Treatment
Dietary modification
- An elimination diet should be instigated. The patient should be fed strictly on a novel protein source that had not previously been exposed to. Clinical signs should resolve within 1-2 weeks. The patient should ideally be rechallenged to demonstrate a true dietary hypersensitivity.
- Folate and cobalamin supplementation may be required if the levels are subnormal.
Antimicrobials
- metronidazole can be given for 3-4 weeks
- This may be suitable for mild to moderate cases, and especially in cats.
- The mucosal damage caused by IBD may decrease the animal's ability to manage to intestinal flora, resulting in secondary ARD has been reported.
Immunosuppressive
- This should be used if other treatments are inadequate.
- Prednisolone
- Azathioprine or Cyclosporine can be given alternatively if the patient is non-responsive or unable to tolerate steroid.
Prognosis
Pathology
Introduction
- Inflammatory bowel disease will result in malabsorption and in many cases, chronic diarrhoea.
- The small and/or large intestines are affected.
- The site determines whether diarrhoea is present.
- Additionally, can get extraintestinal abnormalities
- Cholangiohepatitis
- Nephritis
- Pancreatitis
- Polyarthropathy
- Thrombocytopenia (uncommon)
- Extent of thrombocytopenia not related to duration of IBD or to its resolution.
- The term "inflammatory bowel disease" covers several conditions characterised by the major inflammatory cell(s) present.
- All have some common features:
- Thickening of the mucosa.
- Villus atrophy in advanced disease.
- Significant inflammatory infiltrate in the mucosa and sometimes deeper layers.
- All have some common features:
Lymphocytic - Plasmacytic Enteritis
Pathology
- Hypersensitivity reaction results in increased GIT permeablility and recruitment of inflammatory cells.
- Histologically:
- Mucosal epithelial-glandular alterations.
- Variably increased mucosal infiltrate of lymphocytes and plasma cells.
- In these dogs there is an increase in the number of IgA and IgG containing cells and CD3+ T-cells.
- Can develop into lymphoma.
- Changes in the relative and absolute numbers of plasma cells and lymphocytes have been associated with IBD in humans.
- In these dogs there is an increase in the number of IgA and IgG containing cells and CD3+ T-cells.
Eosinophilic Enteritis
- Can be either focal or diffuse.
Focal
- A disease of young dogs.
- Associated with Toxocara canis infection.
- Pin-head sized white nodules can be seen under the serosa in the bowel.
- Consist of of eosinophils and occasionally macrophages and plasma cells.
- Can sometimes see Toxocara larvae in the nodules.
- Pin-head sized white nodules can be seen under the serosa in the bowel.
Diffuse
- Seen in the dog, cat and horse.
- Idiopathic
- Has a predilection for German Shepherd Dogs, but also occcurs in other breeds of dogs and in cats.
- Recurrent episodes of diarrhoea with tissue and circulatory eosinophilia.
- Eosinophils heavily infiltrate all layers of stomach and intestines.
- It has been suggested that it is a type of hypersensitivity reaction.
- Recurrent episodes of diarrhoea with tissue and circulatory eosinophilia.
Idiopathic Eosinophilic Enteritis
- Dairy cows
- Thickened small intestine, mesenteric lymphadenopathy.
- small intestine
- Marked oedema, lymphangiectasia without vasculitis
- Eosinophilic infiltration of the intestinal mucosa (esp. at the villus tip).
- Eosinophilic enteritis associated with hypoalbuminaemia, hypoglobulinaemia and eosinophilia in other species. The extent of the biochemical changes reflect the extent of the histological changes in the gut.
- Not so in these cases.
- In man, eosinophilic enteritis called if ≥20 eosinophils per HPF in the gut.
- No cause in these cattle found … although loweed ingestion can cause eosinophilic gastroenteritis.
[Idiopathic eosinophilic enteritis in 4 cattle. JAVMA (1998) 212 258-61]
Granulomatous enteritis
- Seen mainly in the dog.
- Also in the cat and horse
- Idiopathic.
- Granulomatous inflammation
- Macrophages and giant cells, but also neutrophils, eosinophils, lymphocytes and plasma cells.
Idiopathic colitis
- Affects the dog.
Histiocytic Ulcerative Colitis
- Occurs in the dog and cat .
- In the dog, animals less than two years old are most likely to be affected.
- Particularly the boxer and French bulldog.
- In the dog, animals less than two years old are most likely to be affected.
- Produces soft faeces containing mucous and blood.
Pathology
- Produces raised ulcerative nodules in the colon.
- Due to an macrophage infiltration of the mucosa and submucosa
- Macrophages are filled with PAS positive material.
- Electron microscopy demonstrates macrophages to be filled with E.coli antigen.
- Due to an macrophage infiltration of the mucosa and submucosa
- Accompanying lymphadenopathy.
References
- Ettinger, S.J. and Feldman, E. C. (2000) Textbook of Veterinary Internal Medicine Diseases of the Dog and Cat Volume 2 (Fifth Edition) W.B. Saunders Company.
- Hall, E.J, Simpson, J.W. and Williams, D.A. (2005) BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition) BSAVA
- Nelson, R.W. and Couto, C.G. (2009) Small Animal Internal Medicine (Fourth Edition) Mosby Elsevier.