Difference between revisions of "Leptospira"
| Line 1: | Line 1: | ||
| − | {{ | + | {{review}} |
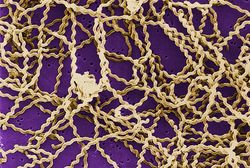
[[File:Leptospira.jpg|right|thumb|250px|<small><center> Leptospira Scanning Micrograph. (Rob Weyant 1998, WikiMedia Commons)</center></small>]] | [[File:Leptospira.jpg|right|thumb|250px|<small><center> Leptospira Scanning Micrograph. (Rob Weyant 1998, WikiMedia Commons)</center></small>]] | ||
| Line 28: | Line 28: | ||
[[Category:To_Do_-_AimeeHicks]][[Category:Leptospiraceae]] | [[Category:To_Do_-_AimeeHicks]][[Category:Leptospiraceae]] | ||
| − | [[Category: | + | [[Category:Expert_Review]] |
Revision as of 13:46, 20 July 2010
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
Overview
Leptospira is from the family,Leptospiraceae which is a spirochaetes species. Leptospira is a motile, helical bacteria found in aquatic environments. It causes Leptospirosis in all animals, which can range from mild urogenital tract infections to systemic diseases. The organisms persist in the kidney tubules or genital tracts of carrier animals and are shed in urine. Transmission occurs via direct contact. Maintenance hosts may transmit the infection to incidental hosts, which are less susceptible to infection, but develop serious disease. Leptospira may cause severe systemic disease, resulting in enteritis.
Pathogenesis
The pathogenesis of Leptospira depends on virulence of the bacteria and susceptibility of the host. Leptospires invade tissues through moist skin or via mucous membranes, aided by their motility. They may invade via receptor-mediated endocytosis and then pass through the body via the blood stream. Antibodies clear the organisms from the blood stream after about 10 days of infection.
The organisms may persist in the renal tubules, uterus, eye or meninges. They evade phagocytosis possibly via macrophage apoptosis and damage red blood cell membranes and endothelial and liver cells, leading to haemolytic anaemia, jaundice, haemoglobin pigmentation, haemoglobinuria and haemorrhage in acute leptospirosis.
Diagnosis
Leptospira can be diagnosed by clinical signs and history of exposure. Dark-field microscopy of urine may detect organisms as may isolation from blood or urine by culture or animal inoculation. The fluorescent antibody technique can be used for identification in tissues. Silver impregnation, molecular techniques such as PCR and Serology using microscopic agglutination test or ELISA can also be used.