Difference between revisions of "Hepatic Lipidosis"
Fiorecastro (talk | contribs) |
JamesSwann (talk | contribs) |
||
| (31 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
| + | {{review}} | ||
| − | + | {{cat}} | |
| − | + | {{dog}} | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | ==== | + | ==Signalment== |
| + | *Indoor cats are more prone to primary hepatic lipidosis. | ||
| + | *Middle-aged cats are more prone. | ||
| − | |||
| − | + | ==Description== | |
| + | Hepatic lipidosis is the derangement of lipid and protein metabolism, which occurs in cats and dogs, but more clinically significant in cats. It is important to differentiate primary or idiopathic hepatic lipidosis from secondary hepatic lipidosis. | ||
| − | + | '''Primary or idiopathic hepatic lipidosis''' is most recognised in obese indoor cats following anorexia. It is the most common hepatic disease in North America but it is also becoming more common in Europe. It is an acute hepatopathy with a large accumulation of lipid in hepatocytes, causing the liver to lose its function. The mortality rate is high unless the disease is treated aggressively. The pathogenesis includes a number of factors: | |
| + | *excessive lipid mobilisation which is induced by anorexia, illness or stress. | ||
| + | *deficiency of dietary proteins and other nutrients, which reduces the liver's capacity to produce transport proteins and to metabolise fat. Recognised nutrient deficiencies include arginine, carnitine, taurine and methionine. | ||
| + | *disturbances in the neurohormonal control of appetite resulting in inappropriate anorexia. | ||
| − | + | '''Secondary hepatic lipidosis''' is a neuroendocrine response in dogs and cats to other diseases for example, [[Pancreatitis - Dog and Cat|pacreatitis]], diabetes mellitus, [[Inflammatory Bowel Disease|inflammatory bowel disease]] and primary hyperlipidaemia. Secondary hepatic lipidosis is therefore less closely correlated with obesity and be seen in normal or even thin cats. | |
| − | |||
| − | + | ==Diagnosis== | |
| + | ===Clinical Signs=== | ||
| + | *Often obese cats following a sudden starvation | ||
| + | *Anorexia and lethargy | ||
| + | *[[Icterus|Jaundice]] | ||
| + | *[[Hepatic Encephalopathy #Clinical Signs|Hepatic Encephalopathy]] | ||
| + | *[[Diarrhoea|Diarrhoea]] (sometimes) | ||
| + | *Palpable hepatomegaly (sometimes) | ||
| + | *Coagulopathies (sometimes) | ||
| − | + | ===Laboratory Tests=== | |
| + | ====Biochemistry==== | ||
| + | *Markedly increased level in alanine | ||
| + | *Low gamma-glutamyltransferase (GGT) concentration | ||
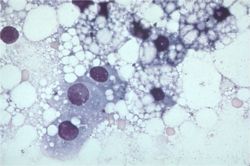
| − | + | [[Image:Hepatic lipidosis histology.jpg|thumb|right|250px|Hepatic Lipidosis Histology - Copyright Karin Allenspach's lecture RVC]] | |
| − | ==== Radiography ==== | + | ===Diagnostic Imaging=== |
| + | ====Radiography==== | ||
| + | Abdominal radiography shows a marked hepatomegaly. | ||
| − | + | ====Ultrasonography==== | |
| + | On ultrasound, an enlarged and diffusely hyperechoeic liver is seen. | ||
| − | |||
| − | |||
| − | == | + | ==Histopathology== |
| − | + | Fine needle aspirate of the liver is normally sufficient for a diagnosis. Cytology demonstrates hepatocytes swollen with lipid. | |
| − | + | Biopsy and culture of the liver tissue is always indicated to determine the underlying cause of the disease. | |
| − | |||
| − | + | ==Treatment== | |
| + | *Intensive treatment of cats is required for best outcome | ||
| − | == | + | ===Nutritional support=== |
| − | + | *For a period of 4 - 6 weeks. | |
| − | + | *This is the most important treatment in hepatic lipidosis. It is vital to ensure that the diet is of adequate calorific content with an increase in protein content. Specific nutrients such as arginine, taurine, or carnitine may also be added. | |
| + | *This can be done via different feeding systems such as naso-oesophageal tube, oesophagostomy tube, gastrostomy tube. | ||
| − | + | ===[[Hepatic Encephalopathy #Medical Management|Hepatic Encephalopathy]]=== | |
| + | *Treat this if presented. | ||
| − | === | + | ===Gastrointestinal drugs=== |
| + | *Anti-emetics and porkinetics such as [[Gastroprotective Drugs #Histamine (H2) Receptor Antagonists|ranitidine]] and [[Drugs Acting on the Intestines#Drugs Acting on 5-HT4 Receptors|metoclopromide]] if vomiting for delayed gastric emptying is present | ||
| − | + | ===Fluid therapy=== | |
| + | *Intravenous fluid therapy in early stages of disease. | ||
| + | *Blood glucose and electrolytes especially potasium and phosphate should be monitored. | ||
| − | === | + | ===Coagulopathy=== |
| + | *Vitamin K supplement may be required if coagulopathy is significant. | ||
| − | |||
| − | + | ==Prognosis== | |
| + | This is dependent on the underlying cause. If treated appropriately, 85% of severely affected animals will recover. | ||
| − | |||
| − | + | ==References== | |
| + | *Ettinger, S.J. and Feldman, E. C. (2000) '''Textbook of Veterinary Internal Medicine Diseases of the Dog and Cat Volume 2''' (Fifth Edition) ''W.B. Saunders Company''. | ||
| + | *Hall, E.J, Simpson, J.W. and Williams, D.A. (2005) '''BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition)''' ''BSAVA'' | ||
| + | *Nelson, R.W. and Couto, C.G. (2009) '''Small Animal Internal Medicine (Fourth Edition)''' ''Mosby Elsevier''. | ||
| + | *Tilley, L. P. & Smith, F. W. K. (2007) '''Blackwell's Five-minute Veterinary Consult: Canine & Feline (Fourth Edition)''' ''Blackwell Publishing'' | ||
| − | = | + | =From Pathology= |
| − | |||
| − | == | + | ==Hepatic lipidosis - fatty liver syndrome== |
| + | *also known as lipid mobilisation syndrome | ||
| + | *any persistent abnormal accumulation of fat within [[Liver - Anatomy & Physiology|liver]] cells | ||
| + | *associated with | ||
| + | **dietary factors: obesity and starvation | ||
| + | **increased demand for energy: pregnancy, lactation, and starvation in physiological states | ||
| + | **''[[DM|Diabetes mellitus]]'', ketosis, and pregnancy toxaemia in pathological conditions | ||
| + | **abnormal hepatocytic function: prevents fatty acids from forming complexes with proteins to form low density lipoproteins for secretion into the blood | ||
| + | *enlarged [[Liver - Anatomy & Physiology|liver]] with round edges | ||
| + | *lightish yellow in colour | ||
| + | *cut surface is uniform and greasy to handle | ||
| − | + | The following are several important specific diseases in which fatty change is the main finding: | |
| − | |||
| − | + | ===associated with obesity=== | |
| + | Overfeeding will lead to the accumulation of fat in the [[Liver - Anatomy & Physiology|liver]] | ||
| − | == | + | This is a normal physiological function but if a sudden check in dietary intake is imposed it may tip such an animal into serious ill health |
| + | ====Bovine==== | ||
| + | *fat cow syndrome (extreme form of fatty liver) | ||
| + | *occurs in well-fed dairy cows a few days postpartum | ||
| + | *an excessive accumulation of liver fat without being able to export it from the [[Liver - Anatomy & Physiology|liver]] (during late dry period and early lactation) | ||
| + | *amount of fat deposited influenced by: | ||
| + | **Body Condition Score (how fat the cow is) | ||
| + | **Milk Yield (energy requirement) | ||
| + | **Appetite (low in fat cows) | ||
| + | *triggered by various conditions: | ||
| + | **abomasal displacement | ||
| + | **mastitis | ||
| + | **metritis | ||
| + | **retained [[Gestation -Placenta - Anatomy & Physiology|placenta]] | ||
| + | *can be fatal due to [[Liver - Anatomy & Physiology|liver]] failure (up to 25% has been reported) | ||
| − | + | =====Clinical===== | |
| + | *cow is sick | ||
| + | *poor appetite | ||
| + | *excessive weight loss | ||
| + | *downer | ||
| + | *high incidence of post parturient disease | ||
| − | == | + | =====Gross===== |
| − | + | *fat infiltration of [[Liver - Anatomy & Physiology|liver]] | |
| − | + | *enlarged | |
| − | + | *rounded edges | |
| − | + | *pale yellow colour | |
| − | + | *friable | |
| − | + | NB: will also get fat infiltration of [[Liver - Anatomy & Physiology|liver]] in cows which have not been eating for several days so interpret carefully | |
| − | |||
| − | |||
| − | + | =====Prevention===== | |
| − | + | *dry off cows at correct BCS (up to 3.5) | |
| − | + | *do not adjust BCS during dry period | |
| + | *do not starve fat dry cows | ||
| + | *maintain appetite over late dry and calving period to prevent excessive weight loss and fat mobilisation | ||
| + | *use transistion diet | ||
| − | == | + | ====Feline==== |
| + | *feline fatty [[Liver - Anatomy & Physiology|liver]] syndrome | ||
| + | *fairly similar and associated solely with obesity | ||
| + | *diagnosis on cytology/histopathology | ||
| + | *Survival rate is only 50-60% | ||
| + | *Pathophysiology: | ||
| + | **Incompletely understood | ||
| + | **Obese cats that lose 30-40% of body weight exhibit a similar syndrome to naturally occurring hepatic lipidosis | ||
| + | **But many causative factors for naturally occurring hepatic lipidosis: | ||
| + | ***Peripheral lipolysis secondary to absolute or relative lack of insulin | ||
| + | ***Protein-calories malnutrition | ||
| + | ***Amino acid deficiencies – inability to synthesize apolipoproteins necessary to mobilize hepatic fat | ||
| + | ***Deficiency of lipotrophic compounds | ||
| + | ***Error of fatty acid oxidation | ||
| + | ***Hepatic perioxosomal damage due to oxidative stress | ||
| + | *Cats with hepatic lipidosis have higher nonesterified fatty acids (NEFAs) compared to controls and those with cholangiohepatitis | ||
| + | **NEFAs are derived from lipolysis of fat stores and enter the [[Liver - Anatomy & Physiology|liver]] | ||
| + | **They are oxidized in the [[Liver - Anatomy & Physiology|liver]] for energy or converted to phospholipids or cholesterol or reesterified to triglycerides | ||
| + | **Limited increase in lipoprotein synthesis and secretion of triglycerides in VLDLs | ||
| + | **Capacity for increase in oxidation by mitochondria and ketone body synthesis is low | ||
| + | **Rate of fatty acid esterification to triglycerides is not limited so can lead to a marked increase in the accumulation of stored hepatic triglycerides | ||
| + | *Also all triglyceride accumulation in hepatocytes in these cats comes from mobilized peripheral adipose stores during nutritional stress | ||
| + | **high levels of triglyceride concentrations in the [[Liver - Anatomy & Physiology|liver]] will cause: | ||
| + | ***severe periacinar necrosis | ||
| + | ***jaundice | ||
| + | ***hepatic encephalopathy | ||
| + | ***high mortality rate | ||
| + | *Lipolysis – under control of hormone-sensitive lipase hydrolyses triglycerides to NEFAs and glycerol | ||
| + | **Insulin – inhibits it | ||
| + | *Catecholamines (eg: released in stress, etc – neural input), glucocorticoids, thyroxine, GH and glucagons all promote lipolysis | ||
| + | *Lower insulin levels in cats with hepatic lipidosis or cholangiohepatitis compared to controls; and lower glucogon:insulin ratio in diseased cats | ||
| + | **But as not lipidosis specific, not likely to be the main factor involved | ||
| + | *Higher serum triglycerides in lipidotic cats compared to controls | ||
| − | + | [[Hyperlipidaemia - Equine ]] | |
| − | |||
| − | |||
| − | |||
| + | [[White Liver Disease - Ovine]] | ||
| − | + | ===associated with derangement of carbohydrate metabolism=== | |
| + | ====[[Diabetes Mellitus]]==== | ||
| + | ====[[Ketosis]]==== | ||
| + | ===associated with anoxia and toxaemia=== | ||
| + | ====anoxia==== | ||
| + | *passive congestion | ||
| + | *anaemias | ||
| + | ====toxaemia==== | ||
| + | *toxins absorbed from the gut interfere with many stages of triglyceride metabolism | ||
| − | + | [[Category:Liver_-_Degenerative_Pathology]][[Category:Cat]][[Category:Cattle]] | |
| − | |||
| − | [[Category: | + | [[Category:To_Do_-_James]] |
| − | |||
Revision as of 17:28, 22 July 2010
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
Signalment
- Indoor cats are more prone to primary hepatic lipidosis.
- Middle-aged cats are more prone.
Description
Hepatic lipidosis is the derangement of lipid and protein metabolism, which occurs in cats and dogs, but more clinically significant in cats. It is important to differentiate primary or idiopathic hepatic lipidosis from secondary hepatic lipidosis.
Primary or idiopathic hepatic lipidosis is most recognised in obese indoor cats following anorexia. It is the most common hepatic disease in North America but it is also becoming more common in Europe. It is an acute hepatopathy with a large accumulation of lipid in hepatocytes, causing the liver to lose its function. The mortality rate is high unless the disease is treated aggressively. The pathogenesis includes a number of factors:
- excessive lipid mobilisation which is induced by anorexia, illness or stress.
- deficiency of dietary proteins and other nutrients, which reduces the liver's capacity to produce transport proteins and to metabolise fat. Recognised nutrient deficiencies include arginine, carnitine, taurine and methionine.
- disturbances in the neurohormonal control of appetite resulting in inappropriate anorexia.
Secondary hepatic lipidosis is a neuroendocrine response in dogs and cats to other diseases for example, pacreatitis, diabetes mellitus, inflammatory bowel disease and primary hyperlipidaemia. Secondary hepatic lipidosis is therefore less closely correlated with obesity and be seen in normal or even thin cats.
Diagnosis
Clinical Signs
- Often obese cats following a sudden starvation
- Anorexia and lethargy
- Jaundice
- Hepatic Encephalopathy
- Diarrhoea (sometimes)
- Palpable hepatomegaly (sometimes)
- Coagulopathies (sometimes)
Laboratory Tests
Biochemistry
- Markedly increased level in alanine
- Low gamma-glutamyltransferase (GGT) concentration
Diagnostic Imaging
Radiography
Abdominal radiography shows a marked hepatomegaly.
Ultrasonography
On ultrasound, an enlarged and diffusely hyperechoeic liver is seen.
Histopathology
Fine needle aspirate of the liver is normally sufficient for a diagnosis. Cytology demonstrates hepatocytes swollen with lipid. Biopsy and culture of the liver tissue is always indicated to determine the underlying cause of the disease.
Treatment
- Intensive treatment of cats is required for best outcome
Nutritional support
- For a period of 4 - 6 weeks.
- This is the most important treatment in hepatic lipidosis. It is vital to ensure that the diet is of adequate calorific content with an increase in protein content. Specific nutrients such as arginine, taurine, or carnitine may also be added.
- This can be done via different feeding systems such as naso-oesophageal tube, oesophagostomy tube, gastrostomy tube.
Hepatic Encephalopathy
- Treat this if presented.
Gastrointestinal drugs
- Anti-emetics and porkinetics such as ranitidine and metoclopromide if vomiting for delayed gastric emptying is present
Fluid therapy
- Intravenous fluid therapy in early stages of disease.
- Blood glucose and electrolytes especially potasium and phosphate should be monitored.
Coagulopathy
- Vitamin K supplement may be required if coagulopathy is significant.
Prognosis
This is dependent on the underlying cause. If treated appropriately, 85% of severely affected animals will recover.
References
- Ettinger, S.J. and Feldman, E. C. (2000) Textbook of Veterinary Internal Medicine Diseases of the Dog and Cat Volume 2 (Fifth Edition) W.B. Saunders Company.
- Hall, E.J, Simpson, J.W. and Williams, D.A. (2005) BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition) BSAVA
- Nelson, R.W. and Couto, C.G. (2009) Small Animal Internal Medicine (Fourth Edition) Mosby Elsevier.
- Tilley, L. P. & Smith, F. W. K. (2007) Blackwell's Five-minute Veterinary Consult: Canine & Feline (Fourth Edition) Blackwell Publishing
From Pathology
Hepatic lipidosis - fatty liver syndrome
- also known as lipid mobilisation syndrome
- any persistent abnormal accumulation of fat within liver cells
- associated with
- dietary factors: obesity and starvation
- increased demand for energy: pregnancy, lactation, and starvation in physiological states
- Diabetes mellitus, ketosis, and pregnancy toxaemia in pathological conditions
- abnormal hepatocytic function: prevents fatty acids from forming complexes with proteins to form low density lipoproteins for secretion into the blood
- enlarged liver with round edges
- lightish yellow in colour
- cut surface is uniform and greasy to handle
The following are several important specific diseases in which fatty change is the main finding:
associated with obesity
Overfeeding will lead to the accumulation of fat in the liver
This is a normal physiological function but if a sudden check in dietary intake is imposed it may tip such an animal into serious ill health
Bovine
- fat cow syndrome (extreme form of fatty liver)
- occurs in well-fed dairy cows a few days postpartum
- an excessive accumulation of liver fat without being able to export it from the liver (during late dry period and early lactation)
- amount of fat deposited influenced by:
- Body Condition Score (how fat the cow is)
- Milk Yield (energy requirement)
- Appetite (low in fat cows)
- triggered by various conditions:
- abomasal displacement
- mastitis
- metritis
- retained placenta
- can be fatal due to liver failure (up to 25% has been reported)
Clinical
- cow is sick
- poor appetite
- excessive weight loss
- downer
- high incidence of post parturient disease
Gross
- fat infiltration of liver
- enlarged
- rounded edges
- pale yellow colour
- friable
NB: will also get fat infiltration of liver in cows which have not been eating for several days so interpret carefully
Prevention
- dry off cows at correct BCS (up to 3.5)
- do not adjust BCS during dry period
- do not starve fat dry cows
- maintain appetite over late dry and calving period to prevent excessive weight loss and fat mobilisation
- use transistion diet
Feline
- feline fatty liver syndrome
- fairly similar and associated solely with obesity
- diagnosis on cytology/histopathology
- Survival rate is only 50-60%
- Pathophysiology:
- Incompletely understood
- Obese cats that lose 30-40% of body weight exhibit a similar syndrome to naturally occurring hepatic lipidosis
- But many causative factors for naturally occurring hepatic lipidosis:
- Peripheral lipolysis secondary to absolute or relative lack of insulin
- Protein-calories malnutrition
- Amino acid deficiencies – inability to synthesize apolipoproteins necessary to mobilize hepatic fat
- Deficiency of lipotrophic compounds
- Error of fatty acid oxidation
- Hepatic perioxosomal damage due to oxidative stress
- Cats with hepatic lipidosis have higher nonesterified fatty acids (NEFAs) compared to controls and those with cholangiohepatitis
- NEFAs are derived from lipolysis of fat stores and enter the liver
- They are oxidized in the liver for energy or converted to phospholipids or cholesterol or reesterified to triglycerides
- Limited increase in lipoprotein synthesis and secretion of triglycerides in VLDLs
- Capacity for increase in oxidation by mitochondria and ketone body synthesis is low
- Rate of fatty acid esterification to triglycerides is not limited so can lead to a marked increase in the accumulation of stored hepatic triglycerides
- Also all triglyceride accumulation in hepatocytes in these cats comes from mobilized peripheral adipose stores during nutritional stress
- high levels of triglyceride concentrations in the liver will cause:
- severe periacinar necrosis
- jaundice
- hepatic encephalopathy
- high mortality rate
- high levels of triglyceride concentrations in the liver will cause:
- Lipolysis – under control of hormone-sensitive lipase hydrolyses triglycerides to NEFAs and glycerol
- Insulin – inhibits it
- Catecholamines (eg: released in stress, etc – neural input), glucocorticoids, thyroxine, GH and glucagons all promote lipolysis
- Lower insulin levels in cats with hepatic lipidosis or cholangiohepatitis compared to controls; and lower glucogon:insulin ratio in diseased cats
- But as not lipidosis specific, not likely to be the main factor involved
- Higher serum triglycerides in lipidotic cats compared to controls
associated with derangement of carbohydrate metabolism
Diabetes Mellitus
Ketosis
associated with anoxia and toxaemia
anoxia
- passive congestion
- anaemias
toxaemia
- toxins absorbed from the gut interfere with many stages of triglyceride metabolism