Difference between revisions of "Platelet Abnormalities"
| (10 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
[[Platelet|Platelets]] (or thrombocytes) are responsible for primary haemostasis by the formation of a temporary platelet plug that initially seals any breach to a blood vessel wall. These breaches are then sealed more completely by the formation of a fibrin clot induced by the coagulation factor cascade. | [[Platelet|Platelets]] (or thrombocytes) are responsible for primary haemostasis by the formation of a temporary platelet plug that initially seals any breach to a blood vessel wall. These breaches are then sealed more completely by the formation of a fibrin clot induced by the coagulation factor cascade. | ||
===Terminology=== | ===Terminology=== | ||
| − | *'''Thrombocytopaenia''' refers to low absolute numbers of platelets. | + | *'''Thrombocytopaenia''' refers to low absolute numbers of platelets. [[Immune Mediated Thrombocytopaenia|Immune-mediated thrombocytopaenia]] (ITP) is one common cause of thrombocytopaenia and this may be a primary or secondary disease. |
*'''Thrombocytopathia''' refers to platelets that are unable to function adequately. | *'''Thrombocytopathia''' refers to platelets that are unable to function adequately. | ||
*'''Thrombocytosis''' refers to an increase in the blood platelet concentration above the normal level. | *'''Thrombocytosis''' refers to an increase in the blood platelet concentration above the normal level. | ||
| Line 21: | Line 21: | ||
===Causes of increased platelet destruction=== | ===Causes of increased platelet destruction=== | ||
| + | *'''[[Immune Mediated Thrombocytopaenia|Immune-mediated thrombocytopaenia]]''' is a common autoimmune disease that leads to the production of antibodies against platelets and their subsequent destruction by cells of the [[Monocytes|monocyte]] phagocyte system (MPS). | ||
*'''Infectious diseases''' that cause destruction of platelets include [[Bovine Viral Diarrhoea Virus|bovine viral diarrhoea (BVD)]], [[Classical Swine Fever|classical swine fever]] and [[Infectious Canine Hepatitis|infectious canine hepatitis]]. The parasites [[Ehrlichia platys|''Anaplasma platys'']], [[Ehrlichia phagocytophila|''Anaplasma phagocytophilum'']] and ''[[Ehrlichia canis]]'' may also cause infectious thrombocytopaenia. Any severe bacterial infection, including those caused by [[:Category:Staphylococcus species|''Staphylococci'']] and the Gram negative bacteria that produce endotoxins (e.g. [[:Category:Pseudomonas and Burkholderia species|''Pseudomonas sp.'']] or [[Salmonella|''Salmonella sp.'']]) may also result in the destruction of platelets. | *'''Infectious diseases''' that cause destruction of platelets include [[Bovine Viral Diarrhoea Virus|bovine viral diarrhoea (BVD)]], [[Classical Swine Fever|classical swine fever]] and [[Infectious Canine Hepatitis|infectious canine hepatitis]]. The parasites [[Ehrlichia platys|''Anaplasma platys'']], [[Ehrlichia phagocytophila|''Anaplasma phagocytophilum'']] and ''[[Ehrlichia canis]]'' may also cause infectious thrombocytopaenia. Any severe bacterial infection, including those caused by [[:Category:Staphylococcus species|''Staphylococci'']] and the Gram negative bacteria that produce endotoxins (e.g. [[:Category:Pseudomonas and Burkholderia species|''Pseudomonas sp.'']] or [[Salmonella|''Salmonella sp.'']]) may also result in the destruction of platelets. | ||
| − | |||
===Causes of platelet sequestration=== | ===Causes of platelet sequestration=== | ||
| Line 29: | Line 29: | ||
===Artefactual or spurious thrombocytopaenia=== | ===Artefactual or spurious thrombocytopaenia=== | ||
*'''Cavalier King Charles spaniels''' have a genetic abnormality which produces a small number of giant platelets (macrothrombocytes) in the circulation with a corresponding reduction in free platelets; they do not suffer from bleeding disorders as they maintain a similar total platelet mass as do dogs of other breeds. Automated blood counts will include the macrothrombocytes in the white or red cell count and the apparent thrombocytopenia will be exaggerated. | *'''Cavalier King Charles spaniels''' have a genetic abnormality which produces a small number of giant platelets (macrothrombocytes) in the circulation with a corresponding reduction in free platelets; they do not suffer from bleeding disorders as they maintain a similar total platelet mass as do dogs of other breeds. Automated blood counts will include the macrothrombocytes in the white or red cell count and the apparent thrombocytopenia will be exaggerated. | ||
| − | |||
*If venepuncture is traumatic (using small viens with excessive suction or patient agitation) '''platelet clumps''' may form and these will not be counted by automated machines. The presence of clumps can be investigated by making a blood smear and examining the feathered edge for large agglomerations of platelets. Time, temperature and contact with glass can also cause clumping of platelets once the sample has been taken. | *If venepuncture is traumatic (using small viens with excessive suction or patient agitation) '''platelet clumps''' may form and these will not be counted by automated machines. The presence of clumps can be investigated by making a blood smear and examining the feathered edge for large agglomerations of platelets. Time, temperature and contact with glass can also cause clumping of platelets once the sample has been taken. | ||
| Line 47: | Line 46: | ||
*'''Splenic contraction''' which pushes sequestered platelets into the circulation. This phenomenon is especially marked in '''horses''' which have a muscular splenic capsule. | *'''Splenic contraction''' which pushes sequestered platelets into the circulation. This phenomenon is especially marked in '''horses''' which have a muscular splenic capsule. | ||
*'''Splenectomy''' prevents the sequestration of platelets in the spleen, resulting in consistently increased levels of platelets. | *'''Splenectomy''' prevents the sequestration of platelets in the spleen, resulting in consistently increased levels of platelets. | ||
| − | *As part of a response to [[ | + | *As part of a response to [[Anaemia - Introduction|anaemia]] a '''reactive thrombocytosis''' is often documented and this may precede signs of regeneration. |
Pathological | Pathological | ||
| Line 54: | Line 53: | ||
==Clinical Significance== | ==Clinical Significance== | ||
Other than essential thrombocythaemia, thrombocytosis has no clinical importance except as an indicator of another disease process. Thrombocytopaenia and thrombocytopathia both result in reductions in the effectiveness of primary haemostasis, producing bleeding disorders. Since bleeding points are usually sealed by a fibrin clot, disorders of primary haemostasis tend to be less severe than those caused by deficiencies of the coagulation factors. Common signs of a disorder of primary haemostasis include: | Other than essential thrombocythaemia, thrombocytosis has no clinical importance except as an indicator of another disease process. Thrombocytopaenia and thrombocytopathia both result in reductions in the effectiveness of primary haemostasis, producing bleeding disorders. Since bleeding points are usually sealed by a fibrin clot, disorders of primary haemostasis tend to be less severe than those caused by deficiencies of the coagulation factors. Common signs of a disorder of primary haemostasis include: | ||
| − | *Petechial or ecchymotic [[Haemorrhage|haemorrhages]] on the skin or mucous membranes. | + | *Petechial or ecchymotic [[Haemorrhage - Pathology|haemorrhages]] on the skin or mucous membranes. |
| − | *[[Haemorrhage|Haemorrhages]] from the mucous membranes, producing haematuria, haematochezia, haematemesis, haemoptysis and melaena. | + | *[[Haemorrhage - Pathology|Haemorrhages]] from the mucous membranes, producing haematuria, haematochezia, haematemesis, haemoptysis and melaena. |
| − | *[[ | + | *[[Anaemia - Introduction|Anaemia]] with a reactive [[Neutrophilia|neutrophilia]] and [[Monocytosis|monocytosis]] if the haemorrhage is severe. |
| − | Severe platelet deficiencies may be managed with transfusions of whole blood or, in the USA, with transfusions of platelet cryoprecipitate | + | Severe platelet deficiencies may be managed with transfusions of whole blood or, in the USA, with transfusions of platelet cryoprecipitate. With both techniques however, it is likely that the transfused platelets have only a short half life in the recipient. |
| − | The use of Vincristine (a drug also used in chemotherapy for neoplasia) has been advocated in cases of thrombocytopaenia as it | + | The use of Vincristine (a drug also used in chemotherapy for neoplasia) has been advocated in cases of thrombocytopaenia as it causes the release of immature platelets from the bone marrow. |
| − | + | ==Literature Search== | |
| − | | | + | [[File:CABI logo.jpg|left|90px]] |
| + | |||
| + | |||
| + | Use these links to find recent scientific publications via CAB Abstracts (log in required unless accessing from a subscribing organisation). | ||
| + | <br><br><br> | ||
| + | [http://www.cabdirect.org/search.html?q=title%3A%28thrombocytopenia%29+OR+title%3A%28thrombocytopaenia%29&fq=sc%3A%22ve%22 Thrombocytopaenia publications] | ||
[http://www.cabdirect.org/search.html?q=title%3A%28thrombocytopathia%29+ Thrombocytopathia publications] | [http://www.cabdirect.org/search.html?q=title%3A%28thrombocytopathia%29+ Thrombocytopathia publications] | ||
[http://www.cabdirect.org/search.html?q=title%3A%28thrombocytosis%29&fq=sc%3A%22ve%22 Thrombocytosis publications] | [http://www.cabdirect.org/search.html?q=title%3A%28thrombocytosis%29&fq=sc%3A%22ve%22 Thrombocytosis publications] | ||
| − | |||
| − | |||
[[Category:Haemorrhagic Diseases]] | [[Category:Haemorrhagic Diseases]] | ||
[[Category:Haematology Changes]] | [[Category:Haematology Changes]] | ||
| − | |||
| − | |||
Revision as of 10:42, 15 October 2010
Introduction
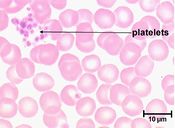
Platelets (or thrombocytes) are responsible for primary haemostasis by the formation of a temporary platelet plug that initially seals any breach to a blood vessel wall. These breaches are then sealed more completely by the formation of a fibrin clot induced by the coagulation factor cascade.
Terminology
- Thrombocytopaenia refers to low absolute numbers of platelets. Immune-mediated thrombocytopaenia (ITP) is one common cause of thrombocytopaenia and this may be a primary or secondary disease.
- Thrombocytopathia refers to platelets that are unable to function adequately.
- Thrombocytosis refers to an increase in the blood platelet concentration above the normal level.
Thrombocytopaenia and thrombocytopathia lead to disorders of primary haemostasis but, in general, this is less serious than the disorders of secondary haemostasis caused by deficiencies in the coagulation factors.
Thrombocytopaenia
Thrombocytopaenia is a common haematological abnormality as platelet numbers are subject to fluctuation in a number of diseases. Care should be taken, however to ensure that this finding is not caused by an artefact of sampling where platelet clumps have formed. The normal blood platelet concentration of the dog is 175-500x10^9; a tendency to bleed following an insult such as venepuncture can be observed if levels fall below 50x10^9 and spontaneous haemorrhage is observed when levels fall below 30x10^9. Acute thrombocytopenia is more likley to give rise to clinical signs than more chronically developed low platelet numbers.
Reductions in platelet numbers may be caused by a failure to produce adequate amounts in the bone marrow during megakaryopoiesis, or an increased destruction of existing platelets or sequestration of platelets outside of the circulation.
Causes of bone marrow suppression
- Aplastic anaemia which can be caused by the ingestion of bracken or administration of oestrogens, chloramphenicol or sulphonamide antibiotics. Prolonged use of phenylbutazone or salicylates may cause the same disease.
- Infectious diseases that reduce stem cell function include canine distemper, canine parvovirus and feline panleucopaenia virus.
- Myelophthisis is the displacement of the normal cell lines of the bone marrow by another cell or tissue type which may also reduce the function of the megakaryocytes. Diseases in this category include myelofibrosis and immunoproliferative or myeloproliferative neoplastic disease.
- Radiotherapy or myelosuppressive chemotherapy may cause reversible bone marrow suppression.
Causes of increased platelet destruction
- Immune-mediated thrombocytopaenia is a common autoimmune disease that leads to the production of antibodies against platelets and their subsequent destruction by cells of the monocyte phagocyte system (MPS).
- Infectious diseases that cause destruction of platelets include bovine viral diarrhoea (BVD), classical swine fever and infectious canine hepatitis. The parasites Anaplasma platys, Anaplasma phagocytophilum and Ehrlichia canis may also cause infectious thrombocytopaenia. Any severe bacterial infection, including those caused by Staphylococci and the Gram negative bacteria that produce endotoxins (e.g. Pseudomonas sp. or Salmonella sp.) may also result in the destruction of platelets.
Causes of platelet sequestration
Diseases that cause sequestration of platelets usually involve some enlargement of the spleen, as this is the major organ where platelets are stored outside of the circulation. A common example would be haemangiosarcoma of the spleen and liver. Splenic enlargement under general anaesthesia maintained with agents such as barbiturates and phenothiazines can also lead to sequestration of platelets.
Artefactual or spurious thrombocytopaenia
- Cavalier King Charles spaniels have a genetic abnormality which produces a small number of giant platelets (macrothrombocytes) in the circulation with a corresponding reduction in free platelets; they do not suffer from bleeding disorders as they maintain a similar total platelet mass as do dogs of other breeds. Automated blood counts will include the macrothrombocytes in the white or red cell count and the apparent thrombocytopenia will be exaggerated.
- If venepuncture is traumatic (using small viens with excessive suction or patient agitation) platelet clumps may form and these will not be counted by automated machines. The presence of clumps can be investigated by making a blood smear and examining the feathered edge for large agglomerations of platelets. Time, temperature and contact with glass can also cause clumping of platelets once the sample has been taken.
Thrombocytopathia
Defects in platelet function may be congenital or acquired in association with a number of diseases. Congenital thrombocytopathias are rare inherited diseases which are characterised by defects in platelet adhesiveness, aggregation or factor release. The defects are usually associated with particular breeds, such as Chediak-Higashi syndrome in blue smoke Persian cats.
Causes of acquired thrombocytopathia include:
- Infection with Angiostrongylus vasorum, the canine lungworm, which also causes a consumptive coagulopathy.
- Hypergammaglobulinaemia as occurs with multiple myeloma and some forms of (B-cell) lymphoma may affect platelet function.
- Administration of large volumes of some colloid solutions.
- Administration of certain pharmaceutical products, including non-steroidal anti-inflammatory drugs and cephalosporins.
Thrombocytosis
Increased platelet number above normal levels may occur due to physiological or pathological processes.
Physiological causes include:
- Splenic contraction which pushes sequestered platelets into the circulation. This phenomenon is especially marked in horses which have a muscular splenic capsule.
- Splenectomy prevents the sequestration of platelets in the spleen, resulting in consistently increased levels of platelets.
- As part of a response to anaemia a reactive thrombocytosis is often documented and this may precede signs of regeneration.
Pathological
- Essential thrombocythaemia is a rare myeloproliferative disease that results in the excessive production of platelets which function abnormally. Affected animals suffer from bouts of spontaneous haemorrhage.
Clinical Significance
Other than essential thrombocythaemia, thrombocytosis has no clinical importance except as an indicator of another disease process. Thrombocytopaenia and thrombocytopathia both result in reductions in the effectiveness of primary haemostasis, producing bleeding disorders. Since bleeding points are usually sealed by a fibrin clot, disorders of primary haemostasis tend to be less severe than those caused by deficiencies of the coagulation factors. Common signs of a disorder of primary haemostasis include:
- Petechial or ecchymotic haemorrhages on the skin or mucous membranes.
- Haemorrhages from the mucous membranes, producing haematuria, haematochezia, haematemesis, haemoptysis and melaena.
- Anaemia with a reactive neutrophilia and monocytosis if the haemorrhage is severe.
Severe platelet deficiencies may be managed with transfusions of whole blood or, in the USA, with transfusions of platelet cryoprecipitate. With both techniques however, it is likely that the transfused platelets have only a short half life in the recipient.
The use of Vincristine (a drug also used in chemotherapy for neoplasia) has been advocated in cases of thrombocytopaenia as it causes the release of immature platelets from the bone marrow.
Literature Search
Use these links to find recent scientific publications via CAB Abstracts (log in required unless accessing from a subscribing organisation).
Thrombocytopaenia publications