Difference between revisions of "Hyperadrenocorticism"
Fiorecastro (talk | contribs) |
|||
| (28 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
| + | [[Image:Cushings alopecia.jpg|right|thumb|200px|<small><center>'''Cushings Alopecia'''. Courtesy of A. Jefferies</center></small>]] | ||
| + | Also known as '''''Cushings disease''' | ||
| + | ==Introduction== | ||
| + | Hyperadrenocorticism is a common disease of adrenal hyperfunction that is seen most commonly in the dog. There are three known causes of the adrenal hyperfunction: dysfunction of the pituitary gland, dysfunction of the adrenal glands and iatrogenic administration of corticosteroids. | ||
| + | ==Pituitary Dependant Hyperadrenocorticism== | ||
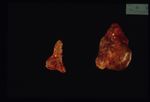
| + | [[Image:Chromophobe adenoma.jpg|right|thumb|150px|<small><center>'''Chromophobe Adenoma'''. Courtesy of A. Jefferies</center></small>]] | ||
| + | 80-85% cases of Cushings disease show bilateral adrenal hyperplasia due to excess stimuation by ACTH. There is a failure of the negative feedback mechanism at the level of the pituitary and so ACTH is produced in an unregulated fashion. This is thought to occur due to a functional chromophobe cell (Produces ACTH and MSH) neoplasia, although visible macroadenomas are only found in 10-15% cases with this aetiology. Most cases are therefore thought to be microadenomas and may be visualised by histopathological staining of the pituitary. | ||
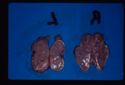
| + | [[Image:Nodular hyperplasia.jpg|right|thumb|150px|<small><center>'''Adrenal Nodular Hyperplasia'''. Courtesy of A. Jefferies</center></small>]] | ||
| − | + | Grossly the adrenals have an irregular surface with protruding nodules of cortical tissue; the hyperplased zona fasciculata cells. | |
| − | == | + | ==Adrenal Dependant Hyperadrenocorticism== |
| − | [[Image: | + | [[Image:Adrenal neoplasia.jpg|right|thumb|150px|<small><center>'''Adrenal Neoplasia'''. Courtesy of A. Jefferies</center></small>]] |
| − | + | Approximately 15% all cases of Cushings disease fit into this category, which is primarily a neoplastic abnormality of the adrenal glands; approximately 50% are benign and 50% are malignant. | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | == | + | ==Iatrogenic Hyperadrenocorticism== |
| + | This is created by the administration of parenteral corticosteroids.In these cases adrenal atrophy is induced as the administered steroids have a negative feedback effect on the pituitary and normal ACTH release is inhibited. | ||
| − | + | ===Pathophysiology=== | |
| + | The clinical signs of Cushings disease are brought about by excess glucocorticoids, particularly cortisol. | ||
| + | [[Image:Cushings alopecia.jpg|right|thumb|150px|<small><center>'''Cushings Alopecia'''. Courtesy of A. Jefferies</center></small>]] | ||
| − | + | *'''[[Liver - Anatomy & Physiology|Liver]]''': Cortisol induces enzymes to increase gluconeogenesis leading to '''hyperglycaemia''' in Cushings patients. The [[Pancreas - Anatomy & Physiology|pancreas]] attempts to maintain normal blood glucose by producing increasing amount of insulin. Eventually the [[Pancreas - Anatomy & Physiology|pancreas]] is exhausted inducing a diabetic state. | |
| + | *'''Muscle''': Cortisol stimulates protein catabolism for gluconeogenesis so patients exhibit '''muscle weakness'''. | ||
| + | *'''Skin''': Again protein catabolism and weakness giving '''poor wound healing'''. | ||
| + | **'''Calcinosis cutis''': Collagen damage due to protein catabolism allows the deposition of calcium in the skin. Calcium acts as a foreign body producing a ''granulomatous reaction''. | ||
| + | **MSH production stimulates the pigmentation of the skin with melanin. | ||
| + | **Cortisol inhibits the growth phase of the hair cycle (ANAGEN) so hair growth stops. When epilated over areas of high friction there will be '''bilaterally symmetric non-pruritic alopecia'''. | ||
| + | *'''Fat''': Lipolysis is stimulated by cortisol to provide precursors for gluconeogenesis. Seen clinically as a redistribution of fat to the abdomen and back of the neck; '''Pot-bellied appearance'''. | ||
| + | *'''Immune system''': Cortisol is '''anti-inflammatory''' by a number of mechanisms E.g. stabilising lysosomal membranes. The circulation will contain fewer lymphocytes and eosinophils. | ||
| + | *'''Kidney''': Cortisol interferes with ADH action on the kidney resulting in '''polyuria and polydipsia'''. | ||
| − | === | + | ===Diagnosis=== |
| − | + | *'''ACTH Stimulation test''': Measure Cortisol before and 30-60 mins after i/v ''Synacthen''. Positive result is initially high cortisol followed by a markedly elevated cortisol after stimulation (>600nmol/l). | |
| + | Adrenal dependant disease may be unresponsive to ACTH. | ||
| + | *'''Low dose dexamethasone test''': Sample before and 3 and 8 hours after i/v dexamethasone at 0.01mg/kg. Normal and dogs with pituitary dependant disase show suppression of cortisol production to <50% at 3 hours whereas dogs with adrenal dependant disease have high cortisol levels which are not suppressed. | ||
| + | *'''High dose dexamethasone test''': Distinguishes pituitary and adrenal dependant disease once Cushings has been diagnosed. Dexamethasone dose is 0.1mg/kg. Pituitary dependant disease will show suppression of cortisol production due to negative feedback at the pituitary whereas adrenal dependant disease will not. | ||
| − | === | + | ===Treatment=== |
| + | [[Image:Mitotane therapy.jpg|right|thumb|125px|<small><center>'''Post-Mitotane Therapy'''. Courtesy of A. Jefferies</center></small>]] | ||
| − | + | *'''Mitotane''': Selectively destroys the zona fasciculata and zona reticularis while sparing the zona glomerulosa. Need to use an induction dose followed by a maintenance dose. | |
| + | *'''Trilostane''': Synthetic steroid analogue. Competitively inhibits enzymes of steroid synthesis. | ||
| + | *'''L-Deprenyl''': Monoamine oxidase inhibitor. Increases dopamine input to hypothalamus and pituitary and so inhibits ACTH secretion. | ||
| − | + | Pituitary tumours may be treated with ''radiotherapy'' or ''surgery''. | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | Pituitary tumours may be treated with ''radiotherapy'' or ''surgery''. | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Revision as of 18:53, 13 November 2010
Also known as Cushings disease
Introduction
Hyperadrenocorticism is a common disease of adrenal hyperfunction that is seen most commonly in the dog. There are three known causes of the adrenal hyperfunction: dysfunction of the pituitary gland, dysfunction of the adrenal glands and iatrogenic administration of corticosteroids.
Pituitary Dependant Hyperadrenocorticism
80-85% cases of Cushings disease show bilateral adrenal hyperplasia due to excess stimuation by ACTH. There is a failure of the negative feedback mechanism at the level of the pituitary and so ACTH is produced in an unregulated fashion. This is thought to occur due to a functional chromophobe cell (Produces ACTH and MSH) neoplasia, although visible macroadenomas are only found in 10-15% cases with this aetiology. Most cases are therefore thought to be microadenomas and may be visualised by histopathological staining of the pituitary.
Grossly the adrenals have an irregular surface with protruding nodules of cortical tissue; the hyperplased zona fasciculata cells.
Adrenal Dependant Hyperadrenocorticism
Approximately 15% all cases of Cushings disease fit into this category, which is primarily a neoplastic abnormality of the adrenal glands; approximately 50% are benign and 50% are malignant.
Iatrogenic Hyperadrenocorticism
This is created by the administration of parenteral corticosteroids.In these cases adrenal atrophy is induced as the administered steroids have a negative feedback effect on the pituitary and normal ACTH release is inhibited.
Pathophysiology
The clinical signs of Cushings disease are brought about by excess glucocorticoids, particularly cortisol.
- Liver: Cortisol induces enzymes to increase gluconeogenesis leading to hyperglycaemia in Cushings patients. The pancreas attempts to maintain normal blood glucose by producing increasing amount of insulin. Eventually the pancreas is exhausted inducing a diabetic state.
- Muscle: Cortisol stimulates protein catabolism for gluconeogenesis so patients exhibit muscle weakness.
- Skin: Again protein catabolism and weakness giving poor wound healing.
- Calcinosis cutis: Collagen damage due to protein catabolism allows the deposition of calcium in the skin. Calcium acts as a foreign body producing a granulomatous reaction.
- MSH production stimulates the pigmentation of the skin with melanin.
- Cortisol inhibits the growth phase of the hair cycle (ANAGEN) so hair growth stops. When epilated over areas of high friction there will be bilaterally symmetric non-pruritic alopecia.
- Fat: Lipolysis is stimulated by cortisol to provide precursors for gluconeogenesis. Seen clinically as a redistribution of fat to the abdomen and back of the neck; Pot-bellied appearance.
- Immune system: Cortisol is anti-inflammatory by a number of mechanisms E.g. stabilising lysosomal membranes. The circulation will contain fewer lymphocytes and eosinophils.
- Kidney: Cortisol interferes with ADH action on the kidney resulting in polyuria and polydipsia.
Diagnosis
- ACTH Stimulation test: Measure Cortisol before and 30-60 mins after i/v Synacthen. Positive result is initially high cortisol followed by a markedly elevated cortisol after stimulation (>600nmol/l).
Adrenal dependant disease may be unresponsive to ACTH.
- Low dose dexamethasone test: Sample before and 3 and 8 hours after i/v dexamethasone at 0.01mg/kg. Normal and dogs with pituitary dependant disase show suppression of cortisol production to <50% at 3 hours whereas dogs with adrenal dependant disease have high cortisol levels which are not suppressed.
- High dose dexamethasone test: Distinguishes pituitary and adrenal dependant disease once Cushings has been diagnosed. Dexamethasone dose is 0.1mg/kg. Pituitary dependant disease will show suppression of cortisol production due to negative feedback at the pituitary whereas adrenal dependant disease will not.
Treatment
- Mitotane: Selectively destroys the zona fasciculata and zona reticularis while sparing the zona glomerulosa. Need to use an induction dose followed by a maintenance dose.
- Trilostane: Synthetic steroid analogue. Competitively inhibits enzymes of steroid synthesis.
- L-Deprenyl: Monoamine oxidase inhibitor. Increases dopamine input to hypothalamus and pituitary and so inhibits ACTH secretion.
Pituitary tumours may be treated with radiotherapy or surgery.