|
|
| (13 intermediate revisions by 2 users not shown) |
| Line 1: |
Line 1: |
| − | {{Navigation | + | {{Navigation2 |
| | |title = Interpretation of Intra-Oral Radiography | | |title = Interpretation of Intra-Oral Radiography |
| | |categories = [[:Category:Intra-Oral Radiography|'''Intra-Oral Radiography''']] | | |categories = [[:Category:Intra-Oral Radiography|'''Intra-Oral Radiography''']] |
| − | |text = Whilst interpreting dental radiographs they should be viewed on a '''viewing box''' with minimal peripheral light and preferably using magnification. It is recommended to radiograph the '''contralateral structures for comparative purposes'''. | + | |text = For interpretation dental radiographs should be viewed using a '''viewing box''' with minimal peripheral light and preferably using magnification. It is recommended to radiograph the '''contralateral structures for comparative purposes'''. |
| | | | |
| | |content = | | |content = |
| − | :[[Normal Intra-Oral Radiographic Anatomy|Normal Radiographic Anatomy]] | + | :[[Normal Intra-Oral Radiographic Anatomy - Small Animal|Normal Radiographic Anatomy]] |
| − | :[[Dental Developmental Abnormalities - Radiographic Interpretation|Developmental Abnormalities]] | + | :[[Radiographic Interpretation of Dental Developmental Abnormalities - Small Animal|Interpreting Developmental Abnormalities]] |
| − | :[[]] | + | :[[Radiographic Interpretation of Periodontal Disease - Small Animal|Interpreting Periodontal Disease]] |
| − | |image = Dog's Joy.jpg | + | :[[Radiographic Interpretation of Endodontic Disease - Small Animal|Interpreting Endodontic Disease]] |
| | + | :[[Radiographic Interpretation of Tooth Resorption - Small Animal|Interpreting Tooth Resorption]] |
| | + | :[[Radiographic Interpretation of Dental Traumatic Injuries - Small Animal|Interpreting Traumatic Injuries]] |
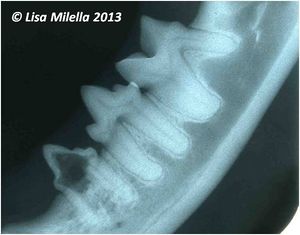
| | + | |image = Cat mandibular radiograph 1.jpg |
| | |resources = | | |resources = |
| | }} | | }} |
| | | | |
| − | [[Category:To Do - Dentistry]]
| |
| − | [[Category:Intra-Oral Radiography]]
| |
| | | | |
| | + | {{Lisa Milella written |
| | + | |date = 1 October 2014}} |
| | | | |
| | + | {{Waltham}} |
| | | | |
| | + | {{OpenPages}} |
| | | | |
| − | | + | [[Category:Intra-Oral Radiography]] |
| − | | + | [[Category:Waltham reviewed]] |
| − | | |
| − | | |
| − | | |
| − | | |
| − | ==Interpreting Periodontal Disease==
| |
| − | Dental radiographs assist in the assessment of periodontitis by providing information regarding alveolar bone loss. They complement, not replace, the clinical examination. The clinical examination is essential for evaluating the soft tissue changes such as inflammation, gingival recession, and periodontal pocket formation. Clinical examination will provide evidence of mild bone loss, such as a Grade I furcation exposure, prior to changes being apparent on a dental radiograph. The dental radiograph is a two-dimensional image, and the morphology of an infrabony defect will be determined on clinical examination rather than on radiographic evaluation.
| |
| − | <br><br>
| |
| − | Widening of the periodontal ligament space, decreased alveolar bone density, and bone loss are all radiographic changes associated with periodontitis.<br><br>
| |
| − | Terms used to describe the alveolar bone loss associated with periodontitis include:
| |
| − | *Alveolar margin bone loss
| |
| − | *Furcation bone loss
| |
| − | *Horizontal bone loss
| |
| − | *Vertical bone loss
| |
| − | *Combination of horizontal and vertical bone loss<br><br>
| |
| − | Dental radiographs made for the evaluation of early alveolar bone loss should not be overexposed because this may result in “burn-out” of the alveolar marginal and interdental marginal bone. Dental radiographs should be made at the correct exposure or slightly under-exposed to provide the best detail when evaluating for early bone loss.<br><br>
| |
| − | Alveolar bone loss may be mild, moderate, or severe, the significance of the bone loss will depend on the amount of attachment loss and the teeth involved. Furcation bone loss is bone loss that occurs in the area where multirooted teeth divide. Approximately 30% to 40% of the furcation bone must be lost before it will be evident on a radiograph. A Grade 3 furcation exposure is complete loss of bone in the furcation area, and this may be identified readily on most two-rooted teeth but may be more difficult to determine on the three-rooted maxillary molar teeth.<br><br>
| |
| − | Crowded and malpositioned teeth make it more difficult to diagnose alveolar margin and furcation bone loss from a radiograph. Interdental alveolar bone loss and furcation bone loss, especially when mild, are often easier to identify radiographically than alveolar bone loss superimposed over the tooth roots.<br><br>
| |
| − | Severe periodontitis may result in secondary complications such as external root resorption and endodontic disease or weakening of the mandible with potential for fracture.
| |
| − | <br><br>
| |
| − |
| |
| − | ==Interpreting Endodontic Disease==
| |
| − | Radiographs may provide information about the presence, nature, and severity of periapical and root pathology. This information is essential for the diagnosis of endodontic disease as well as for the prognosis of its treatment. Radiographs do not provide direct information about pulp health; however, many of the effects of pulp pathology are radiographically visible.<br><br>
| |
| − | Clinical findings that may indicate the presence of endodontic disease include a fractured tooth with exposure of the pulp chamber, a discolored tooth, or an intraoral or extraoral draining fistula. Except in the obvious case of a direct pulp exposure, a definitive diagnosis of endodontic pathology is difficult to make based only on clinical examination of veterinary patients due to the limitations of pulp testing and lack of patient input. <br><br>
| |
| − | Radiographs should be made of teeth that are fractured, close to a draining fistula, intrinsically discolored, anomalous, or compromised from periodontal disease to determine the extent of the problem and to evaluate the endodontic and periradicular health.<br><br>
| |
| − | Dental radiographs can be misleading and unreliable. Early endodontic disease may not show any radiographic abnormalities, while superimposed anatomy can mimic endodontic disease on a radiograph of a healthy tooth. Despite these limitations, dental radiographs continue to be the best tool available to evaluate endodontic health in veterinary patients. The site of exit does not always directly correlate to the problem tooth. Radiographs are needed to determine which tooth is involved.<br><br>
| |
| − | | |
| − | ==Radiographic Signs of Endodontic Disease==
| |
| − | Inflammation caused by endodontic disease affects the surrounding bone and teeth, resulting in changes that can be radiographically detected. Radiographs that are meant to evaluate the periapical tissues should include the entire root tip and surrounding bone, be well positioned to avoid elongation, foreshortening, angulation, or distortion of the image. <br><br>
| |
| − | Radiographic signs of endodontic disease that are associated with the tissues around tooth roots include:
| |
| − | *Increased width of the apical radiolucent periodontal ligament space
| |
| − | *Loss of the radiopaque lamina dura at the apex or other portals of exit such as lateral canals
| |
| − | *Diffuse periapical radiolucency with indistinct borders that may indicate an acute abscess
| |
| − | *Clearly evident periapical radiolucency with distinct borders that is evidence of a more chronic lesion
| |
| − | *Diffuse area of radiopacity where low-grade chronic inflammation results in sclerosing osteitis
| |
| − | *Changes in the trabecular bone pattern around the root apex
| |
| − | <br>
| |
| − | Radiographic signs of endodontic disease that are associated with the tooth itself include:
| |
| − | *Root tip resorption
| |
| − | *Internal root or crown resorption. Inflammation of the pulp can cause internal resorption
| |
| − | *External root resorption. Inflammation in the periodontal ligament can cause external root resorption
| |
| − | *Arrested tooth maturation (pulp necrosis). Pulp necrosis causes the opposite effect, arresting any further dentin formation or tooth maturation. The result is a tooth that appears radiographically less mature (wider root canal space) than the adjacent teeth.
| |
| − | *Accelerated apparent tooth maturation (pulpitis). Pulpitis can also result in formation of tertiary, or reparative dentin on the walls of the pulp cavity. Pulpitis that is generalized over a section of a root canal creates the radiographic effect of a narrower canal in that section, giving the appearance of a more mature tooth. The extreme of this can manifest as “pulp cavity obliteration,” a radiographic term that describes an inability to identify sections of, or the entire, pulp space.
| |
| − | <br>
| |
| − | Endodontic lesions in cats appear radiographically similar to those in dogs.<br><br>
| |
| − | Lucencies That Can Mimic Endodontic Lesions:<br><br>
| |
| − | Apical radiographs can be challenging to interpret due to the two-dimensional depiction of complicated anatomy that combines trabecular (spongy) bone, compact bone, soft tissue, and air spaces all projected at various angles and configurations. Other confusing lucencies and opacities can be created by the summation effect of superimposed structures, projecting overlying anatomy in a way that makes it appear to be associated with a tooth root or its supporting bone. These can include bony foraminae, bony fissures, bony canals, and trabeculae. Many nonpathological lucencies, opacities, and apparent deviations from normal can be distinguished from true lesions by comparison with a radiograph of the contralateral tooth.
| |
| − | <br><br>
| |
| − | Two categories of insult that most commonly cause endodontic disease are bacterial infection and dental trauma. <br><br>
| |
| − | Bacteria can also enter the endodontic system of a nontraumatized tooth through extension of periodontal disease. If the periodontal epithelial attachment migrates apically to an endodontic vascular entrance such as a lateral canal, furcation communication, or the apical foramen or delta, then the pulp could become infected. This is referred to as a primary periodontal lesion with secondary endodontic involvement (it has also been referred to as a “perio-endo lesion”). Apical and radicular LEOs can dissect coronally along the side of the root to exit in the sulcus, creating a primary endodontic lesion with secondary periodontal disease (has also been referred to as an “endo-perio lesion”). The bony defects around a tooth with primary endodontic disease and concurrent but unrelated periodontal disease can meet to form a combined periodontal and endodontic lesion.<br><br>
| |
| − | Pulp inflammation and necrosis can also result from deep dental caries with extension of the bacterial infection to the pulp.<br><br>
| |
| − | Blunt trauma can cause pulp hemorrhage and endodontic disease even when the tooth crown does not fracture. Although the pulp has some ability to heal after mild trauma, the most common result of pulp trauma is irreversible pulpitis even when there is no bacterial contamination of the pulp. <br><br>
| |
| − | Radiographic signs depend on the pulp response:
| |
| − | *Arrested development of a tooth (wide pulp with thin dentin)
| |
| − | *Pulp calcification
| |
| − | *Internal resorption
| |
| − | *External resorption
| |
| − | *Wide periodontal ligament space
| |
| − | *Periradicular radiolucencies
| |
| − | *Discontinuous lamina dura
| |
| − | *Root fractures
| |
| − | <br>
| |
| − | ==Tooth Resorption==
| |
| − | ==Feline Tooth Resorption==
| |
| − | Radiographs of affected teeth often show root resorption that is far more advanced than expected. Every tooth with a clinical TR should be radiographically evaluated, not only to determine severity but also to determine the type of root changes that are occurring and to identify concurrent pathology. Multiple teeth are often involved in affected individuals. Therefore, full mouth radiographs of all teeth may be indicated when a patient is diagnosed with TR. Some practitioners recommend full mouth radiographs of all feline patients to identify pathology that is not clinically apparent.<br><br>
| |
| − | '''Types'''<br>
| |
| − | Radiographs of teeth affected with TRs show distinct changes. The roots of some affected teeth seem to “disappear” as they lose radiodense root tissue at a similar rate to the simultaneously occurring osseous repair, effectively making the roots appear to blend with the surrounding bone. The periodontal ligament and structural details are lost. Other TRs retain areas of normal radiodensity interspersed with radiolucencies caused by resorption and do not lose the detail of the periodontal ligament space and root structures in those areas not directly undergoing resorption. Areas of root resorption are often patchy, remaining radiolucent because the lost root substance is not replaced by reparative tissue. This type of TR also commonly demonstrates concurrent periodontal or endodontic disease.
| |
| − | <br><br>
| |
| − | Lesions in which the roots are not replaced by bone-dense tissue are termed type 1 lesions while those in which the roots are replaced and appear to disappear are type 2 lesions . Both types of lesion can be found in the same individual cat, and even in the same tooth with one root appearing to be type 1 and the other root appearing to be a type 2 . It is unknown if this is a stage of severity in which the root or region with the appearance of a type 1 lesion might have eventually progressed to become a type 2 lesion.<br><br>
| |
| − | Tooth resorption on the canine teeth of cats often have areas that appear to be combined type 1 and type 2. Over time it becomes more evident on radiographs which areas will be replaced and which are associated with pathology.
| |
| − | <br><br>
| |
| − | '''Stages'''<br>
| |
| − | There are a number of staging systems in the literature for recording the severity or extent of lesions. Of these, the most logical and clear one categorizes TRs by severity according to objective and easily determined observation that places them into stages that may have clinical relevance.
| |
| − |
| |
| − | *Stage 1. A lesion that affects only the cementum and/or marginal enamel but does not involve the dentin. This stage occurs subgingivally where the tooth surface is exposed to cells that can become odontoclasts. It is uncommon to identify TRs at this stage. Stage 1 lesions are not radiographically apparent.
| |
| − | *Stage 2. A lesion that involves the dentin but not the pulp.
| |
| − | *Stage 3. A lesion that involves the pulp. Radiographs may be necessary to evaluate pulp involvement.
| |
| − | *Stage 4. A lesion that has destroyed a significant amount of the crown, weakening the crown and placing it at risk of fracture with only moderate trauma.
| |
| − | *Stage 5. A lesion that has destroyed the entire crown of the tooth. The gingiva has grown over the roots and no tooth material is exposed to the oral cavity.
| |
| − | <br>
| |
| − | Radiographic evaluation allows both the type and stage of a lesion to be determined, both of which can be easily recorded on the patient’s dental chart.
| |
| − | <br><br>
| |
| − | ==Tooth Resorption in Dogs==
| |
| − | Similar to cats and other species, dogs are affected by TRs from both known causes (most commonly periodontal or endodontic infection or inflammation) and from unproved etiology. The (currently) idiopathic TRs are far less prevalent than the feline lesions and appear very similar to the idiopathic type of TRs in cats. Type 1, type 2, and combined TRs are found in dogs, and they can be staged using the same criteria that are used to stage feline TRs.
| |
| − | <br><br>
| |
| − | ==Interpretation of Traumatic Injuries==
| |
| − | Dental radiographs are made to assess traumatic injuries to the teeth, alveolar bone, mandible, maxilla, and TMJ. Depending on the injuries, skull radiographs and computed tomography scans may be recommended for complete evaluation of all injuries.<br><br>
| |
| − | Traumatic injuries often lead to root fractures, loss of tooth crown, and retention of tooth root. Radiographs are made to identify persistent roots and any associated pathology. A crown fracture that exposes the pulp chamber will result in endodontic disease. When this occurs, the extent of pathology should be evaluated with a dental radiograph . Blunt trauma may result in damage to the pulp without fracturing the tooth. A dental radiograph should be made of any tooth that is discolored from pulp hemorrhage.<br><br>
| |
| − | Root fractures with or without concurrent crown fractures occur secondary to trauma and affect the prognosis and treatment of the tooth.<br><br>
| |
| − | Intra-oral radiographs of the mandible and maxilla are useful to determine the extent of jaw fractures and the involvement of tooth roots without superimposition of other structures. Intra-oral radiographs also allow proper treatment planning to avoid damage to tooth structures during the repair of jaw fractures.
| |
| − |
| |
| − | [[Category:To Do - Dentistry]] | |