Difference between revisions of "Hyperthyroidism"
| (12 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
| − | {{ | + | {{OpenPagesTop}} |
| − | + | == Introduction == | |
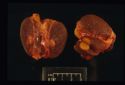
| + | [[Image:thyroid adenoma.jpg|right|thumb|125px|<small><center>'''Thyroid adenoma'''. Courtesy of T. Scase</center></small>]] | ||
| + | This is a disease seen most commonly in the cat. Since it was first diagnosed, the condition has become common in cats and is increasing still in prevalence. It is a very uncommon condition in dogs. Feline hyperthyroidism occurs due to the development of hyperfunctional thyroid nodules, which are benign. Most (>98%) are a functional adenoma of the thyroid gland and many may well be palpable. Rarely they are associated with malignant thyroid neoplasia. | ||
| − | == | + | == Signalment == |
| + | Elderly cats are affected with the average age of onset being around 12-13 years. | ||
| + | == Clinical Signs == | ||
| + | Signs will include '''weight loss despite polyphagia''', which is characteristic of the disease. There may also be increased activity, nervousness (approximately 10% will show apathy), polyuria and polydipsia and heat intolerance and panting. There will also be noticeable tachycardia at around >240 bpm. The coat will appear poorly kept and unkempt. There may be a palpable thyroid mass present. | ||
| − | == | + | == Diagnosis == |
| + | On blood tests, there may be marked to mild elevations of alanine aminotransferase (ALT), aspartate aminotransferase (AST) and alkaline phosphatase (ALP). Approximately 90% of hyperthyroid cats will have an elevation in at least '''one''' of these enzymes. There may also be increases in [[urea]] and [[creatinine]] and occasionally [[azotemia]]. | ||
| + | Specific endocrine tests may show and '''elevated basal plasma T4'''. Increased concentrations are pathognomonic for thyrotoxicosis, although a normal T4 does not mean the disease is not present. In sick or stressed cats, T4 decreases (sick euthyroid syndrome), which can result in a hyperthryoid cat having a low T4. | ||
| − | + | A '''T3 suppression test''' can also be performed which uses the TSH suppressive effect of levels of T3. Normal cats would show a decreased amount of total T4 when T3 is administered, however, hyperthyroid cats would continue producing high levels of T4. | |
| − | + | On echocardiogaphy, a finding that may be linked to hyperthyroidism is a [[Hypertrophic Cardiomyopathy|hypertrophic cardiomyopathy]] due to chronically increased heart rate and activity. | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | == | + | == Treatment == |
| + | Treatment options include '''surgical removal''' of the affected thyroid gland(s). If bilateral it is important to preserve at least one [[Parathyroid Glands - Anatomy & Physiology|parathyroid gland]] to maintain [[calcium]] homeostasis. Although effective, surgical treatment of hyperthyroidism is quite historical. The method of choice is removal via the extracapsular technique. | ||
| − | + | Medical treatment includes the drug '''Carbimazole'''. This interferes with thyroid hormone synthesis and is licensed in the UK. '''Methimazole''' is also used and licensed. Both drugs may produce adverse reactions in around 15% of cases and have the disadvantage of needing cooperative cats and owner compliance. | |
| − | == | + | |
| + | The other therapy is '''radioactive iodine''' therapy. This is useful for intrathoracic thyroid nodules. It is a very simple, effective and safe method of treating hyperthyroidism. The main disadvantages are that the cat needs to be kept in a hospital environment in isolation. There are few, although number are increasing, hospitals in the UK that have this treatment available, and all take referrals. | ||
| + | |||
| + | {{Learning | ||
| + | |flashcards = [[Feline Medicine Q&A 05]] | ||
| + | }} | ||
| + | |||
| + | == References == | ||
| + | Blood, D.C. and Studdert, V. P. (1999) '''Saunders Comprehensive Veterinary Dictionary''' (2nd Edition), ''Elsevier Science.'' | ||
| + | <br> | ||
| + | Church, D. (2008) '''Endocrine System Study Guide, '''''Royal Veterinary College.'' | ||
| + | <br> | ||
| + | Ettinger, S.J. and Feldman, E. C. (2000) '''Textbook of Veterinary Internal Medicine Diseases of the Dog and Cat Volume 2 '''(Fifth Edition), ''W.B. Saunders Company.'' | ||
| + | <br> | ||
| + | Ettinger, S.J, Feldman, E.C. (2005) '''Textbook of Veterinary Internal Medicine '''(6th edition, volume 2),'' W.B. Saunders Company.'' | ||
| + | <br> | ||
| + | Fossum, T. W. et. al. (2007) '''Small Animal Surgery '''(Third Edition), ''Mosby Elsevier.'' | ||
| + | <br> | ||
| + | Nelson, R.W. and Couto, C.G. (2009) '''Small Animal Internal Medicine '''(Fourth Edition),'' Mosby Elsevier. '' | ||
| + | |||
| + | |||
| + | {{review}} | ||
| + | |||
| + | {{OpenPages}} | ||
| + | |||
| + | [[Category:Expert Review - Small Animal]][[Category:Endocrine Diseases - Cat]] | ||
| + | [[Category:Bones - Metabolic Pathology]] | ||
| + | [[Category:Thyroid Gland - Pathology]] | ||
Latest revision as of 12:08, 9 August 2012
Introduction
This is a disease seen most commonly in the cat. Since it was first diagnosed, the condition has become common in cats and is increasing still in prevalence. It is a very uncommon condition in dogs. Feline hyperthyroidism occurs due to the development of hyperfunctional thyroid nodules, which are benign. Most (>98%) are a functional adenoma of the thyroid gland and many may well be palpable. Rarely they are associated with malignant thyroid neoplasia.
Signalment
Elderly cats are affected with the average age of onset being around 12-13 years.
Clinical Signs
Signs will include weight loss despite polyphagia, which is characteristic of the disease. There may also be increased activity, nervousness (approximately 10% will show apathy), polyuria and polydipsia and heat intolerance and panting. There will also be noticeable tachycardia at around >240 bpm. The coat will appear poorly kept and unkempt. There may be a palpable thyroid mass present.
Diagnosis
On blood tests, there may be marked to mild elevations of alanine aminotransferase (ALT), aspartate aminotransferase (AST) and alkaline phosphatase (ALP). Approximately 90% of hyperthyroid cats will have an elevation in at least one of these enzymes. There may also be increases in urea and creatinine and occasionally azotemia.
Specific endocrine tests may show and elevated basal plasma T4. Increased concentrations are pathognomonic for thyrotoxicosis, although a normal T4 does not mean the disease is not present. In sick or stressed cats, T4 decreases (sick euthyroid syndrome), which can result in a hyperthryoid cat having a low T4.
A T3 suppression test can also be performed which uses the TSH suppressive effect of levels of T3. Normal cats would show a decreased amount of total T4 when T3 is administered, however, hyperthyroid cats would continue producing high levels of T4.
On echocardiogaphy, a finding that may be linked to hyperthyroidism is a hypertrophic cardiomyopathy due to chronically increased heart rate and activity.
Treatment
Treatment options include surgical removal of the affected thyroid gland(s). If bilateral it is important to preserve at least one parathyroid gland to maintain calcium homeostasis. Although effective, surgical treatment of hyperthyroidism is quite historical. The method of choice is removal via the extracapsular technique.
Medical treatment includes the drug Carbimazole. This interferes with thyroid hormone synthesis and is licensed in the UK. Methimazole is also used and licensed. Both drugs may produce adverse reactions in around 15% of cases and have the disadvantage of needing cooperative cats and owner compliance.
The other therapy is radioactive iodine therapy. This is useful for intrathoracic thyroid nodules. It is a very simple, effective and safe method of treating hyperthyroidism. The main disadvantages are that the cat needs to be kept in a hospital environment in isolation. There are few, although number are increasing, hospitals in the UK that have this treatment available, and all take referrals.
| Hyperthyroidism Learning Resources | |
|---|---|
 Test your knowledge using flashcard type questions |
Feline Medicine Q&A 05 |
References
Blood, D.C. and Studdert, V. P. (1999) Saunders Comprehensive Veterinary Dictionary (2nd Edition), Elsevier Science.
Church, D. (2008) Endocrine System Study Guide, Royal Veterinary College.
Ettinger, S.J. and Feldman, E. C. (2000) Textbook of Veterinary Internal Medicine Diseases of the Dog and Cat Volume 2 (Fifth Edition), W.B. Saunders Company.
Ettinger, S.J, Feldman, E.C. (2005) Textbook of Veterinary Internal Medicine (6th edition, volume 2), W.B. Saunders Company.
Fossum, T. W. et. al. (2007) Small Animal Surgery (Third Edition), Mosby Elsevier.
Nelson, R.W. and Couto, C.G. (2009) Small Animal Internal Medicine (Fourth Edition), Mosby Elsevier.
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
Error in widget FBRecommend: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt69899935c359d1_95902686 Error in widget google+: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt69899935d0b708_20505342 Error in widget TwitterTweet: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt69899935d61088_39848969
|
| WikiVet® Introduction - Help WikiVet - Report a Problem |