Difference between revisions of "Innate Immunity Cellular Responses"
Rjfrancisrvc (talk | contribs) |
Rjfrancisrvc (talk | contribs) |
||
| Line 34: | Line 34: | ||
==[[Neutrophils|Neutrophils]]== | ==[[Neutrophils|Neutrophils]]== | ||
[[Image:Neutrophil 2.jpg|thumb|right|150px|Neutrophils - J. Bredl, RVC 2008]] | [[Image:Neutrophil 2.jpg|thumb|right|150px|Neutrophils - J. Bredl, RVC 2008]] | ||
| − | |||
* Neutrophils are the principal, highly active '''phagocytes''' in the blood | * Neutrophils are the principal, highly active '''phagocytes''' in the blood | ||
** Comprise 30-70% of white blood cells depending on species | ** Comprise 30-70% of white blood cells depending on species | ||
Revision as of 10:23, 1 May 2012
Introduction
Pathogens can invade the body if a breach occurs in the barriers formed by the skin and mucus membranes, for example a wound, they must be detected and destroyed by cellular and humoral means.
The cells involved in the cellular response to a wound are:
- Tissue mast cells and macrophages that initially phagocytose and detect bacteria or fungi
- The blood granulocytes, or Polymorphonuclear (PMN: multi-lobed nuclei) Cells
- The Neutrophils are the most abundant as they are the primary cells that phagocytose bacteria, and the larger fungi
- The Eosinophils and Basophils / mast cells are only needed in rare circumstances as they are for killing parasites by the release of granules (exocytosis).
- Blood monocytes: phagocytose bacteria
The main role of the innate cellular response is to delay systemic infection until the adaptive response can back it up with a more specific attack
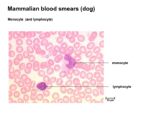
Macrophages
The innate cellular response begins with recognition and phagocytosis by macrophages that precide in the tissue where the wound occurs. The populations of distinct, tissue-specific macrophages that are present are the:
- Alveolar macrophages (lung)
- Tissue histiocytes
- Glomerular macrophages (kidney)
- Hepatic Küpffer cells (liver)
- CNS microglia (Central Nervous System: Brain and Spinal Cord)
- Sinus-lining macrophages of the lymph nodes and spleen
When phagocytosis of the bacteria or fungi by the tissue macrophages occurs they release a number of cytokines that have a number of effects. The first being the activation of the endothelium that results in the expression of adhesion molecules that allow leukocytes, in particular the neutrophils to bind to the endothelium from the bloodstream and the subsequent extravasation (movement out of the bloodstream). Once the leukocytes are out of the bloodstream, the cytokines released by the tissue macrophages act as chemoattractants that enable the chemotaxis of the leukocytes to the site of infection.
The Monocytes are immature macrophages that are circulating phagocytes. They circulate for 6-8 hours and function as phagocytes within the blood and as newly migrated cells in tissues. Their primary function, however, is to replace the various tissue macrophage populations at the latter stages of the immune response.
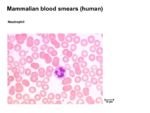
Neutrophils
- Neutrophils are the principal, highly active phagocytes in the blood
- Comprise 30-70% of white blood cells depending on species
- Kill and digest microbes in a similar way as macrophages
- Neutrophils can also cause extracellular bacterial killing by disrupting bacterial membranes
- Secrete small antibacterial peptides
- E.g. defensins and bactenecins
- Secrete small antibacterial peptides
- Neutrophils produce vasoactive peptides
- E.g. histamine and bradykinin
- Cause a great increase in extravasation of blood granulocytes and monocytes and plasma proteins at the site of infection
- Neutrophils are the archetypal cell associated with acute inflammation
- Are attracted to sites of inflammation by:
- Complement activation
- Cytokine production
- Changes to vascular endothelium
- Neutrophil activation in an inflammatory lesion results in the release of prostaglandins
- Responsible for vasoactive changes and for pain
- Are attracted to sites of inflammation by:
- The accumulation of dead and dying neutrophils at the site of infection is called pus
- Their removal from the site after the removal of infection is an important step in the resolution of the lesion
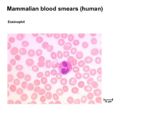
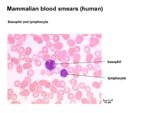
Eosinophils
- Eosinophils are less common than neutrophils, and they are not phagocytic
- Make up <5% of the leukocytes in normal blood
- Eosinophil numbers are increased:
- Slightly during the resolution phase of inflammation
- Many-fold in parasite-infected animals
- The presence of a large proportion of eosinophils in a blood smear is highly indicative of parasitaemia
- Mainly function by targeting the surface of parasites by means of specific antibody or complement
- Release a large range of toxic molecules that break down the parasite integument
- Prominent in allergic (anaphylactic) reactions
Basophils / Mast Cells
- Basophils/mast cells are principally localised at epithelial surfaces
- Very small numbers are present in blood
- Less than 0.5% circulating leukocytes
- Very small numbers are present in blood
- They have two principal functions:
- Induction of acute inflammation
- Trauma and/ or bacterial infection causes the production of cytokines by the mast cells that induce a classical acute inflammatory response
- Response to parasite infection
- Specific IgE binds cells
- Subsequent contact with antigen causes the mast cells to degranulate
- Release enzymes and vasoactive substances that can result in a high level of mucus secretion and smooth muscle contraction
- Induction of acute inflammation
- Also produce factors that influence local host cell physiology
- Various mediators increase the ratio of phagocyte to microbe
| Originally funded by the RVC Jim Bee Award 2007 |