Difference between revisions of "Acute Inflammation - Introduction"
Rjfrancisrvc (talk | contribs) |
Rjfrancisrvc (talk | contribs) |
||
| Line 22: | Line 22: | ||
#* Circulating white blood cells, in particular [[Neutrophils|neutrophils]], begin adherence to the altered endothelial surfaces. | #* Circulating white blood cells, in particular [[Neutrophils|neutrophils]], begin adherence to the altered endothelial surfaces. | ||
# '''Emigration of leukocytes''' | # '''Emigration of leukocytes''' | ||
| − | #* [[Leukocytes|Leukocytes]] migrate, by an active process, through the altered endothelium to reach the injured area. This process is called '''diapedesis'''. The cells are stimulated to do this by chemoattractants in the vicinity of the injury, for example the [[Cytokines|cytokines]] TNF-. | + | #* [[Leukocytes|Leukocytes]], again mostly neutrophils, migrate, by an active process, through the altered endothelium to reach the injured area. This process is called '''diapedesis'''. The cells are stimulated to do this by chemoattractants in the vicinity of the injury, for example the [[Cytokines|cytokines]] TNF-α, Il-1 and IL-6, and the [[Complement|complement]] components C3a and C5a. Once through the endothelium, emigrated leukocytes and components of the fluid exudate are also chemotactic, allowing them to home in to exactly where the injury occured. Once these cells are in contact they further amplify the chemoattractant mechanisms allowing more cells and fluid to be attracted to the area. |
| − | |||
| − | |||
# '''Emigration of red blood cells''' | # '''Emigration of red blood cells''' | ||
| − | #* [[Erythrocytes|Erythrocytes]] migrate through the gaps in the altered endothelium to the damaged tissue. | + | #* Once the gaps are big enough [[Erythrocytes|Erythrocytes]] can migrate through the gaps in the altered endothelium to the damaged tissue. |
# '''Induction of an increase in temperature''' | # '''Induction of an increase in temperature''' | ||
| − | #* This may occur either locally or systemically. | + | #* This rise in temperature may occur either locally or systemically. A systemic rise in temperature is known as pyrexia. Occurs in general acute inflammation, and is often a sign of infection. To raise the body temperature, pyrogens are released which act on the temperature control centres in the hypothalamus, and are released from[[Macrophages|macrophages]] in particular, but also [[Neutrophils|Neutrophils]] and [[Eosinophils|eosinophils]]. Again, the [[Cytokines|cytokines]] TNF-α, Il-1 and IL-6 are all important in producing this pyrogenic response. These are termed '''endogenous pyrogens''' as they are endogenous to the body and not from an external source. Other pyrogens include the cellular coat of gram-negative organisms, the necrosis of damaged tissue cells, antigen-antibody complexes, and tumours (particularly those which have metastasised though it may be difficult to separate this from the pyrexia caused by the central necrosis in such tumours). |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==Cells== | ==Cells== | ||
Revision as of 15:37, 9 May 2012
Introduction
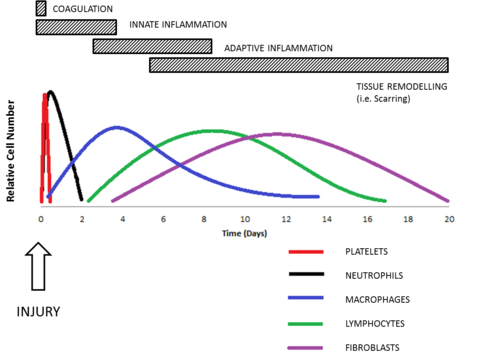
Acute inflammation is characterised by a sudden onset and may last for a few hours to a few days. Vascular, humoral and cellular alterations cause the 5 cardinal signs of inflammation as a result of exposure of tissues to various causes.
When acute inflammation becomes over-active it can be fatal. A classic example is septic shock caused by bacterial LPS. In most cases though acute inflammation acts to protect and repair the damage to the tissue by resolving by regeneration in association with the host defence mechanisms. To assist in resolving and controlling inflammation therapeutic measures have been developed, with some being very recognisable therapies, for example the Non-Steriodal Anti-Inflammatory Drugs (NSAIDs e.g. Aspirin and Ibuprofen N.B. NOT paracetomal).
A repair mechanism that can occur is fibrosis, otherwise known as scarring. There are also conditions, for example arthritis, where the acute inflammation can become chronic. First the inflammation goes through a subacute phase, though whether the inflammation becomes chronic is dependent upon the persistence of the agent and the amount of damage caused.
Sequence of Events
The following sequence of events is provoked by the presence of the irritant.
- Momentary vasoconstriction
- Following contact with the irritant, there is momentary vasoconstriction of the blood vessels in the affected area and is reversed within minutes.
- Dilation of the blood vessels
- Initially, dilation of the capillaries is caused by the release of chemical mediators. The arterioles then dilate under the influence of a local axon reflex, which gives rise to an initial acceleration of the blood flow to the area. This then later gives way to a slowing of blood flow, caused by alterations in vascular endothelial permeability and the filling of previously closed capillaries.
- Exudation of fluid
- Following the slowing of blood flow and altered capillary permeability, a protein-rich fluid is exudated.
- Margination of leukocytes
- Circulating white blood cells, in particular neutrophils, begin adherence to the altered endothelial surfaces.
- Emigration of leukocytes
- Leukocytes, again mostly neutrophils, migrate, by an active process, through the altered endothelium to reach the injured area. This process is called diapedesis. The cells are stimulated to do this by chemoattractants in the vicinity of the injury, for example the cytokines TNF-α, Il-1 and IL-6, and the complement components C3a and C5a. Once through the endothelium, emigrated leukocytes and components of the fluid exudate are also chemotactic, allowing them to home in to exactly where the injury occured. Once these cells are in contact they further amplify the chemoattractant mechanisms allowing more cells and fluid to be attracted to the area.
- Emigration of red blood cells
- Once the gaps are big enough Erythrocytes can migrate through the gaps in the altered endothelium to the damaged tissue.
- Induction of an increase in temperature
- This rise in temperature may occur either locally or systemically. A systemic rise in temperature is known as pyrexia. Occurs in general acute inflammation, and is often a sign of infection. To raise the body temperature, pyrogens are released which act on the temperature control centres in the hypothalamus, and are released frommacrophages in particular, but also Neutrophils and eosinophils. Again, the cytokines TNF-α, Il-1 and IL-6 are all important in producing this pyrogenic response. These are termed endogenous pyrogens as they are endogenous to the body and not from an external source. Other pyrogens include the cellular coat of gram-negative organisms, the necrosis of damaged tissue cells, antigen-antibody complexes, and tumours (particularly those which have metastasised though it may be difficult to separate this from the pyrexia caused by the central necrosis in such tumours).
Cells
- The classical cells of acute inflammation are neutrophils, eosinophils, macrophages, mast cells and basophils at an early stage of the inflammatory response, with the lymphocytes and fibroblasts forming the later stages.
- Macrophages are a common feature of acute and chronic inflammation.