Difference between revisions of "Recurrent Airway Obstruction"
Jump to navigation
Jump to search
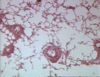
(Created page with "Chronic obstructive pulmonary disease (COPD) [[Image:COPD.jpg|right|thumb|100px|<small><center>COPD (Image sourced from Bristol Biomed Image Archive with permission)</center></sm...") |
m (Text replace - "Category:To Do - Blood" to "Category:To Do - BloodCategory:To Do - Clinical") |
||
| Line 25: | Line 25: | ||
[[Category:Allergic Respiratory Diseases]] | [[Category:Allergic Respiratory Diseases]] | ||
| − | [[Category:To Do - Blood]] | + | [[Category:To Do - Blood]][[Category:To Do - Clinical]] |
[[Category:Horse]] | [[Category:Horse]] | ||
Revision as of 10:56, 20 August 2010
Chronic obstructive pulmonary disease (COPD)
- Synonyms: Recurrent Airway Obstruction (RAO) (correct current terminology), "heaves", "broken wind"
- COPD is one of the most common conditions encountered in adult horses and is a major cause of loss of performance
- It is an asthma-like syndrome of the bronchioloalveolar region
- The aetiopathogenesis of COPD is not fully understood, but is thought primarily to be caused by an immune-mediated hypersensitivity response to inhaled allergens commonly found in mouldy hay or bedding and in stable dust (eg: spores from Faenia rectivirgula, Aspergillus fumigatus, and Thermoactinomyces vulgaris)
- The immune reaction is considered primarily to be a type III hypersensitivity (antigen-antibody complex mediated)
- Type I and type IV hypersensitivity reactions may also play a role
- Repeated episodes of inflammation in the lower airways, especially the bronchioles, results in chronic changes that cause obstruction of the lower airways, sometimes followed by alveolar emphysema
- The histological features are what you would predict given this pathogenesis:
- Luminal accumulation of exudate made up of thick mucus (goblet cell metaplasia), neutrophils and cellular debris
- This can predispose to, and is often accompanied by, secondary bacterial infection eg: Streptococcus equi subsp. zooepidemicus
- Thickened mucosa - epithelial hyperplasia, chronic inflammatory cell infiltrate with variable numbers of eosinophils in the airway wall
- Peribronchiolar fibrosis
- Bronchospasm
- When susceptible horses are exposed to inhaled allergens they develop airway inflammation and respiratory dysfunction
- Typically, susceptible horses are clinically normal when at pasture, but develop signs of disease shortly (hours to days) after being housed
- Clinical signs are what you would predict from a chronic inflammatory process in the airways:
- Coughing (following activation of coughing reflexes due to inflammation in the airways, mechanical pressure on the airway walls associated with the accumulation of intraluminal exudate)
- Nasal discharge (usually bilateral - mucopurulent tracheal exudate on bronchoscopy)
- Increased respiratory rate (compensation for reduced tidal volume following the reduction in airway lumen diameter)
- Pronounced effort during inspiration with an obvious abdominal component (may result in a "heave-line" in the flank due to hypertrophy of the abdominal muscles - reduced airway diameter results in increased resistance to air flow, so more inspiratory effort required for same airflow rates)
- Wheezing and crackling lung sounds on auscultation at the end of inspiration and expiration - caused by bubbles in mucus collapsing