Bones - Anatomy & Physiology
Aimee, please look at page Bones - Anatomy & Physiology and use any info from there that isn't on this page. Then please add that page (bones) to category:Delete. Thanks! Bara
Overview
Bone comprises the structure of the skeletal system and provides lever arms for locomotion. Bone also plays important roles in maintaining mineral homeostasis, as well as providing the environment for hematopoesis in marrow.
Development of Bone and Cartilage
Aimee, please combine this section with Bone & Joint Development - Anatomy & Physiology page and provide link from this page to it. Any questions, please let me know. Thanks, Bara Osteogenesis is the collective name for bone formation.
Intramembranous Ossification
Forms the flat bones of skull and mandible. There is no cartilaginous precursor, the mesenchyme forms bone directly. The mesenchyme condenses, differentiates to pre-osteoblasts, then to osteoblasts. The osteoblasts synthesize osteoid (collagen and proteoglycans) causing mineralization and bone spicule formation. Spicules produce spongy bone. The bone growth can be described as appositional growth, where bone is laid down on the exterior (vs interior) surface of the developing bone. During bone development there is an increasing association with blood vessels and bone marrow is formed by the mesenchyme, between the bone and the blood vessels.
Endochondral Ossification
This is responsible for embryonic bone formation, as well as the growth in length. This occurs via a cartilaginous precursor. The mesenchyme condenses to form the bone outline. Core cells differentiate to chondrocytes and begin secreting the cartilage matrix. Peripheral condensation forms the perichondrium. Interstitial (length) and appositional (width) growth can be noted. The central cells in the developing diaphysis mature and grow and the matrix surrounding the most mature chondrocytes calcifies. The perichondrium then differentiates to osteoblasts. Capillary invasion occurs to the central core of the bone, forming trabecular bone.
Bone Growth and Remodeling
Short bones- Endochondral ossification continues in the diaphysis, until only the cartilage rim remains.
Long bones- A secondary center of ossification develops in the epiphyses.
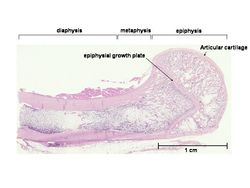
Epiphyseal Growth Plate- The growth plate is a transverse disc of cartilate between the two ossification centers, and allows longitudinal growth to continue to maturity. It then closes. The cartilage of the epiphyseal growth plate is divided into: (from right to left on the magnified image) 1. Resting (reserve) zone 2. Proliferative zone 3. Hypertrophic zone
Primary bone has not yet been remodelled. It contains less mineral and more randomly arranged collagen fibers, known as trabecular organization. Remodelling of bone occurs by haversian canals. The osteoclasts dig out the canal, followed by blood vessel invasion. Concentric lamellae are laid down and phased resorption happens concurrently.
Types of Bone
1. Long Bone
Found in the limbs and act as levers for locomotion. An elongated diaphysis (shaft) and two epiphyses (ends), each of which encases a center for ossification.
2. Short Bone
Found in places of articulation, such as the carpus and tarsus. All dimensions are relatively equal, generally signifying one center of ossification.
3. Flat Bone
Found in the skull, pelvic girdle, and scapula. It expands in two directions, with a broad surface for attachment of large muscle masses and protection of underlying structures.
4. Sesamoid Bones
Eg. Patella and navicular bone. Found within tendons, where they change direction over prominences that would otherwise cause damage. They form synovial joints with major bones with which they are in contact. They also serve to displace tendon from the axis of the joint, increasing the leverage exerted by the muscle.
5. Splanchnic Bones
Develop in soft organs remote from skeletal connection, eg. os penis.
6. Pneumatic Bones
Excavated to contain air spaces, such as the skull in the instance of paranasal sinuses, and the post-cranial skeleton of birds.
Composition of Bone
Bone is a hard, highly specialised connective tissue . It consists of interconnected cells embedded in a calcified, collagenous matrix. It is a living, dynamic, responsive tissue, growing and remodelling throughout life.
Bone is comprised of:
Matrix
Osteoid- An organic, uncalcified, homogeneous substance that stains light pink with H&E . Osteoid consists of type I collagen (90%), which resists tension and bone-specific proteins(10%), including; Osteonectin, Osteopontin and Osteocalcin.
Mineral- An inorganic component, provides rigidity. Consists of a crystalline lattice of calcium phosphate and calcium carbonate. It also contains Mg, Mn, Zn, Cu, Na, F. It accounts for 65% of bone.
Cells
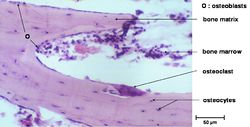
Osteoblasts
A single layer of mesenchymal cells which synthesize bone extracellular matrix (osteoid). When active, thet appear plump and cuboidal, with a basophilic cytoplasm. The cell membranes are rich in alkaline phosphatase (ALP). The cells are possibly involved in pumping calcium across membranes. They are promoted by growth factors and have receptors for PTH. They contract in response, which provides space for osteoclasts to attach. When they are inactive, there is less cytoplasm, so they become flattened.
Osteocytes
osteoblasts are embedded in their own matrix; reside within lacunae and are interconnected via channels forming canaliculi. Canaliculi create connections to form a huge neural-like junctional organization. They contact osteoblasts and each other with cytoplasmic processes and reach through canaliculi in the mineralised bone matrix. Osteocytes regulate the composition of bone fluid.
Osteoclasts
Osteoclasts are giant (multinucleate monocytes) cells. Histologically, they are large, often multinucleated cells. They have an acidophilic cytoplasm. They sit in the bone surface depression known as, howship's lacuna. Osteoclasts respond to vitamin D by increasing their numbers and activity (parathyroid independent). Osteoclasts act to resorb the bone ECM. They firstly dissolve mineral followed by collagen, using the brush border. They do not have receptors for PTH, but do have receptors for calcitonin.
Osteoblasts, osteocytes, chondroblasts and chondrocytes are derived from the stromal fibroblastic system (osteoprogenitor cells). Osteoclasts are derived from the haematopoietic system.
Organization of Bone
The normal progression of bone is from woven bone to lamellar bone, even in pathology, except for canine craniomandibular osteopathy and hypervitaminosis D, where lamellar bone is replaced by woven bone.
Woven bone
Woven bone consists of coarse collagen fibres. It is later removed by osteoclasts and replaced by lamellar bone. In adults, it is a sign of a pathological condition (e.g. fracture, inflammation, neoplasia).
Lamellar bone
Lamellar bone consists of orderly layers, which are much stronger than woven bone. There are fine collagen fibres in concentric or parallel laminae. There are two main types of lamellar bone:
1. Compact bone (cortical)
A sheath covers the external surface of long bone. It is thicker in the shaft and thins over the epiphyses. It is comprised of thin lamallae in a series of concentric tubes arranged around small central canals (collectively known as an osteone). It forms 80% of the total bone mass and consists of cells and interstitial substance - 30% ossein (type of collagen) and 70% minerals, especially calcium phosphate.
2. Cancellous bone (spongy or trabecular)
Stacks of parallel or concentrically stacked sheets arranged as rods, plates, and arches. In vertebrae, it forms flat bones and forms the hematopoeitic center of epiphyses of long bones. It contains no Haversian systems.
Laminar bone
Formed on the periosteal surface of diaphysis. It accomodates rapid growth of large dogs and farm animals. Plates of woven bone from within the periosteum. As it forms, it fuses with the bone surface.
Periosteum and blood supply
Periosteum
The periosteum is the specialised sheath of connective tissue covering bone, except at the articular surfaces. It is loosely attached, except at tendon insertions and boney prominences. Histologically, there is an outer layer which is fibrous for support, and an inner layer that is osteogenic. It consists of a rich supply of nerves and lymph vessels, including nutrient, metaphyseal and periosteal arteries. The normal flow of blood from the medulla to the periosteum is due to higher pressures in the medulla. Young animals have a greater blood supply.
The endosteum lines the marrow cavity. The medullary cavity and cancellous interstitium is for bone marrow storage and production. Red marrow is a richly vascularized, gelatinous tissue with hematopoeitic properties found abundantly in young animals and yellow marrow has been converted from red marrow by fat infiltration, causing hematopoeitic properties to dwindle.
Biomechanics of Bone
Bone growth and maintenance of normal structure are directly related to mechanical forces. Mechanical forces generate bioelectrical potentials (piezoelectricity), these potentials strengthen bone. Inactivity reduces the potentials, causing bone loss.
Wolff's Law
Bone architecture adapts in response to the loads applied upon it according to mathematical laws;
Load: the external force placed on a structure, F.
Strain: the proportional change in the structure's dimensions.
Stress: the internal forces resisting the change in dimension caused by the load.
Cells use strain as a stimulus to adjust mass and architecture according to load. Resorption and osteogenesis happen concurrently to maintain bone integrity. This is mediated by two hormones:
1. Parathyroid hormone (PTH)
Produced by chief cells in the parathyroid glands in response to decreased serum calcium. In response, osteoclasts increase in number and resorb mineralised matrix to increase Ca in blood.
2. Calcitonin
Produced by C-cells in the thyroid glands in response to increased serum calcium. Inhibits osteoclasts.
In neonates, bone growth predominates and modelling is important. In adults, the formation of bone is balanced by resorption - remodelling. It continues throughout life under the influence of hormones and mechanical pressure. Bone resorption may exceed formation in pathological states (hormonal, trauma, nutritional) or in old age and disuse.
Structure and Function of Cartilage
The function of cartilage is to resist compression, provide resilience and support at sites where flexibility is desired.
Structure
Chondrocytes
Reside within lacunae within ECM and are responsible for synthesizing the matrix. The matrix consists of type II collagen, (except fibrocartilage) and proteoglycans with associated glycosaminoglycans. They are continually turned over and are the most vulnerable component of cartilage. Decresed proteoglycan, causes loss of lubrication which results in collagen disruption. This includes, frays, clefts, fibrillation, ulcers, exposure of bone, eburnation, +/- osteophytes and joint mice.
Cartilage is avascular, nutrients and waste move via diffusion. The perichondrium surrounding the cartilage is composed of two layers:
1. Fibrous- outer, dense irregular connective tissue.
2. Chondrogenic- inner, flattened cells that differentiate to chondrocytes.
Types of Cartilage
Hyaline Cartilage
The most abundant in the body. It is normally blue-white, smooth with a moist surface and turns yellow and becomes thinner in old age. It is found in nose, trachea, bronchi, ventral ends of ribs and sternal attachment. It is surrounded by perichondrium. It is at sites of articulation to provide a resilient, frictionless surface that resists compression. It is also found at epiphyseal growth plates.
Elastic Cartilage
Elastic cartilage has a yellow appearance and is found in auricular cartilage, larynx, eustacian tube, and epiglottis. It is surrounded by perichondrium and has resiliance with added flexibility.
Fibrocartilage
Fibrocartilage has more collagen (Type I) and less proteglycans than hyaline. It resists high tensional strain and is often in transition with hyaline. It is found in intervertebral discs, tendon/ligament attachment to bone, joint menisci, and articular surface of some joints (such as the temperomandibular). It has NO perichondrium.
Links
Click here for information on bone and cartilage pathology.