Testes and Epididymis - Anatomy & Physiology
Testes
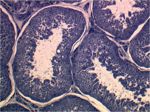
Testicular Architecture
Scrotum
- Skin - Contains many sweat glands, thermosensitive receptors and sympathetic nerves.
- Tunica Dartos - Smooth muscle layer found below the skin of the scrotum. Smooth muscle tone controlled by Androgens released in response to temperature changes detected by sensory nerves within the scrotal skin. The tunica dartos is responsible for holding the testes close to the body during cold temperatures, as it can maintain sustained contraction, and letting the testes lower in hot weather, increasing the surface area for heat loss from the skin.
- Scrotal fascia
- Parietal Vaginal Tunic - The first peritoneum layer taken into the scrotum by the peritoneum fusion with the gubernaculum during testicular descent.
Function:
- Temperature sensor
- Protection
- Cooling of testes - evaporative heat loss due to lots of sweat produced by glands in the skin.
Vaginal Cavity
A potential space
Testicular Capsule
- Visceral Vaginal Tunic - The second peritoneum layer within the scrotum. This layer is closely applied to the Tunica Albuginea.
- Tunica Albuginea - A connective tissue layer containing some smooth muscle fibres. The tunica albuginea sends projections from the capsules into the testicular parenchyma that join up with the mediastinum of the testis forming lobules. Contraction and relaxation of the smooth muscle fibres within the tunica albuginea in response to acetylcholine and norepinephrine results in a pumping action facilitating the flow of spermatozoa through the tubules of the testes.
Testicular Parenchyma
- Interstitial Leydig cells - Produce the androgen testosterone important for supporting spermatogenesis.
- Capillaries, Lymphatic vessels, connective tissue.
Tubular Compartment
- Seminiferous tubules
- Make up highly convoluted tubule network within the testicular parenchyma. These seminiferous tubules connect to rete tubules. The seminiferous epithelium making up the tubules can be divided into two compartments seperated by junctional complexes between the somatic Sertoli cells within the epithelium:
- Basal compartment - containing spermatogonia and proliferating germ cells.
- Adluminal compartment - containing spermatocytes, spermatids and spermatozoa
The Sertoli cells are much larger than the developing germ cells and span the basement membrane to the lumen of the seminiferous tubules. Their function is provide support to developing germ cells and form the blood-testis barrier. Each Sertoli cell can only support a certain number of developing germ cells. Therefore, the number of Sertoli cells within a testis determines the sperm production capabilities of that individual.
Function of the seminiferous tubules:
- Peritubular cells - contractile cells surrounding the seminiferous tubules
- Production of spermatozoa by Sertoli cells
- Production of hormones by interstitial Leydig cells
- The Blood-Testes Barrier formed by tight junctions between neighbouring Sertoli cells. This barrier prevents White blood cells from entering the adluminal compartment of the seminipherous tubules and autoreacting to the haploid spermatids within it.
Comparative Testicular Architecture
There are species differences between Sertoli cell number and parenchyma composition. In the boar the parenchyma is made up from many Leydig cells and little lymph space, humans and rams contain slighly more lymph space and the rat parenchyma is mainly lymph space with few Leydig cells.
Histology
Vasculature
- The Testicular Artery a direct branch off the aorta.
- This has important implications when performing castration procedures as the pressure within the artery will be very high and so it is imperitive to tie the artery off properly.
- The testicular artery is highly convoluted and contains many elastic fibres within its wall. It acts as a pulse pressure eliminator between the inguinal ring and surface of the teste, minimising the differance between systolic and diastolic pressures within the artery (usually 40mmHg).
- The Pampiniform Plexus
- The network of testicular veins that surround the testicular artery providing the testes with a countercurrent heat exchanger.
- The testes require a temperature of 33°C in order for maintaining spermatogenesis, 3-6°C lower than core body temperature. This is achieved by the countercurrent exchange system between the pampiniform plexus and the testicular artery. Heat is transfered from the warmer blood in the testicular artery to the cooler blood returning from the testes in the testicular veins. The testicular veins run close to the surface of the scrotum so the blood within them is cooled by heat radiation from the skin of the scrotum.
Testicular Descent
The developing testes start off in the abdomen. They develop from somatic mesenchymal cells in the genital ridge found caudal to the developing kidneys, around the tenth thoracic vertebra. The testes migrate caudally and retroperitoneally towards the inguinal canal and scrotum. This translocation of the testis is the result of growth and contraction of the gubernaculum aswell as the relative growth of associated viscera within the abdomen. The gubernaculum is a ligamentous structure extending from the site of the future scrotum, through the inguinal ring to the caudal testis. In the inguinal region the distal portion of the gubernaculum fuses with the covering peritoneum before its descent, forming the visceral and parietal vaginal tunics. These two layers of peritoneum cover the testes within the scrotum and are seperated by the vaginal cavity. Once the testes have descended into the scrotum the inguinal canal contracts behind them to keep them in place. The gubernaculum regresses and leaves behind remnants which can be found in the adult; the proper ligament of the testis and the ligament of the tail of the epididymis.
Epididymis
The Epididymis provides the environment for final maturation of spermatozoa. It is here that they aquire motility and fertility. The Epididymal duct is very long, between 30-60 meters. It is devided functionally into 3 regions; the Caput (head), Corpus (body) and Cauda (tail). The caput of the epididymis is connected to the efferent ducts of the testes. The Cauda connects to the Ductus Deferens of the spermatic cord.
Structure & Function
Caput (head)
- Fluid secreted in the rete tubules of the testes is reabsorbed here and epididymal fluid is secreted. This fluid secretion is important in order to facilitate movement of the sperm through the epididymis.
Corpus (body)
- Nuclear chromatin condenses via the addition of di-sulphide bridges. This condensation stabilises the nuclear material and can be observed histologically as darker staining material.
- Stabilising surface proteins are added to the sperm membranes.
- Sperm aquire fertility by the addition of membrane receptors to female tract ligands. This enables them to bind to the Zona Pellucida and oocyte membranes.
- Sperm cells are dehydrated.
- Sperm aquire forward motility.
Cauda (tail)
- Sperm metabolic activity is depressed in order to prolong life.
- Sperm are stored here until ejaculation.
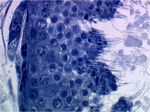
Histology
The Epididymal duct is surrounded by smooth muscle fibers. These fibers contract rhythmically facilitating sperm movement through the duct.
Caput
- Columna epithelium with basal nuclei.
- Small steriocillia present, these have an absorbtive function
Corpus
- Low columna epithelium with very prominant stereocillia.
- Small groups of sperm can be observed within the lumen of the duct.
Cauda
- Cuboidal/ Low columna epithelium. However, unlike the caput and corpus regions of the epididymis the cauda epithelium has no stereocillia.
- Large numbers of sperm observable here as this is the site of sperm storage within the testes.
| Testes and Epididymis - Anatomy & Physiology Learning Resources | |
|---|---|
 Selection of relevant videos |
Dissection of the equine testicle |
 Selection of relevant PowerPoint tutorials |
Histology of the Male reproductive tract |
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |