Equine Eye - Horse Anatomy
| This article is still under construction. |
Introduction
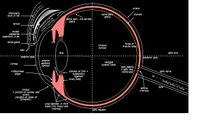
The eye is a paired organ, the organ of vision. The eye is made up of various components, which enable it to receive light stimuli from the environment, and deliver this stimuli to the brain in the form of an electrical signal. Vision involves all components of the eye. The eye is contained within the bony orbit of the head. The bony orbit is a cavity, comprising parts of the lacrimal bone (includes fossa for nasolacrimal duct) and the maxilla (includes caudal foramen of infraorbital canal). It is continuous with the temporal bone and the pterygopalatine fossa caudally. The bony orbit is located laterally in horses, as they are in most prey species. This allows horses a range of vision of more than 350°. However this wide range of monocular vision has two 'blind spots', these are straight in front of the face and directly behind the head, extending over the back and tail. This is important to consider when approaching a horse.
Movement of the eyeball is achieved through the contraction and relaxation of six extraocular muscles:
- Dorsal rectus muscle
- Ventral rectus muscle
- Medial rectus muscle
- Lateral rectus muscle
- Dorsal oblique muscle
- Ventral oblique muscle
The Transparent Media (conjunctiva, cornea, lens, and vitreous and aqueous humour)
Conjunctiva
The conjunctiva is continuous with the skin of the eyelids. The palpebral conjunctiva is the part of the conjunctiva that covers the inner surface of the eyelid, the bulbar conjunctiva covers the surface of the eyeball. It is lined by stratified squamous epithelium, and contains goblet cells, which secrete the deepest, mucus, layer of tear film, which adheres to the surface of the globe. It is highly vascular.
Cornea
The cornea and sclera together make up the tough outer, supportive structure of the eye. Although the cornea has the same composition as the sclera, it is transparent. The main function of the cornea is to refract light. The hallmark of corneal disease is opacity. The transparency of the cornea is partially due to the organization of stromal collagen, but the endothelium plays a critical role as it keeps the cornea in a constant state of relative dehydration. It is avascular, so nutrients and oxygen are obtained from the aqueous humour, and oxygen is also obtained from air. The cornea joins with the sclera at the point of the limbus; the sclera is vascular, but otherwise similar to the cornea.
The layers of the cornea are:
1. (conjunctiva)
2. Bowman’s membrane (basal lamina)
3. Thick transparent fibrous layer
4. Descement’s membrane
5. Endothelium (inner lining of the cornea)
The corneal epithelium consists of an outer layer of squamous cells, a middle layer of polyhedral cells and an inner single layer of columnar cells that produce the basement membrane. The epithelium is attached to the basement membrane by hemidesmosomes and fine fibrils link the basal epithelium, basement membrane and subepithelial stroma.
The stroma (substantia propria)comprises the bulk of the cornea, consisting primarily of keratinocytes, regularly arranged collagen fibrils and ground substance. Fibrils are arranged in sheet-like bundles (lamellae) that extend across the entire width of the cornea, from limbus to limbus; this arrangement helps to maintain transparency. The ground substance of proteoglycans and glycosaminoglycans (GAGs) & glycoproteins occupies the space between lamellae. The keratinocytes have a slow turnover rate in the normal adult cornea, but if there is a corneal insult they can become active fibroblasts and produce precursors of collagen and ground substance. Other cells such as leukocytes, lymphocytes and macrophages are rare in the normal cornea.
The corneal endothelium produces Descemet’s membrane throughout life, but its own powers of replication diminish in early life. When endothelial cells die, they are replaced by neighbouring cells spreading to fill the gap. Consequently, the endothelium thins and descemet’s membrane thickens with age. The endothelium is a single layer of cells of high metabolic activity and are crucial in maintaining dehydration of the cornea and thus corneal clarity. The endothelial cells actively pump fluid that can accumulate, from tear film etc, out of the cornea.
Aqueous Humour
Aqueous humour is produced by ciliary processes of the ciliary body. It is a transparent ultra-filtrate of plasma. Its continual flow is vital for the delivery of nutrients and removal of waste products to the avascular structures it bathes; lens, inner portion of the cornea (including corneal endothelium) and trabecular meshwork. Once produced aqueous traverses the posterior chamber, passes through the pupil and enters the anterior chamber where it can then drain at the iridiocorneal angle. The aqueous is optically clear under normal conditions, a property important for vision. An opacity in the aqueous humour is usually the result of an inflammatory process. The blood-aqueous barrier to free diffusion of molecules is formed by the tight junction between non-pigmented epithelial cells of the ciliary body. Breakdown of this barrier occurs in many conditions, including inflammation, trauma and vascular disease. Interventions such as paracentesis and surgery also causes breakdown, as does topical administration of drugs such as pilocarpine. Typically, the aqueous humour becomes turbid (aqueous flare) because of leakage of plasma proteins into the anterior and posterior chambers due to the damaged barrier and loss of vessel integrity. Fibrinogen and other proteins render the aqueous ‘plasmoid’, as its protein content approaches that of plasma, and when inflammation is severe fibrin clots may form. The cellular component varies according to the underlying aetiology. A preponderance of white blood cells is termed hypopyon and a preponderance of red blood cells is called hyphaema. It also maintains intraocular pressure. An increase in intraocular pressure can cause glaucoma.
Lens
The lens is about 65% water; protein is the other main component. The basement membrane of the lens epithelial cells creates the lens capsule, which envelops the body of the lens. The capsule is an elastic membrane, which is semi-permeable and allows passage of metabolites. The anterior lens capsule is much thicker than the posterior lens capsule.
Throughout life, lens epithelial cells at the equator of the lens undergo mitosis and are pushed towards the ‘lens bow’ where they elongate producing layers of lens fibers that extend into the anterior and posterior cortex. The fibers are continually pressed inward by newly formed fibers and then lose their nuclei. As each fiber elongates, it curves around the deeper and older fibers. The tips of the lens fibers from different regions of the equator meet in a radiating pattern of lines known as sutures. These lines usually form a ‘y’ on the anterior surface of the lens and an ‘inverted y’ on the posterior surface. The suture line can sometimes be helpful in determining the location of an opacity within the lens.
The mature lens is transparent and biconvex. The centers of the lens surface are referred to as the anterior and posterior poles. The circumference of the lens is known as the equator. The center of the lens itself is referred to as the nucleus, which is surrounded by the lens cortex. Attached to the lens equator are zonular ligaments; the zonules attach the lens to the ciliary body and mediate accommodation. Contraction of the ciliary body muscles relieves tension on the zonules, which in turn, allows the elastic capsule to retract; this causes the lens to become more convex. This change in the shape of the lens changes the focal length of the lens.
The lens metabolizes mostly through anaerobic glycolysis; metabolism is limited by the avascular state of the lens and low oxygen supply. The lens is completely dependent on the aqueous humor for nutrients. Pathological changes within the lens result in deposition of lens protein, disruption of lens fibres and hence loss of lens transparency known as a cataract.
Vitreous Humour
The vitreous humour is a transparent hydrogel that occupies almost 3/4 of the volume of the eye in the posterior segment of the globe; it is composed of 99% water with collagen fibrils as a skeleton for hylaronic acid. The vitreous body is attached to peripheral structures only at the edge of the optic nerve, near the ora serrata and at the posterior lens capsule. It acts as a clear medium for transmission of light between the lens and retina and provides mechanical support for the internal structures of the eye.
The Wall (retina, uvea and sclera)
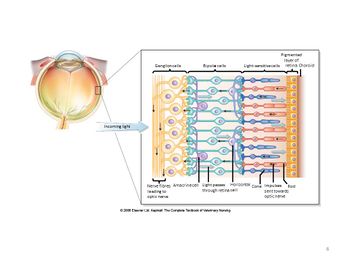
The retina is the inner layer of the eyeball, it develops from the optic vesicle, which is an outgrowth of the diencephalon. It remains connected to the diencephalon via the optic nerve. It can be divided into the non-visual retina (lines the back of the ciliary body) and the optic part of the retina.
The non-visual part of the retina is lined by inner and outer single-layers of epithelium; the outer layer is pigmented, the inner layer is neural. This neural inner layer contains photoreceptors, interneurons, ganglion cells and associated stromal cells, called MÜLLER cells. Rods and cones are photosensitive receptor cells, and are found in the optic part of the retina. Rods are mainly utilised at night, as they are highly sensitive receptors to black and white, while cones are mainly utilised during the day as they are used for colour vision. The fovea is an area of the retina that contains mostly cones, and in high numbers. Here, oxygen is obtained from the choroid (a pigmented layer that makes up part of the uveal tract - mentioned further down) by diffusion. In this region, there is one nerve fibre per cone.
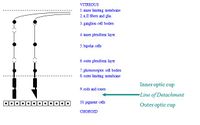
Layers of the retina, from vitreous humour to choroid:
1. Inner limiting membrane
2. Optic nerve fibres and axons of ganglion cells
3. Ganglion cell bodies
4. Inner plexiform layer - synapse of bipolar cells with ganglion cells
5. Inner nuclear layer – nuclei of bipolar cells
6. Outer plexiform layer - synapses of photoreceptors with bipolar cells
7. Outer nuclear layer – photoreceptor cell nuclei
8. Outer limiting membrane
9. Photoreceptor layer – rods and cones
Line of Detachment
10. Pigment cells – retinal pigmented epithelium
Uveal Tract
The uveal tract is a three-part physiological and pathological unit, positioned between the sclera and the retina:
1. Choroid: pigmented, highly vascular layer, containing:
a. tapetum lucidum (inner layer, nearest retina): reflective and coloured, so increases sensitivity to poor light
b. vascular layer: nutritive
c. black/connective layer (outer layer, nearest sclera)
2. Ciliary body: produces aqueous humour and vitreous humour, and is involved in lens accommodation, as its muscle fibres stretch the lens into a flatter shape, allowing distant vision
3. Iris: vascular, coloured, and contractile for pupil size
Sclera
The sclera is continuous with the cornea at the point of the limbus. It is similar to the cornea, except that it is vascular, and has dense, irregular, fibrous connective tissue.
Around the Eye (Adnexa)
Extraocular Muscles
| Muscle | Innervation | Function |
|---|---|---|
| Dorsal Rectus | Oculomotor nerve
(CN III) |
Elevates the eyeball |
| Ventral Rectus | Oculomotor nerve
(CN III) |
Depresses the eyeball |
| Medial Rectus | Oculomotor nerve
(CN III) |
Adduction of the eyeball |
| Ventral Oblique | Oculomotor nerve
(CN III) |
Outward rotation of the eyeball |
| Levator Palpebrae Superioris | Oculomotor nerve
(CN III) |
Elevates the upper eyelid |
| Lateral Rectus | Abducens nerve
(CN VI) |
Abduction of the eyeball |
| Retractor Bulbi | Abducens nerve
(CN VI) |
Retracts the eyeball |
| Dorsal Oblique | Trochlear nerve
(CN IV) |
Inward roation of the eyeball |
All of the extraocular muscles originate at the equator of the eyeball.
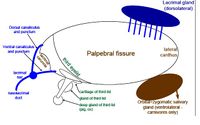
Adnexa
The adnexa refers to the accessory structures of the eye, including the eyelids and the lacrimal apparatus.
Lacrimal Apparatus
Function of the cornea depends on the integrity of the lacrimal system, a major component is the pre-corneal tear film. This is the outer-most layer of the corneal epithelium, it should stay attached to the corneal and conjunctival surface. Pre-corneal tear film functions to:
- Lubricate the cornea and conjunctiva, blinking spreads it over the surface.
- Transfer oxygen and glucose to the avascular cornea
- Provides antibodies/inflammatory cells to the cornea in the event of an irritation or foreign body.
- Flushes away foreign body material.
- Maintains an optically smooth corneal surface so that light can pass freely into the cornea.
The pre-corneal tear film is made up of three major constituents:
- Lipid outer layer: produced by the tarsal aka meibomian glands (modified sebaceous glands) in the tarsal plate of the eyelids. This prevents evaporation of the underlying layers and overflow of tear film onto the eyelids; therefore it stops dehydration of the cornea.
- Aqueous layer: in the middle, performs the primary functions of the tear film. The lacrimal gland, superficial gland of the nicitating membrane and, Hardenian gland and accessory lacrimal glands in the conjunctiva contribute to its formation. Evaluate this layer with the Shirmir Tear Test.
- Mucin: is the inner layer which sticks the aqueous phase to the corneal epithelium. It is produced by conjunctival goblet cells, mainly in the conjunctival fornixes. Evaluate with fluorescein breakup time.
The nasolacrimal drainage system functions to eliminate the used tear film and any excessive tears. Malfunction of the nasolacrimal apparatus results in tear overflow (epiphora), which may cause a cosmetic/dermatological problem of the medial periocular region. Precorneal tear film accumulates along the palpebral margin of each eyelid. Lacrimal puncta at the medial canthus of each eyelid are essentially holes which lead to canaliculi. Where the caniculi meet to drain into the nasolacrimal duct there is a slight dilatation known as the lacrimal sac. Blinking moves the fluid towards the medial canthus, most of the aqueous phase evaporates, the rest is drained by the nasolacrimal system. When orbicularis occuli muscle contracts, the eyelids close. The lacimal sac is within the muscle structure, so when the muscles contract during blinking they act like a pump to empty the lacrimal sac. When the blink is released, the muscle relaxes and the lacrimal sac opens; it sucks fluid down the canaliculi by capillary action. The fluid is then drained down the nasolacrimal duct to exit at the nasal punctum/nasal ostium in the nasal vesibule and out through the external nares.
Vision
Accommodation
Accommodation is primarily achieved by the lens, which is stretched by rectus muscle fibres of the ciliary body, causing the optical power of the eye to increase. This allows the eye to maintain a clear focus on an object, especially as the animal moves nearer towards the object.
Visual Pigments
Rods and cones are the photosensitive receptor cells of the retina, that is the light-sensitive parts of the retina.
Rod cells are mainly used at night (scotopic vision), as they function at lower light intensity. Rods are so-named due to their cylindrical shape. They are positioned in higher numbers at the edges of the retina, so are also used in peripheral vision. Rod cells are a lot more sensitive to light than cone cells, meaning that they require less light to function than cones, this being the reason that they are the predominant cells providing visual information at night. However, many rod cells converge into one interneuron, meaning that signals are amplified, but visual acuity is not as great, so the visual information that is collected may be less distinct.
Rod cells contain a pigment called rhodopsin, which itself consists of a protein called opsin. Bound to opsin is a molecule called retinene - a derivative of vitamin A. Retinene exists in the form of cis-retinene, an aldehyde, when in the dark. When stimulated by light, the cis-retinene undergoes structural change to form trans-retinene:
Vitamin A (alcohol) → cis-retinene (aldehyde) → trans-retinene
This leads to hyperpolarisation of the cell.
When rods and cones are not being activated, they are in a state of depolarisation, and release a neurotransmitter – rods cells release glutamate, cone cells release acetylcholine. This state of depolarisation is achieved in darkness, because the cells have a high concentration of cGMP, which causes the opening of ion channels. Sodium and calcium ions pass through these ion channels, and its their positive charges that cause the depolarisation of the cell, which leads to the release of neurotransmitters. When light hits the rod and cone cells, the cis-retinene undergoes structural change to become trans-retinene. This structural change causes the activation of transducin, which is a regulatory protein. Transducin activates cGMP phosphodiesterase, which causes the break-down of cGMP into GMP. This action allows the sodium channels to close, thereby preventing influx of positive ions, which leads to hyperpolarisation of the cell, and therefore also preventing the release of neurotransmitters.The breakdown of one molecule of rhodopsin leads to signal amplification, so more molecules of rhodopsin are activated, hence rod cells being highly sensitive to small amounts of light. However, when rod cells are exposed to high levels of light intensity for prolonged periods of time, they become desensitised.
Cone cells function better in higher intensities of light (photopic vision). Most cone cells are found concentrated in the fovea. The fovea is the region of the retina where the retinal layers are parted, allowing light to fall directly onto the cone cells. Cone cells provide greater visual acuity, as each cone synapses with a single interneuron, meaning that the visual signal is not amplified, therefore is more distinct. Cone cells respond to light in the same way as rod cells. The only difference is that the pigment present in cone cells is iodopsin, as opposed to rhodopsin. Retinene that is bound to opsin within the iodopsin is stimulated in the presence of light to undergo structural change to form trans-retinene.
Central Visual Pathways
The optic nerve (CN II) is a paired nerve that carries visual information from the retina to the brain. The ganglion cell axons leave the retina and information passes through the optic nerve to the optic chiasm, where 85-88% of fibres cross over (decussate). The optic tract (the optic nerve fibres) wraps around the cerebral peduncles of the midbrain, where it passes into the lateral geniculate nucleus; which is part of the thalamus. Most of the optic tract axons synapse here, and the remaining fibres branch off and synapse in the pretectal nuclei of the superior colliculi. The integrated visual information is then passed via nerve fibres to the cerebral cortex.
Autonomic Innervation of the Eye
Parasympathetic innervation to the eye is supplied by the oculomotor nerve (CN III). When parasympathetic innervation is predominant, it acts upon the circular muscles of the iris, causing constriction of the pupil.
Sympathetic innervation to the eye is via the cranial cervical ganglion. When sympathetic innervation is predominant, it acts upon the radial muscles of the iris, causing dilation of the pupil.
Reflexes with Optic Nerve as the Sensory Arm
1. Pupillary light reflex: the constriction of a pupil in response to increased light intensity, and a dilatation of a pupil in response to a decreased light intensity. This reflex also involves parasympathetic fibres of the Oculomotor nerve (CN III). The presence of this reflex shows the efficiency of the retina, the optic and oculomotor nerves, and the musculature of the iris.
2. Pupil dilation: also called mydriasis. It is a sympathetic response.
3. Menace response: involves the facial nerve (CN VII) in the motor arm of the reflex. The response also requires integration from the cerebral cortex, the cerebellum and the rostral colliculi. However, the menace response is a learned response, so it will not be present in the first few weeks of life.
4. Fixating response: involves oculomotor (CN III), trochlear (CN IV) and abducens (CN VI) nerves in the motor arm of the reflex.