Pancreas - Anatomy & Physiology
Introduction
The pancreas has exocrine and endocrine tissue. The exocrine part secretes pancreatic juice; a solution containing enzymes for carbohydrate, protein and triacylglycerol digestion. Pancreatic juice drains into the small intestine where it is functional. The exocrine part is the larger of the two parts of the pancreas. The endocrine part secretes hormones for the regulation of blood glucose concentration, including insulin, glucagon and somatostatin. The functional units of the exocrine part are the islets of Langerhans.
Development
The pancreas develops from endoderm, except for the connective tissue which develops from splanchnic mesoderm. Development begins with evaginations of the digestive tube caudal to the stomach. Two pancreatic buds form, one in the dorsal mesogastrium and one in the ventral mesogastrium. Some epithelial cells lose their connections to the developing duct system of the exocrine pancreas and develop into the islets of Langerhans of the endocrine pancreas. As the stomach rotates, the ventral bud moves to become more dorsal. The two buds then fuse; the left lobe is derived from the dorsal bud and the right lobe from the ventral bud. The duct of the ventral lobe (pancreatic duct) joins with the bile duct to form the common bile duct which opens into the duodenum at the major duodenal papilla. The duct of the dorsal lobe (accessory duct) enters the duodenum at the minor duodenal papilla. There is species variation in the persistance of each duct.
Structure
- Located in the craniodorsal part of the abdomen in close association with the duodenum.
- Divided into three parts; a body and left and right lobes.
- The lobes are losely united by interlobular tissue.
- Generally, the portal vein runs between the left and right lobes. (see species differences).
- Rougly "V" shaped in all species.
- As mentioned in the development section, there are two ducts present in the pancreas. Their presence reflects the convergent development pattern of the pancreas. However in some species one or other of the ducts may atrophy.
- The pancreatic duct is the biggest of the two opens into the duodenum with the bile duct at the major duodenal papilla.
- The accessory duct opens on the opposite aspect of the duodenum at the minor duodenal papilla.
Exocrine Function
Endocrine Function
- Functional units are the islets of Langerhans, which are embedded throughout the exocrine tissue.
- Cells of the islets produce hormones that maintain normoglycaemia.
- There are four different cell types within each islet that each produce different hormones.
- α cells produce glucagon
- β cells produce insulin
- δ cells produce somatostatin
- F cells produce pancreatic polypeptide
- Glucagon raises the blood glucose level.
- Insulin decreses the blood glucose level.
- Somatostatin acts in a paracrine fashion to inhibit both glucagon and insulin secretion.
- Pancreatic polypeptide is thought to be a cholecystokinin antagonist, and thus inhibits secretion of pancreatic juice.
Glucagon
- Glucagon secretion is stimulated under conditions of hypoglycaemia and inhibited under conditions of hyperglycaemia. Parasympathetic innervation via the vagus nerve also stimulates release of glucagon.
- Glucagon has a catabolic effect on body reserves.
- The main target tissue is the liver.
- Here it acts primarily to increase the degradation of glycogen via glycogenolysis and to increase the synthesis of glucose from amino acids via gluconeogenesis.
- Glycogen regulates the reaction in glycolysis which converts phosphoenolpyruvate(PEP) to pyruvate. This reaction is catalysed by the enzyme pyruvate kinase and produces a molecule of ATP. Glucagon inactivates this enzyme by phosphorylation via protein kinase A (PKA).
- It increases the β oxidation of fatty acids to provide energy for gluconeogenesis.
- Here it acts primarily to increase the degradation of glycogen via glycogenolysis and to increase the synthesis of glucose from amino acids via gluconeogenesis.
- Glucagon also acts on other tissues, including adipose tissue where it increases the rate of lipolysis and, skeletal muscle where it increases the rate of protein catabolism.
- Glucagon reduces basal metabolic rate.
- Glucagon predominates during fasting metabolism.
- During fasting, the citric acid cycle turns slowly as oxaloacetate is removed to make glucose. Therefore, acetyl CoA (produced from lipolyis and protein catabolism) builds up and is converted to ketone bodies. Ketosis may occur if the situation is prolonged.
Insulin
- Insulin secretion is stimulated under conditions of hyperglycaemia and inhibited under conditions of hypoglycaemia.
- It has an anabolic effect on energy sources.
- It is a small polypeptide consisting of two chains; A and B; which are linked by disulphide bonds.
- It is synthesised inactively as a pre-pro-hormone which undergoes cleavage to produce the active form.
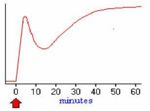
- Insulin is released when blood glucose levels are high. The process of insulin release occurs as follows:
- GLUT 2, which only operate at high glucose concentrations, are present in the plasma membranes of β cells.
- After a meal, glucose concentrations in the blood rise and glucose is taken into the cell.
- Glucose is metabolised inside the β cell which produces ATP.
- ATP inhibits potassium channels which depolarises the plasma membrane.
- Depolarisation causes calcium signalling, which stimulates insulin to be released.
- Pre-formed granules of insulin are release initially, but this supply soon diminishes. This produces a decrease in plasma insulin levels. Insulin levels are restored as de novo insulin is synthesised and secreted.
- Insulin exerts it's anabolic effect on the liver, adipocytes and skeletal muscle.
- It binds to receptors on the cell membrane, which triggers an intracellular signalling cascade.
- This causes preformed granules containing GLUT 4 receptors to be transported and expressed at the cell membrane.
- Cells can now take up glucose from the blood and store it as glycogen or fat.
- Increased glucose levels inside the cell increases the rate of glyogenesis and an increase in the rate of production of triacylglycerides.
- There is an increase in basal metabolic rate in other tissues.
- Insulin regulates the reaction in glycolysis where PEP is converted into pyruvate. This reaction is regulated by the enzyme pyruvate kinase. Insulin activates this enzyme by dephosphorylation via protein phosphatase 1 (PP1). This increases metabolism.
Diabetes Mellitus
- A condition characterised by an inability to maintain normoglycaemia, with persistent hyperglycaemia observed.
- Clinical signs include:
- glucosuria, polyuria and polydipsia - blood glucose concentration exceeds the renal threshold (~10mmol/l) and is excreted into the urine. The increased osmotic potential of the filtrate draws water into the filtrate which is lost in the urine. The animal drinks more to compensate for water loss.
- polyphagia and weight loss - the animal compensates for persistent loss of glucose
- ketosis and ketonuria - ketones are released for energy.
Types of diabetes in dogs
- β cell deficiency - The majority of cases of diabetes mellitus seen in dogs are of this kind. It results in an inability to produce insulin.
- Can be caused by congenital defects, pancreatitis and autoimmunity.
- Insulin antagonism - Seen in females in dioestrus, or in animals with Cushing's (hyperadrenocorticism).
- Progesterone, growth hormone and cortisol are insulin antagonists.
Types of diabetes in cats
- Insulin Dependant Diabetes Mellitus (IDDM); insulin deficiency - similar to human diabetes type 1. There is a failure to produce insulin.
- Can be caused by islet-specific amyloidosis or chronic pancreatitis leading to β cell destrucion.
- Non Insulin Dependant Diabetes Mellitus (NIDDM); insulin antagonism - similar to human diabetes type 2.
- Caused by obesity which leads to carbohydrate intolerance.
Vasculature
Innervation
Lymphatics
Histology
Species Differences
Carnivore
- Portal vein runs between the left and right lobes.
- In dogs, both pancreatic and accessory ducts persist throughout development.
- In cats, the distal part of the accessory duct atrophies during development, so only the pancreatic duct persists.
Ruminant
- Portal vein runs between the left and right lobes.
- In the ox, the distal part of the pancreatic duct atrophies during development, so only the accessory duct persists.
- In sheep and goats the distal part of the accessory duct atrophies during development, so only the pancreatic duct persists.
Horse
- Portal vein perforates the pancreas.
- Both pancreatic and accessory ducts persist throughout development.
Pig
- Portal vein perforated the pancrea.
- The distal part of the pancreatic duct atrophies during development, so only the accessory duct persists.