Spermatogenesis and Spermiation - Anatomy & Physiology
Introduction
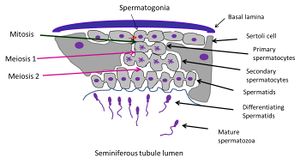
Spermatogenesis is the process of the gradual transformation of germ cells into spermatozoa. It occurs mainly within the seminiferous tubules of the testes and can be divided into three phases, each of which is associated with different germ cell types:
- Proliferative phase: spermatogonia → spermatocytes
- Meiotic phase: spermatocytes → spermatids
- Differentiation phase (also known as spermiogenesis): spermatids → spermatozoa
Unlike the female production of gametes which occurs entirely before birth, with gamete maturation occurring in a pulsatile fashion after puberty, males produce gametes continuously from puberty onwards for the rest of their reproductive lives and the release of the gametes is constant.
The seminiferous tubules are the site of spermatogenesis. The two main cell types within the tubules involved in spermatogenesis are the germ cells, which will develop into sperm, and somatic cells known as Sertoli cells, which nuture the germ cells throughout the development process.
As the germ cells progress through their stages of development they move slowly from the basement membrane of the tubules through the tight junctions between the Sertoli cells into the tubular lumen.
Stages of spermatogenesis
Proliferation phase
Stem or A spermatogonia located in the basal region of the tubular epithelium undergo mitosis. The progeny of these divisions maintain their own numbers as well as giving rise to several interconnected B spermatogonia (the number of these arising from a single A spermatogonia is species dependent). B spermatogonia divide to give rise to primary (1o) spermatocytes. All descendants of a B spermatogonium remain connected by cytoplasmic bridges, forming a syncytium - like cell clone which undergoes synchronous development.
Meiotic phase
Each 1o spermatocyte divides to give rise to two short-lived secondary (2o) spermatocytes, which in turn give rise to two spermatids each. The spermatids contain a haploid number of chromosomes (half the number of a somatic cell). 1o spermatocytes are the largest cells in the spermatogenic series and are located approximately midway within the seminiferous epithelium.
The process of meiosis occurs over a long period, with prophase of the first meiotic division taking up to three weeks [1]
Differentiation phase
This phase is also known as spermiogenesis.
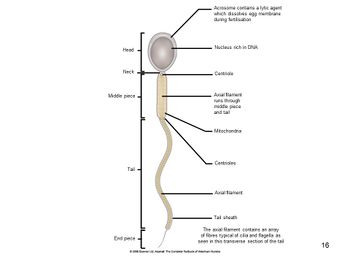
Spermatids undergo transformation into spermatozoa. Many changes occur within the cells, the three major ones being:
i) formation of the acrosome, which covers the cranial part of the head. The acrosome will contain hydrolytic enzymes to allow fusion of sperm and egg for fertilisation.
ii) condensation of nuclear chromatin in the head to form a dark-staining structure
iii) growth of the tail opposite the acrosome, and loss of excess cytoplasmic material which is shed as a residual body. The body is phagoctosed by the Sertoli cells.
The morphological changes occurring during this process can be seen if sections of different seminiferous tubules are examined.
For a diagrammatic representation refer to Figure 2.
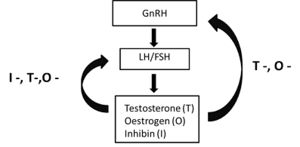
Hormonal Control of spermatogenesis
Spermatogenesis is controlled by a complex feedback mechanism involving the hypothalamus, anterior pituitary and testes. Gonadotrophic releasing hormone (GnRH) is released by the hypothalamus in a pulsatile manner and travels through portal vessels to the anterior pituitary, where it acts of the gonadotrophic cells. These cells respond to the stimulation by producing either follicle stimulating hormone (FSH) or luteinising hormone (LH) depending on the pattern of GnRH secretion.
LH and FSH travel in the bloodstream to the testes, where LH acts on the Leydig cells to stimulate them to convert steroids to testosterone and other androgens, which in turn contribute to the stimulation of Sertoli cells.
FSH acts on the receptors of Sertoli cells and, in combination with testosterone, stimulates many functions, including synthesis and secretion of oestrogen, inhibin and many other products, meiosis, spermatocyte maturation and Leydig cell function.
Inhibin, testosterone and oestrogen feedback negatively on the anterior pituitary and hypothalamus to suppress secretion of gonadotrophic hormones (Figure 3).
Webinars
References
- ↑ Hess RA, Spermatogenesis, overview. In: Knobil E, Neil JD (eds.), Encyclopedia of Reproduction. New York: Academic Press; 1999: pp. 539–545
Cunningham, JG and Klein, BG (eds)(2007) Textbook of Veterinary Physiology. Saunders Elsevier.
| Spermatogenesis and Spermiation - Anatomy & Physiology Learning Resources | |
|---|---|
 Selection of relevant videos |
Dissection of the equine testicle |
 Selection of relevant PowerPoint tutorials |
Histology of the Male reproductive tract |
Webinars
Failed to load RSS feed from https://www.thewebinarvet.com/urogenital-and-reproduction/webinars/feed: Error parsing XML for RSS