Uterine Contraction - Anatomy & Physiology
Jump to navigation
Jump to search
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
|
|
Myometrial Contraction
- Myometrium consists of:
- Non-striated smooth muscle fibres
- Nerves, Blood and Lymph
- During pregnancy, Oestrogens stimulate muscle cell hypertrophy.
- Myometrial cells behave as a functional syncytium, being electrically coupled via specialised regions of contact known as gap junctions/nexi.
- The combination of the above factors allows strong, coordinated myometrial contraction.
- Excitation of smooth muscle depends on alteration in membrane potential. Myometrial cells must be depolarised (-50mV) to achive contraction.
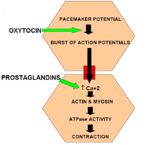
- Spontaneous depolarizing pacemaker potentials occur. If the magnitude of these exceeds the critical threshold, a burst of action potentials will fire.
- This causes calcium influx from endoplasmic reticular stores and extracellular fluid.
- Intracellular calcium binds to regulatory sites on actin and myosin, allowing expression of ATPase, thus causing contraction.
- Uterine contractions increase in both frequency and amplitude during labour. This causes an increase in uterine pressure from 10mmHg to 50-100mmHg.
The Birth Canal
Brachystasis
- Myometrial cells contract and shorten, but do not regain their original length upon relaxation.
- Reduces the uterine volume and causes retraction of the lower uterine segment and the cervix to create a birth canal.
Retraction Ring
- The Uterus is divided into two segments:
- Upper segment: contractile
- Lower segment: passive
- The junction between these segments is the retraction ring.
- Palpation of the retraction ring is used as an indicator of progression through labour.
Endocrine Control
- Two hormones directly regulate myometrial contractions:
- Oxytocin: from the posterior pituitary gland (not the corpus luteum) lowers the excitation threshold of muscle cells to increase the likelihood of action potential firing. Oxytocin also stimulates prostaglandin release.
- The uterine Oxytocin receptor is a G protein coupled receptor with a Gαq subinit. Thus the signalling pathway is via a calcium second messenger. Hence prostaglandin and oxytocin are complementory in action.
- Prostaglandins: Stimulate liberation of calcium from intracellular stores to cause the rise in intracellular calcium concentration required for myometrial contraction.
- Oxytocin: from the posterior pituitary gland (not the corpus luteum) lowers the excitation threshold of muscle cells to increase the likelihood of action potential firing. Oxytocin also stimulates prostaglandin release.