Ear - Anatomy & Physiology
|
|
Introduction
The ear is a paired sensory organ, that is involved in both hearing and balance. For this reason, the ear is known as the vestibulocochlear organ.
Sound waves that are transmitted into the ear provide a mechanical stimulus. These mechanical stimuli are then transferred into electrical signals by the cochlea. Neuroreceptors in the ear allow the animal to gain a perception of position and movement.
Structure
Anatomically, the ear can be looked at in three parts:
1. Outer ear - pinna and auditory canal
2. Middle ear - contains the malleus, incus and stapes bones - known as the ossicles
3. Inner ear - contains the membranous and bony labyrinths, and the cochlea
Outer Ear
The pinna ( or auricle) is defined as the outer projecting part of the ear, that is the part of the ear that can be seen. It consists of the auricular cartilage, surrounded by skin, which allows for flexibility and elasticity. The auricular cartilage connects to scutiform cartilage, which itself connects to annular cartilage, which allows for articulation. These cartilages fit into the bony passage of the ear canal - also called the external auditory meatus, which leads to the tympanic membrane. This is the deepest boundary of the outer ear.
Foreign bodies can become lodged in the external auditory meatus, but glands are present that produce wax which can trap these.
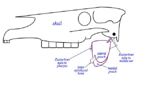
Muscles around the base of the ear that are attached to the skull allow movement of the pinna, so the ear can be directed to the source of sound:
| Muscle | Origin | Innervation | Function |
|---|---|---|---|
| Preauricular | Deep temporal fascia | Auriculopalpebral branch of facial nerve
(cranial nerve VII) |
Moves the ear cranio-laterally, so the pinna is facing forwards |
| Ventroauricular | Laryngeal fascia | Retroauricular branch of facial nerve
(cranial nerve VII) |
Moves the ear laterally |
| Postauricular | Medial cervical raphe | Retroauricular branch of facial nerve
(cranial nerve VII) |
Moves the ear caudo-laterally, so the pinna is facing backwards |
Middle Ear
- The middle ear consists of the tympanic cavity, the auditory ossicles and the eustachian tube. The boundary between the middle and inner ear is the oval window.
- The auditory ossicles are attached to the wall of the tympanic cavity by many ligaments and mucosal folds.
- The tympanic cavity is located within the petrous temporal bone, and can be divided into dorsal, middle and ventral parts:
- Dorsal: contains the auricular ossicle
- Middle: contians the tympanic membrane within its lateral wall, and opens rostrally into the nasopharynx via the eustachian tube
- Ventral: the tympanic bulla - a thin-walled, bulbous expansion of the temporal bone, which houses an extension of the tympanic cavity
- The oval window is positioned rostrodorsally, to which one end of the stapes is attached by an annular ligament. It functions to connect the tympanic cavity with the inner ear.
- The round window is positioned more caudally, and leads to the cavity of the cochlea.
- Sound vibrations are transmitted from the tympanic membrane, across the tympanic cavity, via the ossicles (malleus, incus, then stapes).
- The ossicles, as well as transmitting sound vibrations from the tympanic membrane, also magnify the vibrations by about 20 times. This is necessary for initiating waves in the endolymph of the cochlea. The magnification is achieved by the action of two muscles that are attached to the ossicles, and which act as antagonists of each other. These two muscles are the tensor tympani muscle and the stapedius muscle. The tensor tympani muscle originates within the tympanic cavity, and inserts on the malleus. The contraction of this muscle creates tension of the ossicles, and therefore also of the tympanic membrane, all of which results in greater sensitivity. The stapedius muscle originates from the wall of the tympanic cavity, and inserts on the stapes. Contraction of this muscle pulls the end of the stapes away from the oval window, thereby reducing the fource of the transmission of sound vibrations.
- The eustachian tube connects the tympanic cavity to the nasopharynx, which mark the beginning and end of the eustachian tube, respectively.
- The eustachian tube functions to equalise pressure on either side of the tympanic cavity, by opening while yawning or swallowing, for example.
Inner Ear
- The inner ear is located within the petrous temporal bone.
- The inner ear contains the membranous labyrinth, which is surrounded by the bony labyrinth.
- The membranous labyrinth is an interconnected group of fluid-filled membranous sacs. The fluid is endolymph.
- It is the movement of the endolymph that stimulates the sensory cells within the membranous wall.
- The membranous labyrinth consists of:
- vestibular labyrinth: contains the receptor organ involved with balance, containing the saccule, utricle and the semicircular ducts. The saccule and utricle contain sensory maculae within their walls, and there's a sensory crista within the ampullae of the semicircular ducts. The maculae and ampullae sense and conduct impulses concerned with balance via the vestibular nerve. The three semicircular ducts arise from the utricle, and the cochlear duct arises from the saccule.
- cochlear labyrinth: contains the organ involved with hearing. It consists of the organ of Corti, within the cochlear duct. The cochlear duct is fluid-filled, the fluid being endolymph. The organ of Corti contains the receptor cells for hearing.
- ductus reuniens: this is the duct through which the above two labyrinths communicate
- The bony labyrinth consists of:
- vestibule: a chamber in the centre of the bony labyrinth, which communicates with both the cochlea and the semicircular canals. The oval and the round windows are both located in the lateral wall of the vestibule.
- semicircular canals: contain the semicircular ducts, which have arised from the utricle of the vestibular labyrinth. There are three semicircular canals, corresponding to the three dimensions in which you can move, so they are almost at right angles with each other. Each duct has two crura (leg-like parts). One crus of each duct has an ampulla, which is an expansion of the duct. Movement of endolymph stimulates receptor cells within the ampullae.
- cochlea: forms a spiral around a central hollow core of bone, called the modiolus,which contains the cochlear nerve. The spiral lamina projects into the spiral canal, partially bisecting the lumen into two parts, which are called the scala tympani and the scala vestibuli. The scala media (the cochlear duct) is inbetween these two parts.
The external ear receives sounds, which cause vibrations of the tympanic membrane. These vibrations move along the ossicles of the middle ear, to be transmitted to the inner ear. The stapes is connected to the oval window, so when the stapes transmits vibrations, this causes movement of perilymph that is in the inner ear. The movement of the perilymph is transmitted via the scala vestibuli and the scala tympani, to the round window, where it induces movement of the secondary tympanic membrane. This results in the movement of the endolymph of the cochlear duct, causing pressure on the tectorial membrane, which then induces pressure on the sensory hairs, stimulating the receptor cells within the cochlear duct to send impulses to the spiral ganglion. The axons of the spiral ganglion form part of the vestibulocochlear nerve.
Function - Hearing
The Outer and Middle Ear
- Sound is transmitted from the tympanic membrane to the oval window, via first of all the ossicles (malleus, incus, stapes), then the middle ear wall, then the middle ear cavity:
tympanic membrane → ossicles → middle ear wall → middle ear cavity → oval window
- Amplification due to the bony lever is only 1.5times, as the stapedius muscle prevents the stapes from vibrating too much.
- The tympanic membrane is 20 times larger than the oval window.
The Cochlea
- The entire basilar/Reissner's/ hair cells/scala media complex vibrates within the surrounding perilymph.
- It is not that a travelling wave passes along the cochlea, rather a standing wave is established within the resonant tube of the cochlea.
- Displacement of the basilar membrane during sound transmission is 200 times that of the tympanic membrane.
- This is due to the relative inertia of the tympanic membrane, so it remains relatively still as the basilar and hair cells move relative to it.
The Hair Cell Receptor
- Hair cells discharge in relation to the excursion (a range of movement regularly repeated in performance of a function) of the basilar membrane.
- The tips of the cilia are embedded in the tectorial membrane, and so are flexed by sound vibrations.
- Each cilium contains mechanically-gated non-selective cation channels. Potassium ions (K+) are the main cations in endolymph.
→ → → →
cilium flexes → gK+ ↑ → depolarisation → transmitter release ↑
← ← ← ←
cilium flexes → gK+ ↓ → hyperpolarisation → transmitter release ↓
This shows that if the cilia is pushed in one direction, it will be excited, but if pushed in the other direction it will be inhibited.
Hair Cell Resting Potentials
- Hair cells discharge at up to 300Hz and are very sensitive, due to the unique nature of endolymph encouraging K+ influx into hair cells.
- Cilia are in endolymph, but hair cell body is in perilymph.
- There is a high concentration of potassium ions (K+) in endolymph, which is maintained by ion pumps in the stria vascularis.
Cochlear Microphonics
- The importance of this is uncertain.
- It is the summated activity of hair cells, measurable at the round window.
- Non-nervous: no latency, refractoriness, and persists after death.
- Generated by hair cells.
Tone
1. The Place Principle: The physical properties of the basilar membrane change along its length. Dampening of sound waves by the basilar membrane is critical for determination of pitch:
- high frequencies are dampened out first in the basal, thinner/narrower/stiffer part
- low frequencies reach the apical thicker/wider/more pliant part
2. Lateral Inhibition: allows discrimination of two similar frequencies. It is an active process affected by olivocochlear efferents. It occurs by driving contractions of the outer hair cells which vibrate the membrane.
3. Phase Locking: allows extremely fine discrimination of pitch within the musical range. The action potential occurs at a particular point in the sound wave. The brain can determine frequency information from this.
Direction Discrimination
Outer ear:
1. Pinna shape (most mammals)
2. Pinna mobility (not primates)
Centrally:
1. Phase difference
2. Change in phase difference when head is moved
3. Head 'shadowing' of sound
Deafness
- Conduction Deafness: an interruption in the conduction of sound waves. May be caused by otitis, wax, tumours or tympanic rupture.
- Nerve Deafness: hearing loss due to a lesion to the auditory nerve within the central neural pathway. May be congenital or genetic, for example in white cats with blue eyes or in dalmatians, a problem created due to highly selective in-breeding. Histological examinations carried out on the organ of Corti from affected dogs shows the absence of sensory cells. Nerve deafness may also be due to age.
Central Auditory Pathways
- The signal that has been created from the sound waves that were picked up by the ear, is carried to the brain by the vestibulocochlear nerve (CN VIII), which synapses in the cochlear nucleus.
- From here, the auditory information is then split.
- Those nerve fibres that travel to the ventral cochlear nuclear synapse on their target cells. The ventral cochlear nuclear cells then project to a group of cells within the medulla, called the superior olive nucleus. It is here that the timing and loudness of the sound that was picked up in each ear is compared, allowing determination of the direction that the sound came from. This information is then transferred via the lateral lemniscus to the inferior colliculus.
- The other nerve fibres start in the dorsal cochlear nucleus. It is here that the quality of sound is determined, as it compares the frequency differences. This pathway leads directly to the inferior colliculus, via the lateral lemniscus.
- Both of the above pathways are bilateral. This means that if there is a lesion at any point along the pathway, it usually has no effect on hearing. Deafness is only usually caused if there is damage to either the auditory nerve, the cochlea, or the middle ear.
- From the inferior colliculus, the information from both pathways is sent to the medial geniculate nucleus of the thalamus, which then leads on to the primary auditory cortex of the cerebral cortex.
Vestibular Receptors and Balance
- The vestibular sense is rather more unconscious than that of hearing.
- The vestibular labyrinth, that is contained within the bony labyrinth of the inner ear is the part of the ear that is involved with the vestibular sense - balance.
- The vestibular labyrinth contains the saccule, the utricle and the semicircular ducts - the semicircular ducts being housed within the semicircular canals.
- There are sensory hair cells within the vestibular labyrinth, similar to those in the other regions of the inner ear, which detect movement.
- However, these sensory hair cells are lodged in the ampullary cupulae or in otoliths (minute calcareous particles), rather than in the tectorial membrane as in the rest of the ear.
- The ampulla is a swelling at the base of the semicircular ducts. The sensory hair cells project upwards from the ampulla into the cupula, which is a gelatinous mass. The ampullary cupulae detect flow around the semicircular canals, which are filled with endolymph, and there is an inertia of fluid for detection of angular acceleration. Angular acceleration is the detection of motion of the head in any direction.
- Otoliths are denser than endolymph - they are calcareous and crystalline. They are contained within the maculae, and detect gravity and linear acceleration. Linear acceleration is the detection of motion along a line, for example when you lean to one side.
- Movement of the sensory hair cells triggers impulses, which are carried by the vestibular portion of the vestibulocochlear nerve (CN VIII).
Unilateral Vestibular Signs
- The vestibular system is a common site for pathology. Brain infection, tumours and inflammation are often shown up by vestibular signs. These signs may include:
1. Head tilt towards the lesion
2. Fall towards the lesion
3. Turn towards the lesion
4. Vomiting - due to the connection to the vomiting centre of the brain
5. Nystagmus with slow phase to lesion - nystagmus is rapid, involuntary, oscillatory motion of the eyeball in any direction, and can be caused by a lack of coordination
Central Vestibular Pathways
- The sensory hair cells produce signals, which are carried by the vestibulocochlear nerve (CN VIII) first of all through the bipolar vestibular ganglion cells.
- Most nerve fibres that have come from the hair cells terminate in the vestibular nuclei, which are located in the fourth ventricle of the cerebral cortex.
- After entering the vestibular nuclei, some of the processes of the nerve fibres divide into ascending and descending branches. Some processes pass directly into the cerbellum.
Vasculature
- The medial, intermediate and lateral auricular rami supply the outer ear, all of which are branches of the great auricular artery, which itself is a branch of the external carotid artery.
- The tympanic membrane is highly vascularised.
Innervation
Sensory innervation to the outer ear:
- Ce2 (second cervical spinal nerve) to medial pinna
- Auriculopalpebral branch of trigeminal nerve (CN V) to most of the lateral pinna
- Facial (CN VII) and vagus nerves (CN X) via small auricular branches to pinna
Sensory innervation to the inner parts of the ear is provided by the vestibulocochlear nerve (CN VIII).
Innervation to the muscles of the middle ear:
- The tensor tympani muscle is innervated by the pterygoid nerve, which is a branch of the mandibular nerve, itself being the third branch of the trigeminal nerve (CN V).
- The stapedius muscle is innervated by the facial nerve (CN VII).
Equine Guttural Pouch
- The guttural pouch is an anatomical structure that is only found in the horse (and other perissodactyla).
- The guttural pouches are paired ventral diverticulae of the eustachian tubes, formed by escape of mucosal lining of the tube through a relatively long ventral slit in the supporting cartilages.
- Each pouch attains a capacity of 300-500ml and is air-filled.
- The stylohyoid bone partially divides each of the guttural pouches into lateral and medial compartments - the medial compartment being approximately double the size of the lateral one and extends further caudally and ventrally.
Surrounding Gross Anatomy
- Dorsal to Guttural Pouch: ventral surface of the skull/the wing of atlas.
- Ventral to Guttural Pouch: pharynx and beginning of oesophagus; medial retropharyngeal lymph node between pharynx and ventral wall of pouches.
- Lateral to Guttural Pouch: pterygoid muscles, and parotid and mandibular salivary glands.
- Medial to Guttural Pouch: right and left pouches separated dorsomedially by rectus capitis ventralis and longus capitis muscles; below this by fused walls of the two pouches forming the median septum.
Blood Vessels and Nerves
Several cranial nerves and arteries lie directly against the pouch as they pass to and from foramina in the caudal part of the skull (vessels within mucosal folds that indent the pouches):
- Medial Compartment:
- Cranial nerves IX, X, XI, XII.
- Continuation of the sympathetic trunk beyond the cranial cervical ganglion.
- Internal carotid artery.
- Lateral Compartment:
- Cranial nerve VII - limited contact with the dorsal part of the compartment.
- External carotid artery crosses the lateral wall of the lateral compartment in its approach (as maxillary artery) to the atlas canal. The external maxillary vein is also visible.
The pouch also directly covers the temporohyoid joint.
Drainage
- Natural drainage of the pouch is throught the slit-like (pharyngeal) openings of the eustachian tube in the lateral wall of the nasopharynx.
- The connection opens when the horse swallows and grazing normally provides drainage. However, most of the pouch is ventral to his slit, and therefore drainage may be rather ineffective. If blocked, secretions accumulate and the pouch distends producing a palpable swelling.
Clinical Conditions
1. Guttural Pouch Empyema:
- Purulent material in pouch. Respiratory infections can extend into the pouches from the pharynx or from retropharyngeal lymph nodes.
- Secretion/pus accumulates. The pouch distends forming a palpable, fluctuating visible swelling behind the jaw.
- Seen as a fluid line in standing lateral radiograph of guttural pouches. Can be surgically drained or with catheter.
- Material can become chondroid - hard concretions of pus - removed by surgery.
2. Guttural Pouch Mycosis:
- Fungal infections (Aspergillosis).
- Typically affect caudodorsal medial compartment.
- Signs: painful swelling in parotid region, abnormal carriage of head and neck, nasal discharge, and the horse may be head shy.
- Erosion of the roof of the guttural pouch produces a variety of signs by damage to important structures directly related to the pouch:
a) Epistaxis: nasal bleeding. Erosion of internal carotid artery severe, maybe even cause fatal haemorrhage.
b) Dysphagia: difficulty in swallowing. Paresis of the pharynx and soft palate is caused by lesions involving the glossopharyngeal and vagus nerves.
c) Laryngeal Hemiplegia: roaring - following vagus involvement.
d) Horner's Syndrome: nasal congestion, drooping of upper eyelid, miosis, sweating and hyperaemia on same side of face. From involvement of sympathetic nerve (cranial cervical ganglion).
e) Facial Paresis: rare.
f) Tongue Paralysis: rare.
g) Vestibular Signs and Arthritis: alanto-occipital joint - very rarely.
3. Guttural Pouch Tympany:
- Foals up to one year of age. The guttural pouch fills with air, but cannot escape through the pharyngotubal opening (acts as a one-way valve allowing air to be drawn into the pouch, but not expelled from it). Usually there is no gross abnormality of the opening.
- Visible external swelling and large pouch on radiographs.
- Consequences: collapse of pharyngeal roof, and therefore dysphagia.
- Unilateral tympany can be treated by forcing an opening in the median septum (fenestration) so that both pouches communicate with the pharynx through a single opening.
- Bilateral tympany - parts of the flaps guarding the openings may have to be removed.
Inspection/Imaging of the Pouches
1. Visual observation and palpation.
2. Radiography.
3. Endoscopy - performed by passing an endoscope tube through the ventral nasal meatus and into the pharyngeal opening of the eustachian tube, and thus into the guttural pouches. Draining can be performed by passing a catheter along the same route.
4. Ulstrasonography.
5. Open surgery - best under general anaesthetic - three routes of access:
- Viborg's Triangle: incision between tendon of the sternocephalicus muscle, linguofacial vein and ramus of mandible. (Distance between triangle and pouch is greatly reduced when pouch is enlarged).
- Hyovertebrotomy: incision ventral to wing of atlas.
- Modified Whitehouse Approach: skin incision ventral to linguofacial vein, then blunt dissection along larynx to guttural pouch.
Function(s)
Largely unknown, however hypotheses have been put forward:
- Influences internal carotid artery blood pressure. Air pressure varies with phase and forcefulness of respiration. Artery in mucosal fold exposed sufficiently to be affected.
- Cerebral blood cooling mechanism. Operates at times of physical stress, when core body temperature is raised. Vigorous respiration, cool air in guttural pouches, and exposed artery, all leads to cooling of the blood.
Histology
- Tympanic Membrane: the outer surface is lined with an epithelium that is continuous with that of the external acoustic meatus. The inner surface is lined by the mucosa that lines the tympanic cavity. This inner mucosal layer is made up of simple squamous epithelium.
- Tympanic Cavity: lined by a single-layer of epithelium, and the underlying soft tissue has a rich vascular and nervous supply. The single-layered epithelium also covers the ossicles and the tympanic membrane.
- Saccule and Utricle: lined by simple squamous epithelium, underneath which is a layer of loose connective tissue.
- The connective tissue component of the organ of Corti is the basilar lamina.
Species Differences
- The Cochlea: the spiral has 3 turns in carnivores, 2.5 turns in horses, 4 turns in the pig, and 3.5 turns in ruminants.
- The shape of the pinna varies between breeds and species.
- Fish: to detect high frequency sound, some fish use the swim bladder as an acoustic detecror. It is connected to the lagena (the stumpy piscine cochlea) by three Weberian bones. These are derived from vertebrae.