Equine Endocrine System - Horse Anatomy
| This article is still under construction. |
Hypothalamus
Pituitary Gland
The pituitary gland, or hypophysis is an elongated appendage of the brain lying within a bony cavity of the sphenoid bone in the base of the skull - the Sella Turcica. The hypophysis is suspended ventral to the the hypothalamus by a thin infundibular stalk. It lies between the more rostral optic chiasma, and the more caudal mammillary bodies, separated from the brain by a fold of dura mater known as the diaphragma sellae. The gland is divided into anterior and posterior, with different embryological origins reflecting a difference in function.
Posterior pituitary (Neurohypophysis)
Consisting of the Pars Nervosa, this section is derived from a downgrowth of neural tissue from the hypothalamus. As such, it is a collection of axons and nerve terminals that originate in the paraventricular and superoptic nuclei of the hypothalamus. The pars nervosa stores and releases oxytocin and antidiuretic hormone (ADH).
Anterior pituitary (Adenohypophysis)
Consisting of the Pars Tuberalis and Pars Distalis this part has an embryological origin as an epithelial upgrowth from the foetal oral cavity called Rathke's Pouch.
Pars Tuberalis
The pars tuberalis is a thin band of endocrine cells around the infundibular stalk. It is dense in melatonin receptors, and functions to regulate release of reproductive hormones according to season.
Pars Distalis
The pars distalis contains five cell types (somatotropes, lactotropes, corticotropes, thyrotropes and gonadotropes). The endocrine cells within the pars distalis synthesize, store and release six hormones in response releasing and inhibiting factors from the hypothalamus. These factors reach the pars distalis in the hypophyseal portal system, which connects capillaries of the median eminence to the capillaries of the pars distalis. The hormones produced are growth hormone (GH), follicle stimulating hormone (FSH), luteinising hormone (LH), adrenocorticotrophic hormone (ACTH), thyroid stimulating hormone (TSH) and prolactin (PRL). For further information on each of these hormones, click here.
Pars Intermedia
This is the residual lumen of Rathke's Pouch and consists of a series of small cystic cavities (follicles filled with colloid), with both basophillic and chromatophobic (poorly staining) cell types. These extend into the pars nervosa.T The pars intermedia separates the anterior and posterior lobes. Endocrine cells in this region are known as melanotropes. These convert the prohormone pro-opiomelanocorticotropin (POMC) to melanocyte stimulating hormone (a-MSH) and corticotropin-like intermediate lobe peptide (CLIP). The pars intermedia is innervated by dopaminergic neurones originating in the periventricular nucleus of the hypothalamus.
Thyroid Gland
The thyroid gland lies in the neck, on either side of the second and third tracheal rings on their ventral aspect. It consists of left and right lobes, which are connected at their caudal aspect by a strand of connective tissue known as the isthmus. In the horse, the two lobes of the thyroid are oval in shape and roughly the size of a plumb.
Two types of hormones are produced by the thyroid gland. This first type is the iodine containing hormones; tri-iodothyronine(T3) and thyroxine (T4), which are produced by follicular cells. These thyroid hormones regulate the basal metabolic rate and are important in growth, regulation of body temperature and carbohydrate metabolism. Their release is stimulated by thyroid stimulating hormone (TSH) from the pituitary. The second type of hormone produced from parafollicular (C-cells) of the thyroid gland is calcitonin, which regulates blood calcium levels along with parathyroid hormone and acts to reduce blood calcium by inhibiting its removal from bone.
Vasculature
The main blood supply is via the cranial thyroid artery, which is a branch of the common carotid artery. There is a minor contribution from the caudal thyroid artery. Venous drainage is via the cranial and middle thyroid veins, which drain into the external jugular vein.
Lymphatics
The thyroid drains to the deep cervical thoracic lymph node or the tracheal trunk.
Innervation
- Sympathetic: Supply from the cranial cervical ganglion.
- Parasympathetic: Supply from branches of cranial and caudal laryngeal nerves, which themselves branch from the vagus nerve.
Parathyroid Glands
The parathyroid glands are multiple (generally four) small glands, approximately 1-2mm in length are located about the cranial trachea. There are two internal glands embedded within the cranial thyroid glands, and two external glands along the trachea, close to the caudal deep cervical lymph nodes. The parathyroid glands produce parathyroid hormone (PTH), which regulates serum calcium and phosphorus concentrations.
Vasculature
The parathyroid glands are surrounded by a capillary network which arises from branches of the common carotid artery. Venous drainage is via the jugular vein.
Lymphatics
The parathyroid glands drain to the deep cervical lymph nodes.
Innervation
- Sympathetic: From the cranial cervical ganglion
- Parasympathetic: Run with branches of the caudal laryngeal nerve
Adrenal Glands
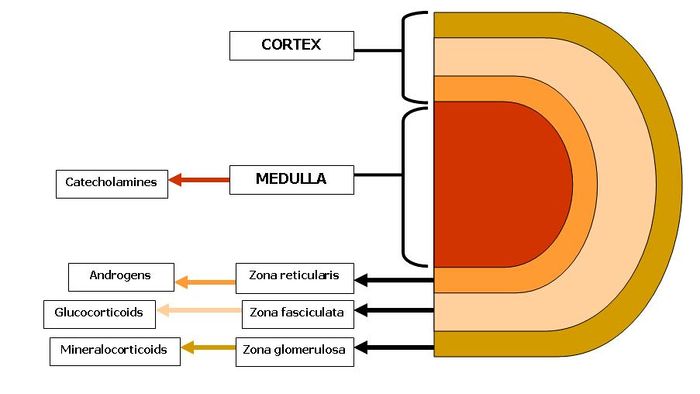
The adrenal glands are paired bodies lying cranial to the kidneys within the retroperitoneal space. The glands consist of two layers; the cortex and medulla.
The adrenal cortex is red to light brown in colour and is composed of three zones. These zones all produce hormones derived from cholesterol, which is abundant in the cells. From the outer to inner, the layers are:
1. Zona Glomerulosa: Secretes mineralocorticoids
2. Zona fasciculata: Secretes glucocorticoids
3. Zona Reticularis: Secretes sex steroids or androgens
The adrenal cortex represents 80-90% of the adrenal gland.
The adrenal medulla is primarily involved in the production of catecholamines; epinephrine and norepinephrine. In fetal life, the adrenal medullaplays a role in the autonomic nervous system. The medulla acts as a sympathetic ganglion with the postganglionic cells lacking axons. Through sympathetic preganglionic fiber stimulation, the medullary cells secrete catecholamines. The adrenal medulla represents only 10-20% of the adrenal gland.