Difference between revisions of "Kidney Hormonal Regulators - Anatomy & Physiology"
| Line 20: | Line 20: | ||
====Effects of Angiotensin 2 on Blood Pressure==== | ====Effects of Angiotensin 2 on Blood Pressure==== | ||
| − | '''Angiotensin 2''' acts on '''AT1 receptors''' to stimulate the release of | + | '''Angiotensin 2''' acts on '''AT1 receptors''' to stimulate the release of '''Aldosterone''' from the [[Adrenal Glands - Anatomy & Physiology#Adrenal Glands|Zona Glomerulosa]] of the adrenal glands. This mineralocorticoid increases the reabsorption of sodium and therefore water and chloride from the distal tubule thus helping to increase blood volume and pressure. It also stimulates the thirst center and increases the secretion of [[Pituitary Gland - Anatomy & Physiology #Posterior Pituitary Gland | ADH]] to help increase blood volume. Thanks to the RAAS pressure can return to 50% baseline within 15 minutes of haemorrhage. |
====Effects of Angiotensin 2 on GFR==== | ====Effects of Angiotensin 2 on GFR==== | ||
Revision as of 12:07, 5 September 2008
|
|
The Renin Angiotensin Aldosterone System (RAAS)
- Allows an animal’s salt intake to vary without any great affect on ECF volume or arterial pressure
- If an animal’s salts intake increased 50x its blood pressure would only increase 5-6mmHg
- Without the RAAS it would go up 10x that amount
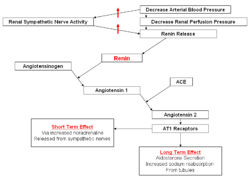
The System
In the event of blood pressure dropping increased Renin is secreted due to the decreased stretch of the juxtaglomerular cells and an increased sympathetic stimulation triggered by the decreased activation of arterial baroreceptors. This enzyme cleaves the alpha glycoprotein Angiotensinogen which is released from the liver. This produces Angiotensin 1 which is further converted by Angiotensin Converting Enzyme (ACE) to Angiotensin 2 mainly in the lungs but to a much lesser extent locally in the kidneys. Angiotensin 2 then works to restore blood pressure. In this section we cover its effects on and through the kidneys.
Effects of Angiotensin 2 on Blood Pressure
Angiotensin 2 acts on AT1 receptors to stimulate the release of Aldosterone from the Zona Glomerulosa of the adrenal glands. This mineralocorticoid increases the reabsorption of sodium and therefore water and chloride from the distal tubule thus helping to increase blood volume and pressure. It also stimulates the thirst center and increases the secretion of ADH to help increase blood volume. Thanks to the RAAS pressure can return to 50% baseline within 15 minutes of haemorrhage.
Effects of Angiotensin 2 on GFR
If blood pressure drops then GFR would also drop due to a reduced blood flow through the kidneys. Therefore it is important to prevent this. If contraction of the efferent arteriole occurs then the pressure difference between the afferent and efferent arterioles increases creating a greater filtration pressure. This effect is mediated by Angiotensin 2 and means that when blood pressure falls there is minimum alteration of GFR. Blood flow which is already reduced due to the reduced pressure will then be further reduced by the increase in resistance. This increased renal resistance to blood flow and the maintained GFR has many advantageous effects.
Advantages of Constriction of the Efferent Arteriole
- If you increase the resistance in the kidneys you contribute to increasing total peripheral resistance. This helps to return blood pressure towards normal. (Angiotensin 2 also has vasoconstrictive effects in other organs.)
- The kidneys can tolerate the reduced perfusion allowing blood to be prioritised to organs which need it like the brain and heart.
- The constriction of the efferent arterioles also reduces hydrostatic pressure in the Peritubular Capillaries this increases reabsorption of water and salt thus helping to restore the ECF and thus helps to normalise blood pressure.
- The amount of waste excreted is variable with GFR. Thanks to the normalised GFR the excretion of waste products such as urea is maintained.
Effects of Angiotensin 2 On Sodium
- Induces insertion of Na+ channels into renal tubules via stimulation of AT1 receptors
- Proximal tubule:
- Apical - Na+/H+ exchangers
- Basolateral Na+(HCO3-)3 and Na+K+ATPase
- Thick ascending limb
- Apical Na+/H+ exchangers and Na+K+2Cl- symporter
- Collecting Duct
- Epithelial Na+ channel
- Also stimulates Aldosterone
Aldosterone
Aldosterone is a steroid hormone which is secreted from the zona glomerulosa of the adrenal gland. It has a mineralocorticoid activity and is the most important regulator of plasma potassium. When plasma potassium increases increased stimulation of aldosterone occurs directly and as a result of Renin-Angiotensin-Aldosterone System (RAAS). It is also the most important regulator of sodium excretion.
Release
- Release is stimulated by 3 things
- Corticotropin (ACTH)
- Angiotensin 2
- K+
- Its release is inhibited by Atrial Natriuretic Peptide
- Most increases in the concentration of aldosterone however can be explained by increases in the Renin-Angiotensin-Aldosterone System and therefore angiotensin 2 and/or by increases in K+ concentration
- Only in severe fluid loss does ACTH significantly stimulate the release of aldosterone
- ANP is secreted in response to sodium/water loading and therefore inhibits aldosterone secretion
Action
- Diffuses across the cell membrane - lipophillic (essentially steroidal)
- Of the principal cells of distal tubule and Collecting Duct
- Binds to cytoplasmic receptors
- Works by altering gene transcription and increases synthesis of proteins
- Affects ATP levels
Sodium
- Affects sodium entry and transport
- Increases number of apical sodium channels, NaCl co-transporters and Na+K+ATPase
- Increases activity of the hydrogen sodium exchanger in the apical membrane
- Increases membrane permeability
- Increases sodium pump activity
- Total quantity of sodium is conserved not the actual plasma concentration
- When sodium is reabsorbed water follows it so the volume of the plasma is altered rather than the concentration of sodium changing
- Angiotensin 2 and Aldosterone affect sodium but they also affect ECF volume so only quantity affected not concentration
- ADH and thirst response also work together to dilute the ECF if concentrations of sodium are high so although there is more NaCl the actual concentration is not really changed.
- If there was no secretion of aldosterone a 20kg dog would excrete 15g per 24 hours
- At maximal secretion no significant amount of sodium would be excreted
Potassium
- In cases of increased K+
- Increased Na+ / K+ ATPase pump activity increases the amount of K+ in cells to reduce plasma K+
- Generally not excreted
- However if plasma K+ is still high aldosterone is stimulated
- Causes potassium secretion
- Stimulates Na+ / K+ ATPases in the basolateral membrane of the principal cells
- Increased potassium in the cells
- Potassium leaves via apical leak channels
- Thanks to electro-chemical gradient
- Very tightly regulated system
- Allows large increase in K+ to have a miniscule effect on plasma K+
Hydrogen
- Increases hydrogen secretion by increasing Hydrogen ATPases in the apical membrane of the intercalated cells
- Increases hydrogen secretion by increasing sodium hydrogen exchanger in the apical membrane of the principal cells
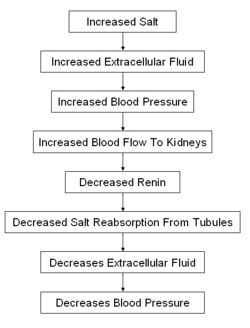
Atrial Natriuretic Peptide
Atrial natriuretic peptide is a peptide hormone which is synthesised and secreted from muscle cells in the atrial walls in response to stretch. The cause of this stretch is usually an increased ECF which results in increased blood volume and pressure distending the atrial walls. To correct this ANP increases renal filtration and inhibits the reabsorption of sodium and therefore water. This increases the volume of water and sodium lost in the urine and therefore decreases the blood volume and pressure.