Difference between revisions of "Regenerative and Non-Regenerative Anaemias"
Fiorecastro (talk | contribs) |
Fiorecastro (talk | contribs) |
||
| Line 47: | Line 47: | ||
===Haemorrhage=== | ===Haemorrhage=== | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Any form of spontaneous haemorrhage with no apparent cause may suggest the presence of an underlying coagulopathy. The most common haemorrhagic presentations are: | Any form of spontaneous haemorrhage with no apparent cause may suggest the presence of an underlying coagulopathy. The most common haemorrhagic presentations are: | ||
*'''Epistaxis''' due to disruption or erosion of blood vessels of the nasal cavity by trauma, neoplasia, fungal infection or a foreign body. | *'''Epistaxis''' due to disruption or erosion of blood vessels of the nasal cavity by trauma, neoplasia, fungal infection or a foreign body. | ||
| Line 73: | Line 55: | ||
===Haemolysis=== | ===Haemolysis=== | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Haemolysis may occur in the following processes: | Haemolysis may occur in the following processes: | ||
*'''Immune-mediated disease''' including [[Immune Mediated Haemolytic Anaemia]] and [[Neonatal Isoerythrolysis]]. | *'''Immune-mediated disease''' including [[Immune Mediated Haemolytic Anaemia]] and [[Neonatal Isoerythrolysis]]. | ||
*'''Infectious agents''' including ''[[Babesia|Babesia spp.]]'' in dogs and cattle, ''[[Feline Infectious Anaemia|Mycoplasma haemofelis]]'' in cats, ''[[Leptospira|Leptospira spp.]]'' in various species and ''[[Clostridium haemolyticum]]'' causing redwater fever in cattle. | *'''Infectious agents''' including ''[[Babesia|Babesia spp.]]'' in dogs and cattle, ''[[Feline Infectious Anaemia|Mycoplasma haemofelis]]'' in cats, ''[[Leptospira|Leptospira spp.]]'' in various species and ''[[Clostridium haemolyticum]]'' causing redwater fever in cattle. | ||
| − | *'''Haemotrophic mycoplasmas | + | *'''[[Features of regenerative and nonregenerative anaemia|Haemotrophic mycoplasmas]]''' |
*'''Inherited defects of red blood cells enzymes''' including pyruvate kinase (which is occur most commonly in West Highland white terriers) and phosphofructokinase (PFK). | *'''Inherited defects of red blood cells enzymes''' including pyruvate kinase (which is occur most commonly in West Highland white terriers) and phosphofructokinase (PFK). | ||
| − | *'''Pyruvate Kinase deficiency | + | *'''[[Features of regenerative and nonregenerative anaemia|Pyruvate Kinase deficiency]]''' |
| − | *'''Phosphofructokinase deficiency''' | + | *'''[[Features of regenerative and nonregenerative anaemia|Phosphofructokinase deficiency]]''' |
*'''Hypophosphataemia''' which occurs in post-parturient cattle (causing post-parturient haemoglobinuria), with refeeding syndrome and when animals with [[Diabetes Mellitus|diabetes mellitus]] are stabilised with insulin. | *'''Hypophosphataemia''' which occurs in post-parturient cattle (causing post-parturient haemoglobinuria), with refeeding syndrome and when animals with [[Diabetes Mellitus|diabetes mellitus]] are stabilised with insulin. | ||
*Exposure to '''toxins''' including rape and kale (which contain SMCO radicals) in cattle, onions and garlic in dogs and paracetamol in cats. | *Exposure to '''toxins''' including rape and kale (which contain SMCO radicals) in cattle, onions and garlic in dogs and paracetamol in cats. | ||
*'''Microangiopathic anaemia''' which occurs when red blood cells are forced through small meshworks of fibrin as with [[Haemangiosarcoma|haemangiosarcomas]], [[Disseminated Intravascular Coagulation|disseminated intravascular coagulation]] (DIC) or bacterial endocarditis. | *'''Microangiopathic anaemia''' which occurs when red blood cells are forced through small meshworks of fibrin as with [[Haemangiosarcoma|haemangiosarcomas]], [[Disseminated Intravascular Coagulation|disseminated intravascular coagulation]] (DIC) or bacterial endocarditis. | ||
| − | |||
Haemolysis usually results in a more strongly regenerative response than haemorrhage and can be differentiated by plasma protein concentrations; these will fall with haemorrhage, but not with haemolysis. | Haemolysis usually results in a more strongly regenerative response than haemorrhage and can be differentiated by plasma protein concentrations; these will fall with haemorrhage, but not with haemolysis. | ||
==Non-regenerative Anaemia== | ==Non-regenerative Anaemia== | ||
The failure to regenerate indicates that there is a failure to produce red blood cells in the bone marrow. Erythrocytes are produced from stem cells in the bone marrow and they then undergo sequential stages of maturation before and after they are released into the circulation. | The failure to regenerate indicates that there is a failure to produce red blood cells in the bone marrow. Erythrocytes are produced from stem cells in the bone marrow and they then undergo sequential stages of maturation before and after they are released into the circulation. | ||
| − | + | === [[Features of regenerative and nonregenerative anaemia|Primary Anaemia: Failure of the bone marrow stem cells to produce erythroid cells]] === | |
| − | |||
| − | |||
| − | === Primary Anaemia: Failure of the bone marrow stem cells to produce erythroid cells === | ||
This occurs in the following conditions: | This occurs in the following conditions: | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
'''[[Immune Mediated Haemolytic Anaemia|Pure red cell aplasia]]''' | '''[[Immune Mediated Haemolytic Anaemia|Pure red cell aplasia]]''' | ||
| Line 125: | Line 77: | ||
'''Myelodysplasia''' | '''Myelodysplasia''' | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
=== Failure of erythrocyte maturation === | === Failure of erythrocyte maturation === | ||
This can occur with: | This can occur with: | ||
| Line 156: | Line 83: | ||
== References == | == References == | ||
| − | + | {{Learning | |
|flashcards = [[Feline Medicine Q&A 08]] |Vetstream = [https://www.vetstream.com/equis/Content/Disease/dis01203.asp Anemia] | |flashcards = [[Feline Medicine Q&A 08]] |Vetstream = [https://www.vetstream.com/equis/Content/Disease/dis01203.asp Anemia] | ||
}} | }} | ||
{{review}} | {{review}} | ||
| − | |||
[[Category:Anaemia|2]] | [[Category:Anaemia|2]] | ||
[[Category:Lymphoreticular and Haematopoietic Diseases - Dog]][[Category:Lymphoreticular and Haematopoietic Diseases - Cat]][[Category:Lymphoreticular and Haematopoietic Diseases - Horse]][[Category:Lymphoreticular and Haematopoietic Diseases - Cattle]][[Category:Donkey]][[Category:Lymphoreticular and Haematopoietic Diseases - Sheep]][[Category:Lymphoreticular and Haematopoietic Diseases - Pig]] | [[Category:Lymphoreticular and Haematopoietic Diseases - Dog]][[Category:Lymphoreticular and Haematopoietic Diseases - Cat]][[Category:Lymphoreticular and Haematopoietic Diseases - Horse]][[Category:Lymphoreticular and Haematopoietic Diseases - Cattle]][[Category:Donkey]][[Category:Lymphoreticular and Haematopoietic Diseases - Sheep]][[Category:Lymphoreticular and Haematopoietic Diseases - Pig]] | ||
Latest revision as of 16:55, 11 April 2022
Introduction
Anaemia refers to a reduction in packed cell volume (PCV), haemoglobin concentration or the level of total red blood cells. In the clinical approach to the anaemic patient, the initial step is to determine whether the anaemia is regenerative or non-regenerative. Regeneration refers to the production of new erythrocytes from the bone marrow and their subsequent release into the circulation. In dogs, there is a lag period of 48-72 hours before immature red blood cells (reticulocytes and nucleated red blood cells ) begin to appear in the circulation and the extent of the regenerative response is usually in proportion to the severity of the anaemic insult.
Causes of Anaemia
The major causes of anaemia are:
- Immune-mediated disease including immune-mediated haemolytic anaemia, a disease caused by an autoimmune response directed against endogenous erythrocytes, and neonatal isoerythrolysis, the result of a maternal immune response directed against foetal antigens inherited from the sire.
- Haemorrhage
- Haemolysis
- Anaemia of Chronic Disease
- Infectious Diseases, notably:
- Equine Infectious Anaemia caused by EIA virus.
- Canine and feline infectious anemia caused by Mycoplasma haemocanis and Mycoplasma haemofelis respectively. Candidata M. haemominutum and M. turicensis may also cause anaemia in cats.
- Leptospira spp. may cause anaemia, usually when an animal is exposed to a non-host-adapted serovar.
- Babesia spp. may cause anaemia in dogs and cattle.
- Hepatozoon spp. in dogs and pigs.
- Clostridium haemolyticum causing Redwater Fever in cattle.
Regenerative or Non Regenerative?
The following features may be used to determine whether anaemia is regenerative or non-regenerative:
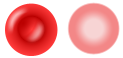
| Feature | Regenerative | Non-regenerative | Image |
| Mean Corpuscular Volume (MCV) | Increased as reticulocytes are larger than mature erythrocytes | Normal | |
| Mean Corpuscular Haemoglobin Concentration (MCHC) | Decreased as reticulocytes are larger cells and less packed with haemoglobin (as the marrow is trying to produce cells at a faster rate it means they are not as well formed) and they also contain the remnant of the ribosomal RNA that is lost with progressive development of the cell | Normal | |
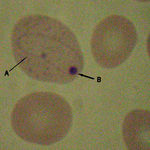
| Blood Smear | Howell-Jolly bodies may be present as small basophilic spots within red blood cells. These represent the remnant of the endoplasmic reticulum of the erythrocyte. Large polychromatic red blood cells may be evident when the smear is stained with a Romanowsky stain. These cells probably represent reticulocytes but this cannot be confirmed unless a smear is also stained with a supra-vital stain such as new methylene blue. This latter procedure can be used to estimate the degree of reticulocytosis and to determine if this is appropriate to the severity of the anaemia. |
The red blood cells are usually normochromic and normocytic but poikilocytosis may be apparent in cases of maturation defect anaemia. |
Regenerative Anaemia
The major causes of regenerative anaemia are haemorrhage and haemolysis.
Haemorrhage
Any form of spontaneous haemorrhage with no apparent cause may suggest the presence of an underlying coagulopathy. The most common haemorrhagic presentations are:
- Epistaxis due to disruption or erosion of blood vessels of the nasal cavity by trauma, neoplasia, fungal infection or a foreign body.
- Haematuria which may arise due to haemorrhage from any part of the urinary tract, especially the kidney (due to trauma, neoplasia or idiopathic haematuria) and bladder (due to trauma, cystitis, urolithiasis and neoplasia).
- Melaena, haematochezia or haematemesis due to gastro-intestinal haemorrhage. Meleana refers to the production of black tarry faeces with digested blood whereas haematochezia refers to the production of fresh blood with the faeces. Classically, haematemesis is described as resembling 'coffee grounds' as blood is denatured by a low gastric pH but, as the gastric pH of the dog may vary widely between 2 and 6, vomited blood may also appear as fresh red blood.
- Haemoptysis refers to the production of blood from the respiratory tract. It may occur with severe forms of pneumonia and with pulmonary haemorrhage.
- Haemoabdomen, haemothorax and haemopericardium are all forms of haemorrhagic effusion that occur in body cavities.
Haemolysis
Haemolysis may occur in the following processes:
- Immune-mediated disease including Immune Mediated Haemolytic Anaemia and Neonatal Isoerythrolysis.
- Infectious agents including Babesia spp. in dogs and cattle, Mycoplasma haemofelis in cats, Leptospira spp. in various species and Clostridium haemolyticum causing redwater fever in cattle.
- Haemotrophic mycoplasmas
- Inherited defects of red blood cells enzymes including pyruvate kinase (which is occur most commonly in West Highland white terriers) and phosphofructokinase (PFK).
- Pyruvate Kinase deficiency
- Phosphofructokinase deficiency
- Hypophosphataemia which occurs in post-parturient cattle (causing post-parturient haemoglobinuria), with refeeding syndrome and when animals with diabetes mellitus are stabilised with insulin.
- Exposure to toxins including rape and kale (which contain SMCO radicals) in cattle, onions and garlic in dogs and paracetamol in cats.
- Microangiopathic anaemia which occurs when red blood cells are forced through small meshworks of fibrin as with haemangiosarcomas, disseminated intravascular coagulation (DIC) or bacterial endocarditis.
Haemolysis usually results in a more strongly regenerative response than haemorrhage and can be differentiated by plasma protein concentrations; these will fall with haemorrhage, but not with haemolysis.
Non-regenerative Anaemia
The failure to regenerate indicates that there is a failure to produce red blood cells in the bone marrow. Erythrocytes are produced from stem cells in the bone marrow and they then undergo sequential stages of maturation before and after they are released into the circulation.
Primary Anaemia: Failure of the bone marrow stem cells to produce erythroid cells
This occurs in the following conditions:
Myelophthisis
Myelodysplasia
Failure of erythrocyte maturation
This can occur with:
- Iron deficiency
- Vitamin B12/folate deficiency
References
| Regenerative and Non-Regenerative Anaemias Learning Resources | |
|---|---|
To reach the Vetstream content, please select |
Canis, Felis, Lapis or Equis |
 Test your knowledge using flashcard type questions |
Feline Medicine Q&A 08 |
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
- Anaemia
- Lymphoreticular and Haematopoietic Diseases - Dog
- Lymphoreticular and Haematopoietic Diseases - Cat
- Lymphoreticular and Haematopoietic Diseases - Horse
- Lymphoreticular and Haematopoietic Diseases - Cattle
- Donkey
- Lymphoreticular and Haematopoietic Diseases - Sheep
- Lymphoreticular and Haematopoietic Diseases - Pig