Difference between revisions of "Reabsorption and Secretion Along the Distal Tubule and Collecting Duct - Anatomy & Physiology"
| (2 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
| − | |||
[[Image:disttubexch.jpg|right|thumb|250px|<small><center>Exchange in the Principal Cells of the Distal Tubule</center></small>]] | [[Image:disttubexch.jpg|right|thumb|250px|<small><center>Exchange in the Principal Cells of the Distal Tubule</center></small>]] | ||
==Distal Tubule== | ==Distal Tubule== | ||
| Line 107: | Line 106: | ||
Use the [[Reabsorption and Secretion Along the Distal Tubule and Collecting Duct - Renal Flash Cards - Anatomy & Physiology|flash card revision resource]] for this section to test yourself. | Use the [[Reabsorption and Secretion Along the Distal Tubule and Collecting Duct - Renal Flash Cards - Anatomy & Physiology|flash card revision resource]] for this section to test yourself. | ||
| − | + | [[Category:Urinary System]] | |
| − | [[Category: | ||
| − | |||
Revision as of 18:07, 9 December 2010
Distal Tubule
- Important site of regulation of ions and water
- Less emphasis on bulk transport compared with proximal tubule
- More emphasis on fine management
- It is able to do this as it has high resistance epithelia. Allowing it to maintain substantial gradients across it
- Very important for the homeostasis of:
- Sodium
- Potassium
- Acid / Base
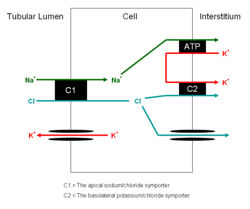
- There are two cell types present each with different functions. They are similar to the cells of the collecting ducts
- Principal cells
- Absorb sodium
- Excrete potassium and hydrogen
- Site of action of Aldosterone
- Intercalated cells
- ATP driven proton secretion
- Principal cells
Juxtaglomerular Apparatus
- The terminal portion of the straight distal tubule contacts the afferent and efferent vessels supplying its own glomerulus
- These vessels are said to embrace the distal tubule
- Here a special apparatus called the Juxtaglomerular Apparatus has 3 different structures:
- The tubular epithelial cells of the distal tubule which are in contact with the arterioles supplying the glomerulus of that nephron are called the macula densa. They play a vital role in the regulation of the GFR.
- The Juxtaglomerular Cells are smooth muscle cells which adjoin the macula densa in the capillary wall.
- The Extraglomerular Mesangium has an unclear function
Juxtaglomerular Cells
- Smooth muscle cells
- Synthesise renin
- From the zymogen prerenin
- Described as intra-renal baroreceptors
- Respond to stretch
- The secretion of renin from these cells depends on the stretch
- If stretch decreases - blood pressure has decreased - renin secretion increases
- Also respond to the sympathetic nervous system
- Increases renin output
Developmental
Develops from metanephric tubule
Collecting Duct
This part of the nephron has two cell types
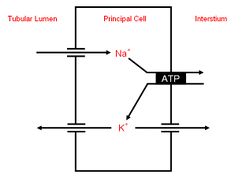
Principal Cells
- ADH acts on these cells inserting aquaporins into the cell membranes
- It is released from the posterior pituitary gland
Intercalated cells
- The intercalated cells can be subdivided further to:
- Alpha intercalated cells secrete H+
- Beta intercalated cells secrete HCO3-
Developmental
- Develops from branched ureteric bud
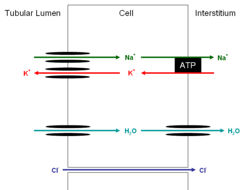
The Concentrating Mechanism, Aquaporins and ADH
Water is drawn from the lumen of the tubule by the increasing hypertonicity of the surrounding tissue as the duct makes its way deeper into the medulla. However this reabsorption is only possible thanks to ADH inserting aquaporins into the apical membrane. These channels are always present on the basolateral membrane of the epithelial cells but not on the apical membrane. The reabsorption would not be possible if the urine did not go back up the thick ascending limb of the loop of henle, where its concentration was decreased by the reabsorption of salt, but instead went straight into the collecting ducts. Although this would mean very concentrated urine it would result in massive salt losses. Thus the collecting duct allows for very concentrated urine with minimal salt loss. It also allows the concentration of the urine to vary from dilute to concentrated under the control of the hypothalamus and ADH concentrations.
Ions and Compounds
The following ions and compounds are reabsorbed or secreted partly or completely in the distal tubules and collecting ducts:
Sodium
The remaining 10% is reabsorbed in the distal tubule. Although the transport capacity here is minimal the high resistance epithelia mean that very little back flow into the lumen occurs allowing the remaining sodium to be easily reabsorbed. Some of this reabsorption takes place using a sodium chloride co-transporter. The reabsorption of sodium from here and the collecting ducts is under hormonal control allowing "fine tuning" to occur.
See:
Potassium
Distal Tubule
- Here the potassium and chloride symporter actually excretes the two ions into the lumen of the tubule
- Na+ / K+ ATPases in the basolateral membrane move potassium into epithelial cells from the intercellular spaces in order to remove sodium. The potassium then diffuses into the lumen via channels
- The ability to secrete potassium here is vital in animals with high potassium diets such as herbivores where excreting only the amount filtered would not be suffice
Principal Cells of Collecting Duct
- Potassium transported into lumen
- Is both absorbed and secreted via paracellular route
- Na+ / K+ ATPases in the basolateral membrane move potassium into epithelial cells from the intercellular spaces in order to remove sodium and keep potassium concentrations high.
- Aldosterone works here
Intercalated Cells of Collecting Duct
- Potassium is absorbed here in exchange for hydrogen
H+ and HCO3-
- H+ ions are secreted in the cortical and medullary collecting tubules
- This is an active secretion using a H+ ATPase
- Also a H+/K+ ATPase antiporter
- The main function of this is maintaining potassium
- HCO3- is reabsorbed here
Urea
In the lower portion of the collecting duct urea freely diffuses across the epithelia. The permeability is also increased with ADH. This adds to the hypertonicity of the medulla and increases water reabsorption.
Urea and Water Reabsorption
Water follows urea as it is reabsorbed from the collecting duct. This actually increases the concentration of urea in the tubular fluid despite some of it being reabsorbed. This means that urea concentration only drops moderately when the urine concentration falls due to increased reabsorption of water.
Calcium
The regulation of how much calcium is reabsorbed occurs in the ascending limb of the loop of henle, the distal tubule and collecting ducts. Parathyroid hormone stimulates reabsorption. It is normal for a 1-2% excretion of calcium to occur
Revision
Use the flash card revision resource for this section to test yourself.