Difference between revisions of "Lungs Circulatory - Pathology"
Jump to navigation
Jump to search
(Redirected page to Category:Lungs - Circulatory Pathology) |
|||
| (14 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
| − | # | + | {{review}} |
| + | |||
| + | {{toplink | ||
| + | |backcolour = D1EEEE | ||
| + | |linkpage =Cardiorespiratory System - Pathology | ||
| + | |linktext =Cardiorespiratory System | ||
| + | |maplink = Cardiorespiratory System (Content Map) - Pathology | ||
| + | |pagetype =Pathology | ||
| + | |sublink1=Lungs Degenerative - Pathology | ||
| + | |subtext1=LUNGS DEGENERATIVE | ||
| + | }} | ||
| + | <br> | ||
| + | ==Hyperaemia== | ||
| + | |||
| + | *Localised of diffuse as part of acute inflammation | ||
| + | |||
| + | |||
| + | ==Congestion== | ||
| + | |||
| + | *Decreased outflow of venous blood | ||
| + | *Most commonly caused by left-sided or bilateral cardiac failure | ||
| + | **Stagnant blood in pulmonary vessels -> red blood cells move into alveoli and are phagocytosed -> [[Pigmentation and Calcification - Pathology#Haemosiderin|haemosiderin in macrophages]] (heart failure cells) | ||
| + | *One-sided in post-mortem hypostatic congestion | ||
| + | *Acute pulmonary congestion is seen after barbiturate euthanasia | ||
| + | *Leads to pulmonary oedema (below) | ||
| + | |||
| + | |||
| + | ==Pulmonary oedema== | ||
| + | |||
| + | *Excessive fluid in the lung | ||
| + | *Normally, mechanisms are in place to protect the lung from the entry of circulatory fluid into alveolar spaces (See [[Respiratory System General Introduction - Pathology#Lungs|functional anatomy]]) | ||
| + | *Occurs when exudation of fluid from vessels into interstitium or alveoli exceeds the rate of alveolar or lymph removal | ||
| + | *Generally a sequel to or part of congestion or inflammatory process | ||
| + | *Generally begins as '''interstitial oedema''' characterised by expansion of perivascular and peribronchial and peribronchiolar fascia and distension of interstitial lymphatics | ||
| + | *Only when this interstitial compartment is overwhelmed does fluid flood the airspaces causing '''alveolar oedema''' | ||
| + | *Gross pathology: | ||
| + | **Heavy wet lungs which do not properly collapse | ||
| + | **Subpleural and interstitial tissue distended with fluid | ||
| + | **Foamy fluid oozing from the cut surface and airways | ||
| + | *Micro pathology: | ||
| + | **Pinkish fluid in alveoli and airways in association with air bubbles, and also in dilated lymphatics of the interstitium | ||
| + | **Colour of the fluid enhanced in cases where the endothelium is damaged - more protein present | ||
| + | **In slowly developing cases, macrophages contain haemosiderin | ||
| + | *The major causes of pulmonary oedema are: | ||
| + | **Increased capillary or type I epithelial permeability caused by | ||
| + | ***Systemic toxins | ||
| + | ***Shock | ||
| + | ***Inhaled caustic gases | ||
| + | **Increased capillary hydrostatic pressure ('''cardiogenic oedema''' - left-sided or biventricular heart failure, sympathetic stimulation in acute brain damage) | ||
| + | **Decreased plasma oncotic pressure (hypoalbuminaemia) | ||
| + | **Overloading in excessive fluid therapy | ||
| + | **As part of inflammatory process | ||
| + | |||
| + | |||
| + | ==Pulmonary haemorrhage== | ||
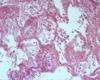
| + | [[Image:Pulmonary haemorrhage.jpg|right|thumb|100px|<small><center>Pulmonary haemorrhage (Image sourced from Bristol Biomed Image Archive with permission)</center></small>]] | ||
| + | *Potential sequel of septicaemias, bleeding disorders, disseminated intravascular coagulation, and severe congestion, severe acute inflammation, "back splashing" at slaughter (aspiration of blood) | ||
| + | *[[Exercise Induced Pulmonary Haemorrhage|'''Exercise-induced pulmonary hemorrhage''' (EIPH)]] | ||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | ==Embolism, thrombosis and infarction== | ||
| + | [[Image:Pulmonary infarction.jpg|right|thumb|100px|<small><center>Pulmonary infarction (Image sourced from Bristol Biomed Image Archive with permission)</center></small>]] | ||
| + | [[Image:Segmental pulmonary infarction.jpg|right|thumb|100px|<small><center>Segmental pulmonary infarction (Image sourced from Bristol Biomed Image Archive with permission)</center></small>]] | ||
| + | |||
| + | *Lungs are strategically situated to catch emboli carried in venous blood | ||
| + | *Because the lung is supplied by both pulmonary and bronchial arteries and has extensive collateral channels, infarction usually does not follow embolism or thrombosis unless pulmonary circulation is already compromised | ||
| + | *In animals, greatest risk comes from: | ||
| + | **'''Tumor emboli''' | ||
| + | ***From e.g.: osteosarcoma and haemangiosarcoma in dogs, uterine carcinoma in cattle | ||
| + | **'''Septic emboli''' | ||
| + | ***From bacterial [[Endocarditis|endocarditis]], jugular thrombophlebitis, [[Hepatic Abscessation|hepatic abscesses]] etc. | ||
| + | ***May cause unexpected death if in large numbers | ||
| + | ***May develop [[Lungs Inflammatory - Pathology|suppurative pneumonia]] -> [[Lungs Inflammatory - Pathology#Pulmonary abscesses|pulmonary abscesses]], [[Arteritis|arteritis]], [[Thrombosis|thrombosis]] | ||
| + | *Pulmonary infarcts usually occur when there is embolisation or thrombosis during general circulatory collapse or passive congestion of heart failure | ||
| + | *Pulmonary thromboembolism is a sequel to in cattle to large emboli from liver abscesses close to the vena cava | ||
| + | **Death may ocur due to massive haemorrhaging into lung tissue | ||
| + | *Parasites (e.g. [[Respiratory Parasitic Infections - Pathology#Dirofilaria immitis|''Dirofilaria immitis'']], [[Respiratory Parasitic Infections - Pathology#Angiostrongylus vasorum|''Angiostrongylus vasorum'']]) may be responsible | ||
| + | *Long-term intravenous catheterisation may cuse thrombi pieces breaking off and lodging in pulmonary vessels | ||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
| + | ==Pulmonary hypertension== | ||
| + | |||
| + | *Caused by '''left-to-right vascular shunts''' or increased resistance of the pulmonary vascular system | ||
| + | |||
| + | *In animals, it is most commonly a sequel of '''widespread fibrosis in the lung''' or [[Bronchi and Bronchioles Inflammatory - Pathology#Chronic bronchitis|chronic bronchitis or bronchiolitis]] which stimulates hypertrophy in the walls of small arteries | ||
| + | *Severe prolonged pulmonary hypertension leads to [[Cor Pulmonale|'''cor pulmonale''']], right-sided heart failure secondary to primary lung disease | ||
Revision as of 15:18, 1 July 2010
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
|
|
Hyperaemia
- Localised of diffuse as part of acute inflammation
Congestion
- Decreased outflow of venous blood
- Most commonly caused by left-sided or bilateral cardiac failure
- Stagnant blood in pulmonary vessels -> red blood cells move into alveoli and are phagocytosed -> haemosiderin in macrophages (heart failure cells)
- One-sided in post-mortem hypostatic congestion
- Acute pulmonary congestion is seen after barbiturate euthanasia
- Leads to pulmonary oedema (below)
Pulmonary oedema
- Excessive fluid in the lung
- Normally, mechanisms are in place to protect the lung from the entry of circulatory fluid into alveolar spaces (See functional anatomy)
- Occurs when exudation of fluid from vessels into interstitium or alveoli exceeds the rate of alveolar or lymph removal
- Generally a sequel to or part of congestion or inflammatory process
- Generally begins as interstitial oedema characterised by expansion of perivascular and peribronchial and peribronchiolar fascia and distension of interstitial lymphatics
- Only when this interstitial compartment is overwhelmed does fluid flood the airspaces causing alveolar oedema
- Gross pathology:
- Heavy wet lungs which do not properly collapse
- Subpleural and interstitial tissue distended with fluid
- Foamy fluid oozing from the cut surface and airways
- Micro pathology:
- Pinkish fluid in alveoli and airways in association with air bubbles, and also in dilated lymphatics of the interstitium
- Colour of the fluid enhanced in cases where the endothelium is damaged - more protein present
- In slowly developing cases, macrophages contain haemosiderin
- The major causes of pulmonary oedema are:
- Increased capillary or type I epithelial permeability caused by
- Systemic toxins
- Shock
- Inhaled caustic gases
- Increased capillary hydrostatic pressure (cardiogenic oedema - left-sided or biventricular heart failure, sympathetic stimulation in acute brain damage)
- Decreased plasma oncotic pressure (hypoalbuminaemia)
- Overloading in excessive fluid therapy
- As part of inflammatory process
- Increased capillary or type I epithelial permeability caused by
Pulmonary haemorrhage
- Potential sequel of septicaemias, bleeding disorders, disseminated intravascular coagulation, and severe congestion, severe acute inflammation, "back splashing" at slaughter (aspiration of blood)
- Exercise-induced pulmonary hemorrhage (EIPH)
Embolism, thrombosis and infarction
- Lungs are strategically situated to catch emboli carried in venous blood
- Because the lung is supplied by both pulmonary and bronchial arteries and has extensive collateral channels, infarction usually does not follow embolism or thrombosis unless pulmonary circulation is already compromised
- In animals, greatest risk comes from:
- Tumor emboli
- From e.g.: osteosarcoma and haemangiosarcoma in dogs, uterine carcinoma in cattle
- Septic emboli
- From bacterial endocarditis, jugular thrombophlebitis, hepatic abscesses etc.
- May cause unexpected death if in large numbers
- May develop suppurative pneumonia -> pulmonary abscesses, arteritis, thrombosis
- Tumor emboli
- Pulmonary infarcts usually occur when there is embolisation or thrombosis during general circulatory collapse or passive congestion of heart failure
- Pulmonary thromboembolism is a sequel to in cattle to large emboli from liver abscesses close to the vena cava
- Death may ocur due to massive haemorrhaging into lung tissue
- Parasites (e.g. Dirofilaria immitis, Angiostrongylus vasorum) may be responsible
- Long-term intravenous catheterisation may cuse thrombi pieces breaking off and lodging in pulmonary vessels
Pulmonary hypertension
- Caused by left-to-right vascular shunts or increased resistance of the pulmonary vascular system
- In animals, it is most commonly a sequel of widespread fibrosis in the lung or chronic bronchitis or bronchiolitis which stimulates hypertrophy in the walls of small arteries
- Severe prolonged pulmonary hypertension leads to cor pulmonale, right-sided heart failure secondary to primary lung disease