Difference between revisions of "Renin Angiotensin Aldosterone System"
Fiorecastro (talk | contribs) |
|||
| (28 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
| − | |||
Also known as: '''''RAAS''''' | Also known as: '''''RAAS''''' | ||
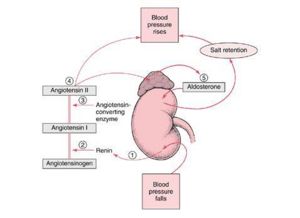
[[Image:RAS.jpg|right|thumb|300px|<small><center> Schematic of the RAAS ©RVC 2008</center></small>]] | [[Image:RAS.jpg|right|thumb|300px|<small><center> Schematic of the RAAS ©RVC 2008</center></small>]] | ||
| − | |||
==Introduction== | ==Introduction== | ||
| − | + | The RAAS is activated whenever blood flow through the kidneys is reduced and when there are sodium losses in conditions such as diarrhoes, vomiting or excessive sweating. These losses reduce extracellular fluid volume and this in turn reduces arterial blood pressure, which triggers the RAAS system through several different mechanisms. | |
| − | The RAAS is activated whenever blood flow through the kidneys is reduced | ||
==RAAS Activation== | ==RAAS Activation== | ||
| − | |||
[[Image:raasflowdefap.jpg|right|thumb|275px|<small><center>The Mechanism Behind the RAAS </center></small>]] | [[Image:raasflowdefap.jpg|right|thumb|275px|<small><center>The Mechanism Behind the RAAS </center></small>]] | ||
[[Image:raasflowsumap.jpg|right|thumb|250px|<small><center>Summary of the purpose of the RAAS</center></small>]] | [[Image:raasflowsumap.jpg|right|thumb|250px|<small><center>Summary of the purpose of the RAAS</center></small>]] | ||
| + | In the event of blood pressure dropping [[Kidney Endocrine Function - Anatomy & Physiology#Renin|Renin]] is secreted due to the decreased stretch of the [[Reabsorption and Secretion Along the Distal Tubule and Collecting Duct - Anatomy & Physiology#Juxtaglomerular Cells|'''juxtaglomerular cells''']] and an increased sympathetic stimulation triggered by the decreased activation of arterial baroreceptors. This enzyme cleaves the alpha glycoprotein '''Angiotensinogen''' which is released from the [[Liver - Anatomy & Physiology|liver]]. This produces '''Angiotensin 1''' which is further converted by [[Angiotensin Converting Enzyme(ACE) - Renal Anatomy & Physiology|'''Angiotensin Converting Enzyme''' (ACE)]] to '''Angiotensin II''' mainly in the lungs but to a much lesser extent locally in the kidneys. Angiotensin 2 then works to restore blood pressure by inducing constriction of arterioles, which increases vascular resistance, and constricting veins which reduces vascular volume. In this section we cover its effects on and through the kidneys. | ||
| − | + | ==Effects of Angiotensin 2 on Blood Pressure== | |
| − | + | '''Angiotensin II''' acts on '''AT1 receptors''' to stimulate the release of '''[[Aldosterone|aldosterone]]''' from the [[Adrenal Glands - Anatomy & Physiology#Adrenal Glands|zona glomerulosa]] of the adrenal glands. This mineralocorticoid increases the reabsorption of sodium and therefore water and chloride from the distal tubule of the kidney, thus helping to increase blood pressure and volume. It also stimulates the thirst center and increases the secretion of [[Pituitary Gland - Anatomy & Physiology #Posterior Pituitary Gland | ADH]] to help increase blood volume. The RAAS allows pressure to return to 50% of baseline within 15 minutes of a significant haemorrhage occuring. | |
| − | ==Effects of Angiotensin | ||
| − | |||
| − | '''Angiotensin II''' acts on '''AT1 receptors''' to stimulate the release of '''[[Aldosterone|aldosterone]]''' from the [[Adrenal Glands - Anatomy & Physiology#Adrenal Glands|zona glomerulosa]] of the adrenal glands. This mineralocorticoid increases | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | ==Effects of Angiotensin 2 on GFR== | |
| + | If blood pressure drops then [[The Formation of the Filtrate by the Glomerular Apparatus- Anatomy & Physiology#Glomerular Filtration Rate|GFR]] also drops due to a reduced blood flow through the kidneys. Therefore it is important to prevent this. If contraction of the efferent arteriole occurs then the pressure difference between the afferent and efferent arterioles increases creating a greater filtration pressure. This effect is mediated by Angiotensin 2 and means that when blood pressure falls there is minimum alteration of GFR. Blood flow which is already reduced due to the reduced pressure will then be further reduced by the increase in resistance. This increased renal resistance to blood flow and the maintained GFR has many advantageous effects. | ||
| − | Angiotensin | + | ===Advantages of Constriction of the Efferent Arteriole=== |
| + | * If you increase the resistance in the kidneys you contribute to increasing total peripheral resistance. This helps to return blood pressure towards normal. (Angiotensin 2 also has vasoconstrictive effects in other organs.) | ||
| + | * The kidneys can tolerate the reduced perfusion allowing blood to be prioritised to organs which need it like the brain and heart. | ||
| + | * The constriction of the efferent arterioles also reduces hydrostatic pressure in the [[The Formation of the Filtrate by the Glomerular Apparatus- Anatomy & Physiology#Pressure in the Peritubular Capillaries| Peritubular Capillaries]] this increases reabsorption of water and salt thus helping to restore the ECF and thus helps to normalise blood pressure. | ||
| + | * The amount of waste excreted is variable with GFR. Thanks to the normalised GFR the excretion of waste products such as urea is maintained. | ||
| − | + | ==Effects of Angiotensin 2 On Sodium== | |
| − | + | * Induces insertion of Na<sup>+</sup> channels into renal tubules via stimulation of AT<sub>1</sub> receptors | |
| − | + | * Proximal tubule: | |
| + | ** Apical - Na<sup>+</sup>/H<sup>+</sup> exchangers | ||
| + | ** Basolateral Na<sup>+</sup>(HCO<sub>3</sub><sup>-</sup>)<sub>3</sub> and Na<sup>+</sup>K<sup>+</sup>ATPase | ||
| + | * Thick ascending limb | ||
| + | ** Apical Na<sup>+</sup>/H<sup>+</sup> exchangers and Na<sup>+</sup>K<sup>+</sup>2Cl<sup>-</sup> symporter | ||
| + | * Collecting Duct | ||
| + | ** Epithelial Na<sup>+</sup> channel | ||
| + | * Also stimulates '''Aldosterone''' | ||
| − | == | + | ==Revision== |
| − | + | Use the [[Important Hormonal Regulators of the Kidney - Renal Flash Cards - Anatomy & Physiology|flash card revision resource]] for this section to test yourself. | |
| − | [[Category: | + | [[Category:Urinary System - Anatomy & Physiology]][[Category:Endocrine System - Anatomy & Physiology]] |
| + | [[Category:Image Review]] | ||
[[Category:Blood Pressure]] | [[Category:Blood Pressure]] | ||
| − | |||
| − | |||
Revision as of 18:27, 27 October 2010
Also known as: RAAS
Introduction
The RAAS is activated whenever blood flow through the kidneys is reduced and when there are sodium losses in conditions such as diarrhoes, vomiting or excessive sweating. These losses reduce extracellular fluid volume and this in turn reduces arterial blood pressure, which triggers the RAAS system through several different mechanisms.
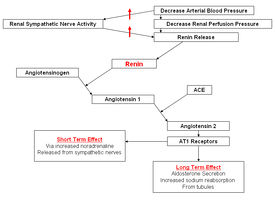
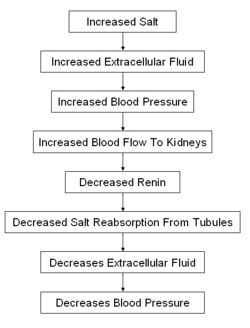
RAAS Activation
In the event of blood pressure dropping Renin is secreted due to the decreased stretch of the juxtaglomerular cells and an increased sympathetic stimulation triggered by the decreased activation of arterial baroreceptors. This enzyme cleaves the alpha glycoprotein Angiotensinogen which is released from the liver. This produces Angiotensin 1 which is further converted by Angiotensin Converting Enzyme (ACE) to Angiotensin II mainly in the lungs but to a much lesser extent locally in the kidneys. Angiotensin 2 then works to restore blood pressure by inducing constriction of arterioles, which increases vascular resistance, and constricting veins which reduces vascular volume. In this section we cover its effects on and through the kidneys.
Effects of Angiotensin 2 on Blood Pressure
Angiotensin II acts on AT1 receptors to stimulate the release of aldosterone from the zona glomerulosa of the adrenal glands. This mineralocorticoid increases the reabsorption of sodium and therefore water and chloride from the distal tubule of the kidney, thus helping to increase blood pressure and volume. It also stimulates the thirst center and increases the secretion of ADH to help increase blood volume. The RAAS allows pressure to return to 50% of baseline within 15 minutes of a significant haemorrhage occuring.
Effects of Angiotensin 2 on GFR
If blood pressure drops then GFR also drops due to a reduced blood flow through the kidneys. Therefore it is important to prevent this. If contraction of the efferent arteriole occurs then the pressure difference between the afferent and efferent arterioles increases creating a greater filtration pressure. This effect is mediated by Angiotensin 2 and means that when blood pressure falls there is minimum alteration of GFR. Blood flow which is already reduced due to the reduced pressure will then be further reduced by the increase in resistance. This increased renal resistance to blood flow and the maintained GFR has many advantageous effects.
Advantages of Constriction of the Efferent Arteriole
- If you increase the resistance in the kidneys you contribute to increasing total peripheral resistance. This helps to return blood pressure towards normal. (Angiotensin 2 also has vasoconstrictive effects in other organs.)
- The kidneys can tolerate the reduced perfusion allowing blood to be prioritised to organs which need it like the brain and heart.
- The constriction of the efferent arterioles also reduces hydrostatic pressure in the Peritubular Capillaries this increases reabsorption of water and salt thus helping to restore the ECF and thus helps to normalise blood pressure.
- The amount of waste excreted is variable with GFR. Thanks to the normalised GFR the excretion of waste products such as urea is maintained.
Effects of Angiotensin 2 On Sodium
- Induces insertion of Na+ channels into renal tubules via stimulation of AT1 receptors
- Proximal tubule:
- Apical - Na+/H+ exchangers
- Basolateral Na+(HCO3-)3 and Na+K+ATPase
- Thick ascending limb
- Apical Na+/H+ exchangers and Na+K+2Cl- symporter
- Collecting Duct
- Epithelial Na+ channel
- Also stimulates Aldosterone
Revision
Use the flash card revision resource for this section to test yourself.