Difference between revisions of "T cells"
Rjfrancisrvc (talk | contribs) |
|||
| (12 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
| + | {{OpenPagesTop}} | ||
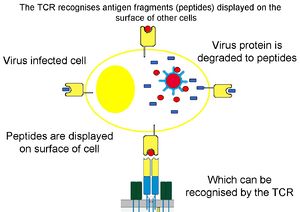
[[Image:TCR2.jpg|thumb|right|300px|T-cell receptor binds antigen fragments presented by MHC on the cell surface - B. Catchpole, RVC 2008]] | [[Image:TCR2.jpg|thumb|right|300px|T-cell receptor binds antigen fragments presented by MHC on the cell surface - B. Catchpole, RVC 2008]] | ||
| − | Also known as '''T lymphocytes | + | Also known as '''T lymphocytes'''<br /> |
| + | |||
| + | ''See also: [[T cell differentiation|T cell differentiation]]'' | ||
==Introduction== | ==Introduction== | ||
<p>T cells are so named as they differentiate in the [[Thymus - Anatomy & Physiology|thymus]]. They are long lived and are involved in '''cell mediated immunity'''. They represent 60-80% of the circulating lymphocytes and all express the markers CD2, CD3 and CD7 as well as having T cell receptors (TCR). Each T cell has 30,000 TCRs each of which is identical and recognises antigens and major histocompatability complex (MHC) II.</p><p>Functionally they are divided into three subsets that are distinguished by the presence or absence of CD4 or CD8 markers. CD4 and CD8 cells have α/β antigen receptors while the γδ cells have the γ/δ antigens receptors.</p> | <p>T cells are so named as they differentiate in the [[Thymus - Anatomy & Physiology|thymus]]. They are long lived and are involved in '''cell mediated immunity'''. They represent 60-80% of the circulating lymphocytes and all express the markers CD2, CD3 and CD7 as well as having T cell receptors (TCR). Each T cell has 30,000 TCRs each of which is identical and recognises antigens and major histocompatability complex (MHC) II.</p><p>Functionally they are divided into three subsets that are distinguished by the presence or absence of CD4 or CD8 markers. CD4 and CD8 cells have α/β antigen receptors while the γδ cells have the γ/δ antigens receptors.</p> | ||
| Line 11: | Line 14: | ||
==Helper CD4<sup>+</sup>== | ==Helper CD4<sup>+</sup>== | ||
| − | <p>These T cells express the marker CD4 and are categorised into three groups, | + | <p>These T cells express the marker CD4 and are categorised into three groups, T<sub>H</sub>1 and T<sub>H</sub>2, with a third lineage, T<sub>H</sub>17 being recently described. These lineages are distinguished by the cytokines they produce. T helper cells recognise antigens bound to MHC II complexes. |
| − | * | + | *T<sub>H</sub>1 cells produce IL-2, IFN-γ and TNF-α |
| − | * | + | *T<sub>H</sub>2 cells produce IL-4, IL-5, IL-10 and IL-13 |
| − | * | + | *T<sub>H</sub>17 cells produce IL-17, IL-17F, IL-21 |
| − | + | T<sub>H</sub>1 cells interact with CD8<sup>+</sup>, NK and dendritic cells and T<sub>H</sub>2 cells interact with B cells. T<sub>H</sub>1 cells are involved with the control of intracellular pathogens and T<sub>H</sub>2 cells extracellular pathogens. IL-2 produced by T<sub>H</sub>1 cells stimulates further proliferation of CD4<sup>+</sup> cells. T<sub>H</sub>17 cells are produced to enhance innate immunity, with the cytokines produced increasing the extravasation of neutrophils.</p> | |
| − | <p> | + | <p>T<sub>H</sub>0 populations are CD4<sup>+</sup> cells that have yet to differentiate into T<sub>H</sub>1, T<sub>H</sub>2 or T<sub>H</sub>17 cells and they secrete IL-2, IL-4, IL-5, IFN-γ. In the presence of IL-4 they develop into T<sub>H</sub>2 cells while in the presence of IL-2 they develop into T<sub>H</sub>1 cells. In the abscence of IL-2 T<sub>H</sub>1 cells will change into T<sub>H</sub>2 cells. T<sub>H</sub>17 cells develop in the presence of TGF-β and IL-6 and can further develop into T<sub>H</sub>1 cells depending on various conditions. </p> |
| − | <p> | + | <p>T<sub>H</sub>1 cells have two populations; one that secretes IFN-γ and is short lived, and the other that doesn’t secrete IFN-γ and is long lived. The cells that do not secrete IFN-γ are termed '''memory T cells'''</p> |
| + | <p> T cell differentiation is a field of continual change, with discoveries made on a regular basis. </p> | ||
==Cytotoxic CD8<sup>+</sup>== | ==Cytotoxic CD8<sup>+</sup>== | ||
| Line 23: | Line 27: | ||
*One pathway uses the CD95 (death receptor) which triggers apoptosis in the target cell (usually other T cells) | *One pathway uses the CD95 (death receptor) which triggers apoptosis in the target cell (usually other T cells) | ||
*The other pathway uses perforins and granzymes which form pores in the target cell membrane causing cell lysis | *The other pathway uses perforins and granzymes which form pores in the target cell membrane causing cell lysis | ||
| − | **Perforins are structurally related to complement factor C9 | + | **Perforins are structurally related to [[Complement#Membrane Attack Complex|complement factor C9]] |
**Granzymes are proteolytic enzymes that target cell nucleases and cause apoptosis | **Granzymes are proteolytic enzymes that target cell nucleases and cause apoptosis | ||
| − | In both cases direct contact is required between the T cell and target cell, and cell killing can take several minutes.</p><p> Cytotoxic T cells secrete a pattern of cytokines similar to that of | + | In both cases direct contact is required between the T cell and target cell, and cell killing can take several minutes.</p><p> Cytotoxic T cells secrete a pattern of cytokines similar to that of T<sub>H</sub>1 cells i.e. IFN-γ but not IL-2. IFN-γ shifts the balance of the immune response in favour of TH<sub>1</sub> cells giving an increased level of T cell proliferation. The initiation of the immune response via cytotoxic T cells leads to the selective proliferation of cytotoxic T cells enhancing the main mechanism of killing infected cells.</p> |
==γδ cells== | ==γδ cells== | ||
| Line 33: | Line 37: | ||
*One with restricted antigen binding, that act as first line defence against invading organisms and recognises antigens bound to MHC I complex | *One with restricted antigen binding, that act as first line defence against invading organisms and recognises antigens bound to MHC I complex | ||
*The other subset doesn’t require the MHC complex and this subset has two further divisions | *The other subset doesn’t require the MHC complex and this subset has two further divisions | ||
| − | ** One producing cytokines and chemokines ( | + | ** One producing cytokines and chemokines (T<sub>H</sub>1 and T<sub>H</sub>2) |
**The other having cytotoxic effects.</p> | **The other having cytotoxic effects.</p> | ||
<br><br> | <br><br> | ||
{{Jim Bee 2007}} | {{Jim Bee 2007}} | ||
| + | |||
| + | |||
| + | {{OpenPages}} | ||
[[Category:Lymphocytes|D]] | [[Category:Lymphocytes|D]] | ||
Latest revision as of 17:04, 2 July 2012
Also known as T lymphocytes
See also: T cell differentiation
Introduction
T cells are so named as they differentiate in the thymus. They are long lived and are involved in cell mediated immunity. They represent 60-80% of the circulating lymphocytes and all express the markers CD2, CD3 and CD7 as well as having T cell receptors (TCR). Each T cell has 30,000 TCRs each of which is identical and recognises antigens and major histocompatability complex (MHC) II.
Functionally they are divided into three subsets that are distinguished by the presence or absence of CD4 or CD8 markers. CD4 and CD8 cells have α/β antigen receptors while the γδ cells have the γ/δ antigens receptors.
T-cell receptors
T-cell receptors are the antigen-specific receptors for T-lymphocytes, and are a combination of either α/β chains or γ/δ chains; one T-cell will express either α/β or γ/δ TCRs. The antigen-binding site of the TCR is produced by a combination of the V domains of the relevant chain. Like antibody, the specificity of the TCR is determined by the amino acid composition of the variable domains.
TCRs are linked to the cell membrane; structurally, they look like a single arm of an antibody molecule consisting of a distal domain and a membrane proximal constant domain
Helper CD4+
These T cells express the marker CD4 and are categorised into three groups, TH1 and TH2, with a third lineage, TH17 being recently described. These lineages are distinguished by the cytokines they produce. T helper cells recognise antigens bound to MHC II complexes.
- TH1 cells produce IL-2, IFN-γ and TNF-α
- TH2 cells produce IL-4, IL-5, IL-10 and IL-13
- TH17 cells produce IL-17, IL-17F, IL-21
TH1 cells interact with CD8+, NK and dendritic cells and TH2 cells interact with B cells. TH1 cells are involved with the control of intracellular pathogens and TH2 cells extracellular pathogens. IL-2 produced by TH1 cells stimulates further proliferation of CD4+ cells. TH17 cells are produced to enhance innate immunity, with the cytokines produced increasing the extravasation of neutrophils.
TH0 populations are CD4+ cells that have yet to differentiate into TH1, TH2 or TH17 cells and they secrete IL-2, IL-4, IL-5, IFN-γ. In the presence of IL-4 they develop into TH2 cells while in the presence of IL-2 they develop into TH1 cells. In the abscence of IL-2 TH1 cells will change into TH2 cells. TH17 cells develop in the presence of TGF-β and IL-6 and can further develop into TH1 cells depending on various conditions.
TH1 cells have two populations; one that secretes IFN-γ and is short lived, and the other that doesn’t secrete IFN-γ and is long lived. The cells that do not secrete IFN-γ are termed memory T cells
T cell differentiation is a field of continual change, with discoveries made on a regular basis.
Cytotoxic CD8+
These T cells express the marker CD8 and once fully mature seek and destroy target cells (infected or neoplastic cells). When the cytotoxic T cell recognises the MHC I complex on the target cell (MHC I binds to TCR) the T cell kills that cell -for example with a viral infection, viral peptides associate with MHC I and the CD8+ T cell recognises this and binds to the infected cell. Only two pathways are used by cytotoxic T cells to kill cells:
- One pathway uses the CD95 (death receptor) which triggers apoptosis in the target cell (usually other T cells)
- The other pathway uses perforins and granzymes which form pores in the target cell membrane causing cell lysis
- Perforins are structurally related to complement factor C9
- Granzymes are proteolytic enzymes that target cell nucleases and cause apoptosis
In both cases direct contact is required between the T cell and target cell, and cell killing can take several minutes.
Cytotoxic T cells secrete a pattern of cytokines similar to that of TH1 cells i.e. IFN-γ but not IL-2. IFN-γ shifts the balance of the immune response in favour of TH1 cells giving an increased level of T cell proliferation. The initiation of the immune response via cytotoxic T cells leads to the selective proliferation of cytotoxic T cells enhancing the main mechanism of killing infected cells.
γδ cells
Information on these cells is varied.
They do not express CD4 or CD8 and have γδ antigen receptors rather than α/β like other T cells. They develop in the thymus and migrate to epithelial tissues where they remain. The number present in an individual varies greatly but is generally greatest in immature ruminants and pigs.
The cells can be divided into two subsets:
- One with restricted antigen binding, that act as first line defence against invading organisms and recognises antigens bound to MHC I complex
- The other subset doesn’t require the MHC complex and this subset has two further divisions
- One producing cytokines and chemokines (TH1 and TH2)
- The other having cytotoxic effects.
| Originally funded by the RVC Jim Bee Award 2007 |
Error in widget FBRecommend: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt67293744602bb7_65119885 Error in widget google+: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt672937446a70d0_31854683 Error in widget TwitterTweet: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt67293744715431_89921329
|
| WikiVet® Introduction - Help WikiVet - Report a Problem |