Difference between revisions of "Monocytes"
Kate English (talk | contribs) |
|||
| (14 intermediate revisions by 3 users not shown) | |||
| Line 5: | Line 5: | ||
==Development== | ==Development== | ||
<p>Monocytes develop from the bi-potential [[Haematopoiesis - Overview#Colony Forming Units|CFU-GM]] stem cell during [[Leukopoiesis|leukopoiesis]].</p> | <p>Monocytes develop from the bi-potential [[Haematopoiesis - Overview#Colony Forming Units|CFU-GM]] stem cell during [[Leukopoiesis|leukopoiesis]].</p> | ||
| − | <p>When monocytes leave the blood stream they then differentiate into a number of cells (all are [[Macrophages|macrophages]]): | + | <p>When monocytes leave the blood stream they then differentiate into a number of cells (all are classified as [[Macrophages|macrophages]]): |
* Connective tissue histiocyte | * Connective tissue histiocyte | ||
* [[Respiratory System General Introduction - Pathology#Alveolar macrophages|Alveolar macrophage]] | * [[Respiratory System General Introduction - Pathology#Alveolar macrophages|Alveolar macrophage]] | ||
* Peritoneal macrophage | * Peritoneal macrophage | ||
| − | * Kupffer cell | + | * Liver Kupffer cell |
* Melanophage of skin | * Melanophage of skin | ||
* Lipophage | * Lipophage | ||
* [[Bones - Anatomy & Physiology#Osteoclasts|Osteoclasts]] in bone | * [[Bones - Anatomy & Physiology#Osteoclasts|Osteoclasts]] in bone | ||
| − | * Microglial cell in bone & brain | + | * [[Neurons_- Anatomy & Physiology#Microglial_Cells|Microglial cell]] in bone & brain |
* Specialised histiocytes | * Specialised histiocytes | ||
** Epithelioid cell | ** Epithelioid cell | ||
* Histiocytic giant cell | * Histiocytic giant cell | ||
| − | ** | + | ** Langerhans cell |
| − | + | ** Touton giant cell</p> | |
| − | ** Touton</p> | ||
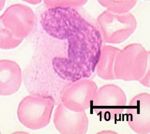
[[Image:Monocyte Picture.jpg|thumb|right|150px|Monocyte Picture - Copyright Prof Dirk Werling DrMedVet PhD MRCVS]] | [[Image:Monocyte Picture.jpg|thumb|right|150px|Monocyte Picture - Copyright Prof Dirk Werling DrMedVet PhD MRCVS]] | ||
| Line 26: | Line 25: | ||
<p>Monocytes can live for months to years in the circulation.</p> | <p>Monocytes can live for months to years in the circulation.</p> | ||
<p>Monocytes are referred to as macrophages once they enter a tissue by '''diapedesis'''.</p> | <p>Monocytes are referred to as macrophages once they enter a tissue by '''diapedesis'''.</p> | ||
| − | <p>Monocytes/macrophages act as phagocytes, removing particular antigens. They also act as antigen presenting cells to take up, process and present antigen to [[ | + | <p>Monocytes/macrophages act as phagocytes, removing particular antigens. They also act as antigen presenting cells to take up, process and present antigen to [[T cells]].</p> |
| − | == | + | ==Monocytosis== |
| − | + | An increase in the number of monocytes (haematogenous macrophages) in the blood is known as a [[Monocytosis|monocytosis]]. It occurs in conjunction with other changes inidicative of a [[Stress Leucogram|stress leucogram]] or it may occur independently. Monocytes in the blood represent a brief transitional stage as they quickly move into tissues and differentiate further to tissue macrophages; they rarely perform any notable functions whilst in the bloodstream but they have been found to phagocytose red blood cells in cases of immune-mediated haemolytic anaemia. The major causes of monocytosis are: | |
| − | + | *Stress leucogram mediated by the production or administration of glucocorticoids (plus a neutrophilia, eosinopenia and lymphopenia). | |
| − | + | *Chronic inflammatory processes, including chronic bacterial infections and chronic inflammatory diseases of the liver (chronic hepatitis and cholangitis) and pancreas (chronic pancreatitis). | |
| − | + | *Granulomatous disease results in monocytosis as monocytes are recruited to contain certain types of bacteria (namely Mycobacteria spp., Nocardia spp., Actinomyces and Rhodococcus equi) or foreign bodies. | |
| − | + | *Certain types of monocytic or myelomonocytic chronic myeloid leukaemia may result in the presence of large numbers of monocytes in the blood. | |
| − | [[Category:Blood_Cells]] | + | [[Category:Blood_Cells]] [[Category:Kate English reviewing]] |
Latest revision as of 12:53, 16 February 2011
Introduction
Monocytes are the largest leukocytes. They have a large indented nucleus, few granules and constitute about 5% of circulating leukocytes. Monocytes are precursors to a number of cells that make up the mononuclear phagocytic system. Developing in the bone marrow, monocytes migrate into the circulation where, after approximately three days, they migrate into tissues and differentiate.
Development
Monocytes develop from the bi-potential CFU-GM stem cell during leukopoiesis.
When monocytes leave the blood stream they then differentiate into a number of cells (all are classified as macrophages):
- Connective tissue histiocyte
- Alveolar macrophage
- Peritoneal macrophage
- Liver Kupffer cell
- Melanophage of skin
- Lipophage
- Osteoclasts in bone
- Microglial cell in bone & brain
- Specialised histiocytes
- Epithelioid cell
- Histiocytic giant cell
- Langerhans cell
- Touton giant cell
Action
During inflammation chemokines attract monocytes which migrate out of blood vessels into the damaged tissue, where they differentiate into cells of the mononuclear phagocytic system.
Monocytes can live for months to years in the circulation.
Monocytes are referred to as macrophages once they enter a tissue by diapedesis.
Monocytes/macrophages act as phagocytes, removing particular antigens. They also act as antigen presenting cells to take up, process and present antigen to T cells.
Monocytosis
An increase in the number of monocytes (haematogenous macrophages) in the blood is known as a monocytosis. It occurs in conjunction with other changes inidicative of a stress leucogram or it may occur independently. Monocytes in the blood represent a brief transitional stage as they quickly move into tissues and differentiate further to tissue macrophages; they rarely perform any notable functions whilst in the bloodstream but they have been found to phagocytose red blood cells in cases of immune-mediated haemolytic anaemia. The major causes of monocytosis are:
- Stress leucogram mediated by the production or administration of glucocorticoids (plus a neutrophilia, eosinopenia and lymphopenia).
- Chronic inflammatory processes, including chronic bacterial infections and chronic inflammatory diseases of the liver (chronic hepatitis and cholangitis) and pancreas (chronic pancreatitis).
- Granulomatous disease results in monocytosis as monocytes are recruited to contain certain types of bacteria (namely Mycobacteria spp., Nocardia spp., Actinomyces and Rhodococcus equi) or foreign bodies.
- Certain types of monocytic or myelomonocytic chronic myeloid leukaemia may result in the presence of large numbers of monocytes in the blood.