| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
|
|
Anatomy and Physiology
Anatomy and Physiology of the thyroid gland can be found here.
Goitre
Refers to a benign enlargement of the throid gland. May be hypofunctional or hyperfunctional. (More often see increased function with neoplasia of the thyroid or the pituitary glands).
Diffuse parenchymatous goitre
Hypofunctional goitre, low levels of thyroglobulin is produced.
Aetiology:
- Dietary iodine deficiency.
- Goitrogenic compounds E.g. Thiocyanates. Reduce uptake of iodine by the thyroid. Includes rape, kale and white clover.
Most often seen as a congenital disease in areas with iodine deficient soil.
Clinical signs:
- Lamb/calf/piglet born dead or moribund.
- Hairless.
- Oedema of head and neck.
Pathophysiology:
No thyroid hormones are produced and there is overstimulation of the thyroid gland by TSH as there is no negative feedback. Histopathologically seen as hyperplasia of the epithelial lining cells as they are stimulated by TSH. Very little colloid is formed as no iodine is available and the epithelial cells form papillary ingrowths into the follicle centre.
Diffuse colloid goitre
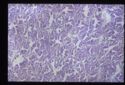
Also hypofunctional. Failure at the pituitary level to produce TSH. TSH is needed for the release of thyroglobulin so without it colloid will accumulate and the follicles will become inactive, seen as:
- Large amounts of densely staining colloid.
- Flattened, low cuboidal epithelium.
- Follicles may coalesce to form cystic spaces.
Usually due to damage to the TSH producing cells of the pituitary.
Nodular goitre
Results from a cycle of hyperplasia and hypoplasia.