Feline Odontoclastic Resorptive Lesions
Also known as: FORL — Neck lesions — Feline Tooth Resorption — Cervical Line Lesions — Dental Resorptive Lesions — Feline Caries — RL
Introduction
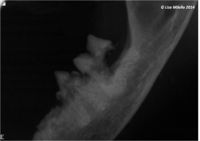
Feline tooth resorption or feline odontoclastic resorptive lesions (RL) (also referred to as cervical line lesions, neck lesions, dental resorptive lesions and feline caries) affect more than one third of adult domestic cats and are the second most common oral problem seen in cats (after periodontitis), with prevalence increasing with age (image 1).
On examination, there is a loss of dental tissue on the crown or at the neck of the tooth. The crown may be completely resorbed with the remaining root covered with gingiva.
Aetiology and Pathogenesis
The aetiology and pathogenesis of FORLs has not yet been demonstrated but is almost certainly multifactorial. Possible hypotheses that have been suggested include, the texture of the diet, abnormal calcium regulation, hypervitaminosis A, mechanical stress, anatomical abnormalities of the teeth, viral infections and plaque bacteria and periodontal disease.
Hard tissues are protected from resorption by their surface layers of blast cells. It appears that as long as these layers are intact, resorption cannot occur. However bone, dentine and cementum are mesenchymal, mineralized tissues composed mainly of collagen and hydroxyapatite, and they differ markedly in their susceptibility to resorption.
Two mechanisms are involved in resorption of hard tissue:
- The trigger
- A reason for the resorption to continue
The trigger mechanism in root resorption is a root surface detached from its protective blast cell layer. For the resorption to continue, a stimulus is required, e.g. infection or a continuous mechanical force.
Root resorption always starts at a surface, and is termed internal if emanating from the root canal wall and as external if emanating from the root surface. Internal resorption is rare in permanent teeth. Histological examination reveals resorption of the internal aspect of the root by multinucleated giant cells adjacent to granulation tissue in the pulp. There are different theories regarding the origin of the pulpal granulation tissue involved in internal resorption. The most logical explanation is that it is pulp tissue that is inflamed because of an infected coronal pulp space. In addition to the requirement of the presence of granulation tissue, root resorption takes place only if the odontoblast layer and predentine are lost or altered. Traditionally, a pink tooth has been thought pathognomonic of internal root resorption; the pink colour is caused by granulation tissue in the coronal dentine undermining the crown enamel. However, a pink tooth can also be a feature of a specific type of external root resorption, namely peripheral inflammatory external root resorption (detailed later), which must be ruled out before a diagnosis of internal root resorption is made. A pink tooth can also be due to pulpal haemorrhage. There are different forms of external root resorption described in man. The underlying mechanism is understood for some of these, whereas other forms are still unexplained and therefore termed idiopathic. A classification system for external root resorptions that have a known mechanism has been proposed in man and is as follows:
- Surface resorption
- Replacement resorption associated with ankylosis
- Inflammatory resorption
This classification system works for external root resorption in cats and dogs as well.
SURFACE RESORPTION - is initiated subsequent to injury of the cementoblast layer. It is thought that minor traumas caused by unintentional biting on hard objects, bruxism, etc. can cause localized damage to the periodontal ligament and trigger this type of resorption. The process is self-limiting and reversible.
REPLACEMENT RESORPTION - results in replacement of the dental hard tissue by bone. When a surface resorption stops, cells from the periodontal ligament will proliferate and populate the resorbed area. Cells from the nearby bone may then arrive first and establish themselves on the resorbed surface. Bone will thus be formed directly upon the dental hard tissue. This results in fusion between bone and tooth, i.e. ankylosis. When the resorptive process is over, the osteoblasts will form bone in the resorbed area. In this way the dental tissues will gradually be replaced by bone.
INFLAMMATORY RESORPTION - In addition to apical root resorption caused by apical periodontitis as a consequence of pulpal necrosis, there are two main forms of external resorption associated with inflammation in the periodontal tissues, namely:
- Peripheral inflammatory root resorption (PIRR)
- External inflammatory root resorption (EIRR).
Both forms are triggered by destruction of the cementoblasts. In PIRR, the osteoclast-activating factors, which perpetuate the resorptive process, are provided by an inflammatory lesion in the adjacent periodontal tissues. EIRR, on the other hand, receives its stimulus for continued resorption from an infected necrotic pulp. In other words, the common factor for these two types of resorption is inflammation in the adjacent tissues.
Tooth resorption in cats accounts for a large proportion of the dental case load seen in general veterinary practice. Most studies have shown an increased incidence with increasing age. The lesions have also been shown to occur in both feral and wild cats, and in other species, e.g. man, dog and chinchilla.
It is likely that the lesions are either peripheral inflammatory root resorption (triggered by inflammation of periodontal tissues) or replacement resorption (idiopathic).
Typical Signalment
There are no sex or breed predispositions, however, it does become more prevalent with age.
Clinical Signs
Anorexia, drooling, lethargy and pain on contact with the lesions.
Clinically, they commonly present as a cavity at the cemento-enamel junction of the tooth. However, studies which included radiography have demonstrated that the resorption can occur anywhere on the root surfaces, i.e. not necessarily at the cemento-enamel junction.
All types of teeth in the feline dentition may be affected by tooth resorption but molar and premolar teeth are more frequently affected than canine and incisor teeth. Also, the buccal/labial surfaces tend to be more likely to be affected compared to the lingual/palatal aspect of the tooth. The lesions are often bilaterally symmetrical.
Diagnosis
The lesions can be detected by means of a combination of visual inspection, tactile examination with a dental explorer and radiography.
Oral Examination
Visual inspection and tactile examination with a dental explorer will only identify end-stage lesions, i.e. when the process involves the crown and has resulted in an obvious cavity.
Signs on visual inspection which are consistent with RLs:
- Focal hyperplastic gingival tissue covering the tooth defect. This gingival covering is usually, but not always, inflamed (image 2).
- Red spot on crown of the tooth as seen in the images (images 3 and 4).
- Missing/fractured teeth; site may have inflamed covering gingiva and/or bony swelling (image 5).
- Root fragments
Intra-Oral Radiography
A definitive diagnosis can only be made after an examination and intra-oral radiography with the cat under general anaesthesia. The lesion can be felt as a concavity using a sharp explorer probe (image 6). Lesions are often only detected once the calculus has been removed.
Visualisation is aided by drying the teeth using the air stream from a dental air-water syringe. With normal teeth, the marginal gingiva will lift away from the tooth when the air is directed at the base of the crown, but with RLs, the soft tissue seems “stuck” to the underlying tooth. General anaesthesia is imperative as examination of these lesions in a conscious cat is painful.
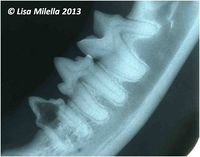
Radiography will identify lesions that are localized to the root surfaces within the alveolar bone, which cannot be detected by clinical methods. Radiography is also required to confirm the diagnosis and to assess the extent and type of the lesion. Radiographs often reveal a lesion that is more advanced than originally suspected from the clinical examination (image 7).
Radiographic Features of RLs:
a) Loss of integrity of the periodontal ligament space.
b) Loss of the lamina dura.
c) Irregularities on the root surface.
d) Diffuse decrease in radiodensity of the entire root compared with adjacent roots.
e) Radiolucent areas within the root dentine often extending into the crown dentine.
f) Replacement of root substance by bone-like tissue.
g) Resorbing roots present with clinically missing crown.
For more information see radiographic interpretation of tooth resorption.
Classifying the Lesions
Classification of tooth resorption :
American Veterinary Dental College classification pictures
| Disease type | Area affected |
|---|---|
| Stage 1 (TR 1) | Mild dental hard tissue loss (cementum or cementum and enamel). |
| Stage 2 (TR 2) | Moderate dental hard tissue loss (cementum or cementum and enamel with loss of dentin that does not extend to the pulp cavity). |
| Stage 3 (TR 3) | Deep dental hard tissue loss (cementum or cementum and enamel with loss of dentin that extends to the pulp cavity); most of the tooth retains its integrity. |
| Stage 4 (TR 4) | Extensive dental hard tissue loss (cementum or cementum and enamel with loss of dentin that extends to the pulp cavity); most of the tooth has lost its integrity. TR4a - Crown and root are equally affected. Extensive dental hard tissue loss (cementum or cementum and enamel with loss of dentin that extends to the pulp cavity); most of the tooth has lost its integrity. |
| Stage 5 (TR 5) | Remnants of dental hard tissue are visible only as irregular radiopacities, and gingival covering is complete. |
Treatment
Currently, the suggested methods for management of odontoclastic resorptive lesions are:
- Conservative management
- Tooth extraction
- Coronal amputation
Historically, restoration of the tooth surface has been recommended for the treatment of accessible lesions that extend into the dentine and do not involve pulp tissue. However, several studies have shown that tooth resorption continues and the restorations are lost. Consequently, the use of restoration of odontoclastic lesions as a major treatment technique cannot be recommended.
Conservative Management
This consists of monitoring the lesions clinically and radiographically. This approach is recommended for lesions that are not evident on clinical examination, i.e. only seen radiographically, and there is no evidence of discomfort or pain. In general practice, most lesions are only diagnosed when pathology is extensive and conservative management is rarely an option.
In most cases, extraction or coronal amputation of an affected tooth is indicated. Preoperative radiographs are mandatory to allow selection of the appropriate treatment option.
Extraction
Teeth with resorption are notoriously difficult to extract, as the root is resorbing and being replaced by bone-like tissue. Moreover, there are areas of ankylosis, i.e. fusion of bone and tooth substance, along the root surface.
Teeth affected by resorption can be extracted using a closed technique, but an open technique is usually less traumatic to the tissues and easier to perform. The teeth are often prone to fracture so an open technique allows good access to any root fragments remaining.
Coronal Amputation
The indications for, and outcome of, coronal amputation have been well documented and the procedure is recommended for selected cases, but needs radiographic monitoring at regular intervals postoperatively to ensure that the root is resorbing and that healing is uneventful. In brief, the technique involves raising a gingival flap to expose the margin of the alveolar bone. The crown of the affected tooth is amputated using a small round bur. A small amount of root tissue is also removed with the bur, just enough to ensure that the intentionally retained root(s) is (are) apical to the alveolar margin. The gingival flap is replaced and sutured in place. This technique is only appropriate for teeth that do not have any radiographic evidence of endodontic disease (ie. periapical inflammation) or periodontitis, and teeth in cats with gingivostomatitis should be removed entirely.
| Feline Odontoclastic Resorptive Lesions Learning Resources | |
|---|---|
To reach the Vetstream content, please select |
Canis, Felis, Lapis or Equis |
 Search for recent publications via CAB Abstract (CABI log in required) |
Feline odontoclastic resorptive lesions publications |
References
Tutt, C., Deeprose, J. and Crossley, D. (2007) BSAVA Manual of Canine and Feline Dentistry (3rd Edition) BSAVA
Merck & Co (2008) The Merck Veterinary Manual Merial
| This article was expert reviewed by Lisa Milella BVSc DipEVDC MRCVS. Date reviewed: 22 October 2014 |
| Endorsed by WALTHAM®, a leading authority in companion animal nutrition and wellbeing for over 50 years and the science institute for Mars Petcare. |
Error in widget FBRecommend: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt69a377203d6d62_48398810 Error in widget google+: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt69a377204db299_39255781 Error in widget TwitterTweet: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt69a377205ce660_65475936
|
| WikiVet® Introduction - Help WikiVet - Report a Problem |