Difference between revisions of "Gastric Ulceration - Dog"
TestStudent (talk | contribs) |
|||
| (16 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
| − | {{ | + | {{unfinished}} |
| − | Also known as: ''''' | + | |
| + | {| cellpadding="10" cellspacing="0" border="1" | ||
| + | | Also known as: | ||
| + | | '''Gastrointestinal ulceration''' | ||
| + | |- | ||
| + | |} | ||
| + | {| cellpadding="10" cellspacing="0" border="1" | ||
| + | | See also: | ||
| + | |'''[[Gastric Ulceration - all species]]''' | ||
| + | |} | ||
| + | |||
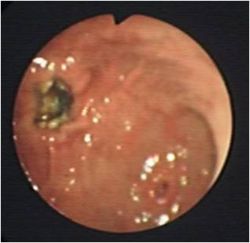
| − | + | [[Image:Gastric ulceration.jpg|thumb|right|250px|Gastric Ulceration - Copyright David Walker RVC]] | |
| − | + | ==Description== | |
| − | + | Is a round or oval punched out lesion of the gastric mucosa ranging from 1-4 cm in diameter. | |
| − | |||
There are many disease associations including: | There are many disease associations including: | ||
| Line 26: | Line 35: | ||
|- | |- | ||
|'''Inflammatory''' | |'''Inflammatory''' | ||
| − | |[[Gastritis, Acute|Gastritis]], [[Pancreatitis - Dog|Pancreatitis]] | + | |[[Gastritis, Acute|Gastritis]], [[Pancreatitis - Dog and Cat|Pancreatitis]] |
|- | |- | ||
|'''Neoplastic''' | |'''Neoplastic''' | ||
| Line 37: | Line 46: | ||
Gastric ulceration is caused by damage to the gastric mucosa through the above mechanisms. [[NSAIDs|NSAIDs]] directly damage the mucosa and interfere with prostaglandin synthesis. Gastric ulceration is worsened by the use of NSAIDs in combination with [[Steroids|corticosteroids]]. This risk can be minimised by using cyclooxygenase-1 (COX-1) sparing NSAIDs. | Gastric ulceration is caused by damage to the gastric mucosa through the above mechanisms. [[NSAIDs|NSAIDs]] directly damage the mucosa and interfere with prostaglandin synthesis. Gastric ulceration is worsened by the use of NSAIDs in combination with [[Steroids|corticosteroids]]. This risk can be minimised by using cyclooxygenase-1 (COX-1) sparing NSAIDs. | ||
| − | Gastric acid hypersecretion following mast cell degranulation of histamine and gastrin secretion from | + | Gastric acid hypersecretion following mast cell degranulation of histamine and gastrin secretion from gastrinomas is a major cause of gastric ulceration. |
==Signalment== | ==Signalment== | ||
| − | |||
Sled dogs are prone to gastric ulceration. | Sled dogs are prone to gastric ulceration. | ||
| + | ==Diagnosis== | ||
==Clinical Signs== | ==Clinical Signs== | ||
History may involve access to toxins and drugs such as [[NSAIDs|NSAIDs]]. | History may involve access to toxins and drugs such as [[NSAIDs|NSAIDs]]. | ||
Clinical Signs can include vomiting, haematemesis, malaena, pale mucous membranes, abdominal pain, weakness, inappetance and hypersalivation which can progress to circulatory compromise. | Clinical Signs can include vomiting, haematemesis, malaena, pale mucous membranes, abdominal pain, weakness, inappetance and hypersalivation which can progress to circulatory compromise. | ||
| + | |||
==Laboratory Tests== | ==Laboratory Tests== | ||
===Haematology=== | ===Haematology=== | ||
| − | [[ | + | [[Anaemia|Anaemia]] which may be regenerative initially, and can progress to microcytic, hypochromic and minutely regenerative anaemia. |
| − | A thrombocytosis may also be present. If a | + | A thrombocytosis may also be present. If a stress leucogram (lymphopenia and neutrophilia) is not present this is supportive of hypoadrenocorticism. |
Examination of the buffy coat may detect mastocytosis. | Examination of the buffy coat may detect mastocytosis. | ||
A [[Neutrophilia|Neutrophilia]] and a left shift are indicative of inflammation or gastric perforation. | A [[Neutrophilia|Neutrophilia]] and a left shift are indicative of inflammation or gastric perforation. | ||
| − | There may also be abnormalities in [[:Category:Haemostasis | + | There may also be abnormalities in [[:Category:Haemostasis|haemostasis]]. |
===Biochemistry=== | ===Biochemistry=== | ||
| Line 62: | Line 72: | ||
===Urinalysis=== | ===Urinalysis=== | ||
| − | Animals will be dehydrated resulting in | + | Animals will be dehydrated resulting in Hypersthenuria. If renal disease is the underlying cause, urine may be isosthenuric. |
===Plain radiography=== | ===Plain radiography=== | ||
| − | [[Image:Gastric ulceration.png|thumb|right|250px|Gastric Ulceration - | + | [[Image:Gastric ulceration.png|thumb|right|250px|Gastric Ulceration - Copyright David Walker RVC]] |
| − | Not usually diagnostic but can rule out differentials such as | + | Not usually diagnostic but can rule out differentials such as foreign bodies and [[Peritonitis|peritonitis]]. |
===Positive contrast radiography=== | ===Positive contrast radiography=== | ||
| Line 75: | Line 85: | ||
===Endoscopy and Biopsy=== | ===Endoscopy and Biopsy=== | ||
| − | Diagnostic test of choice and allows biopsies to be taken. NSAID related ulcers are | + | Diagnostic test of choice and allows biopsies to be taken. NSAID related ulcers are reguarly located in the antrum and there is limited mucosal thickening or irregularity whereas ulcerated [[Gastric Neoplasia|gastric tumours]] will have thickened mucosa and edges. Any biopsies should be taken at the edge of normal and diseased tissue to avoid further deepening or perforation. |
==Treatment== | ==Treatment== | ||
| − | The main aim is to treat any primary underlying cause whilst giving general support. This may be hydrating, restoring electrolytes and acid-base and also helping the gastric lining to recover. | + | The main aim is to treat any primary underlying cause whilst giving general support. This may be hydrating, restoring electrolytes and acid-base and also helping the gastric lining to recover. Anti-ulcerative therapy should be continued for up to 6-8 weeks. |
===[[Principles of Fluid Therapy|Fluid Therapy]]=== | ===[[Principles of Fluid Therapy|Fluid Therapy]]=== | ||
| − | Depends upon the degree of dehydration, | + | Depends upon the degree of dehydration, prescence of shock and any other diseases that are affected by volume. Prolonged vomiting or anorexia may lead to hypokalaemia so KCl may need adding to any fluids given. Normal rates for treatment of shock apply with dehydration being overcome by a fluid rate over 24 hours to replace the defecits along with a maintenance rate. |
===Reducing acid secretion=== | ===Reducing acid secretion=== | ||
[[Gastroprotective Drugs#Histamine (H2) Receptor Antagonists|Histamine receptor antagonists]] inhibit acid secretion and include cimetidine, ranitidine and famotidine. | [[Gastroprotective Drugs#Histamine (H2) Receptor Antagonists|Histamine receptor antagonists]] inhibit acid secretion and include cimetidine, ranitidine and famotidine. | ||
| − | [[Gastroprotective Drugs#Proton Pump Inhibitors|Omeprazole]] is the drug of choice to treat ulceration associated with mass cell tumours and gastrinomas. It inhibits the hydrogen-potassium ATPase which prevents hydrogen ion | + | [[Gastroprotective Drugs#Proton Pump Inhibitors|Omeprazole]] is the drug of choice to treat ulceration associated with mass cell tumours and gastrinomas. It inhibits the hydrogen-potassium ATPase which prevents hydrogen ion prouction by the parietal cells. |
===Mucosal protectants=== | ===Mucosal protectants=== | ||
| Line 108: | Line 118: | ||
==Prognosis== | ==Prognosis== | ||
For animals with peptic ulcers is good. Prognosis is poorer for patients with renal or hepatic failure related ulcers. It is also poor for animals with gastric carcinoma and gastrinoma. | For animals with peptic ulcers is good. Prognosis is poorer for patients with renal or hepatic failure related ulcers. It is also poor for animals with gastric carcinoma and gastrinoma. | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==References== | ==References== | ||
| Line 118: | Line 123: | ||
Hall, J.E., Simpson, J.W. and Williams, D.A., (2005) '''BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition)''' ''BSAVA'' | Hall, J.E., Simpson, J.W. and Williams, D.A., (2005) '''BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition)''' ''BSAVA'' | ||
| − | Ettinger, S.J, Feldman, E.C. (2005) '''Textbook of Veterinary Internal Medicine''' (6th edition, volume 2) | + | Ettinger, S.J, Feldman, E.C. (2005)'''Textbook of Veterinary Internal Medicine''' (6th edition, volume 2)W.B. Saunders Company |
| + | |||
| + | |||
| + | [[Gastric Ulceration - all species]] | ||
| − | |||
| − | + | [[Category:Gastric_Ulceration]][[Category:Dog]] | |
| + | [[Category:To_Do_-_Caz]] | ||
| − | [[Category: | + | [[Category:To_Do_-_Review]] |
| − | |||
Revision as of 09:52, 29 September 2010
| This article is still under construction. |
| Also known as: | Gastrointestinal ulceration |
| See also: | Gastric Ulceration - all species |
Description
Is a round or oval punched out lesion of the gastric mucosa ranging from 1-4 cm in diameter.
There are many disease associations including:
| Disease type | E.g. |
|---|---|
| Hypotension | Shock, Sepsis |
| Drug - induced | Non-steroidal anti-inflammatory drugs (NSAIDs) |
| Idiopathic | Stress, exercise induced |
| Inflammatory | Gastritis, Pancreatitis |
| Neoplastic | Adenocarcinoma, lymphosarcoma, leiomyoma, gastrinoma, (Zollinger-Ellison syndrome), Mast cell Tumours. |
| Metabolic/endocrine | Hypoadrenocorticism, liver disease, uraemia, Disseminated Intravascular Coagulation (DIC), mastocytosis and hypergastrinaemia |
Gastric ulceration is caused by damage to the gastric mucosa through the above mechanisms. NSAIDs directly damage the mucosa and interfere with prostaglandin synthesis. Gastric ulceration is worsened by the use of NSAIDs in combination with corticosteroids. This risk can be minimised by using cyclooxygenase-1 (COX-1) sparing NSAIDs.
Gastric acid hypersecretion following mast cell degranulation of histamine and gastrin secretion from gastrinomas is a major cause of gastric ulceration.
Signalment
Sled dogs are prone to gastric ulceration.
Diagnosis
Clinical Signs
History may involve access to toxins and drugs such as NSAIDs. Clinical Signs can include vomiting, haematemesis, malaena, pale mucous membranes, abdominal pain, weakness, inappetance and hypersalivation which can progress to circulatory compromise.
Laboratory Tests
Haematology
Anaemia which may be regenerative initially, and can progress to microcytic, hypochromic and minutely regenerative anaemia. A thrombocytosis may also be present. If a stress leucogram (lymphopenia and neutrophilia) is not present this is supportive of hypoadrenocorticism. Examination of the buffy coat may detect mastocytosis. A Neutrophilia and a left shift are indicative of inflammation or gastric perforation. There may also be abnormalities in haemostasis.
Biochemistry
Increased liver enzymes and bilirubin, decreased urea, albumin and cholesterol will indicate hepatic disease as an underlying problem. If renal disease is present, an azotaemia will be present on biochemistry. If Hypoadrenocorticism is the cause of the ulceration, it is likely biochemistry will show a Sodium:Potassium ratio of less than 27:1. If the animal is vomiting this will lead to electrolyte and acid-base abnormalities, a metabolic alkalosis, hypokalaemia and hypochloraemia.
Urinalysis
Animals will be dehydrated resulting in Hypersthenuria. If renal disease is the underlying cause, urine may be isosthenuric.
Plain radiography
Not usually diagnostic but can rule out differentials such as foreign bodies and peritonitis.
Positive contrast radiography
May show filling defects.
Ultrasonography
Shows gastric thickening and rules out other differential diagnoses.
Endoscopy and Biopsy
Diagnostic test of choice and allows biopsies to be taken. NSAID related ulcers are reguarly located in the antrum and there is limited mucosal thickening or irregularity whereas ulcerated gastric tumours will have thickened mucosa and edges. Any biopsies should be taken at the edge of normal and diseased tissue to avoid further deepening or perforation.
Treatment
The main aim is to treat any primary underlying cause whilst giving general support. This may be hydrating, restoring electrolytes and acid-base and also helping the gastric lining to recover. Anti-ulcerative therapy should be continued for up to 6-8 weeks.
Fluid Therapy
Depends upon the degree of dehydration, prescence of shock and any other diseases that are affected by volume. Prolonged vomiting or anorexia may lead to hypokalaemia so KCl may need adding to any fluids given. Normal rates for treatment of shock apply with dehydration being overcome by a fluid rate over 24 hours to replace the defecits along with a maintenance rate.
Reducing acid secretion
Histamine receptor antagonists inhibit acid secretion and include cimetidine, ranitidine and famotidine.
Omeprazole is the drug of choice to treat ulceration associated with mass cell tumours and gastrinomas. It inhibits the hydrogen-potassium ATPase which prevents hydrogen ion prouction by the parietal cells.
Mucosal protectants
Such as misoprostol can be given alongside NSAIDs to decrease the risk of ulceration. Sucralfate which is polyaluminium sucrose sulphate, binds to damaged mucosa and assists in the treatment of gastric ulceration. It is best given 2 hours after acid inhibitors to prevent interference.
Prophylaxis
Prophylactic treatment has been shown not to prevent gastric ulceration. Sucralfate is reported to be the best drug in patients receiving high doses of glucocorticoids.
Anti-emetics
Anti-emetics are indicated if vomiting is severe causing fluid and electrolyte imbalances and discomfort.
Analgesia
Is best provided by opiods such as buprenorphine, pethidine and fentanyl.
Antibiotics
Animals suffering from shock and gastric barrier dysfunction may require prophylactic antibiotic cover. First line drugs include ampicillin or a cephalosporin which are effective against Gram-positive, some Gram-negative and some anaerobic bacteria. These can be combined with an aminoglycoside which are effective against Gram-negative aerobes if sepsis is present. Enrofloxacin can also be used instead of an aminoglycoside in skeletally mature animals.
Surgery
May be required to investigate or to resect perforating ulcers which may lead to peritonitis.
Prognosis
For animals with peptic ulcers is good. Prognosis is poorer for patients with renal or hepatic failure related ulcers. It is also poor for animals with gastric carcinoma and gastrinoma.
References
Hall, J.E., Simpson, J.W. and Williams, D.A., (2005) BSAVA Manual of Canine and Feline Gastroenterology (2nd Edition) BSAVA
Ettinger, S.J, Feldman, E.C. (2005)Textbook of Veterinary Internal Medicine (6th edition, volume 2)W.B. Saunders Company