Difference between revisions of "Healing and Repair - Pathology"
Jump to navigation
Jump to search
| (5 intermediate revisions by the same user not shown) | |||
| Line 62: | Line 62: | ||
** This classical dual replacement gives rise to granulation tissue. | ** This classical dual replacement gives rise to granulation tissue. | ||
| − | == | + | ==Repair in the Skin== |
| + | ''Back to [[Integumentary System - Pathology|Integumentary System Pathology]] | ||
| + | * Healing of a wound or surgical incision may be by: | ||
| + | ** '''First intention''' | ||
| + | ** '''Second intention'''. | ||
| − | ==[[ | + | ===Healing by First Intention=== |
| + | * Healing by first intention occurs when the incised ends remain in close apposition to each other anf bacterial contamination is minimal. | ||
| + | ** This may be induced by suturing. | ||
| + | ** For example, a surgical incision. | ||
| + | * Results in minimal scarring. | ||
| + | |||
| + | ====Process==== | ||
| + | * Initially, the incision ruptures the dermal blood vessels. | ||
| + | ** The exuded blood forms a fibrinous clot between and above the incision. | ||
| + | *** The clot functions to: | ||
| + | ***# Stem the flow of blood from the injured site. | ||
| + | ***# Adhere the two ends together. | ||
| + | ***# Prevent infection from entering the injured area. | ||
| + | * The basal layer of epithelium wthin 1mm of the wound edge begins to lose its connections with adjacent basal and overlying epithelium. | ||
| + | ** Undergoes mitosis. | ||
| + | ** Begins to migrate down both sides of the wound under the clot using pseudopodia. | ||
| + | *** As they are migrating, cells differentiate to some degree to form more superficial layers of the epithelium. | ||
| + | **** Gives a rather thick, if not very strong, barrier of epidermis. | ||
| + | *** In the area of migration, the skin is usually hypopigmented and lacks hair follicles. | ||
| + | * Within 2-4 days, the migrating basal layer of epithelium from either side meet together under the clot. | ||
| + | ** It is thought that there is passage of substances, from one side to another that prevents further migration and mitosis. | ||
| + | ** This gives reconstituion of an intact barrier to micro-organisms. | ||
| + | * While the epithelial changes are occuring, there is a sudden proliferation of local fibroblasts and accompanying endothelial cells in the dermis surrounding the incision. | ||
| + | ** These grow across the narrow divide from each side and link up in the middle. | ||
| + | *** Takes about 12 hours to accomplish. | ||
| + | ** In the early stages (days 4-7), their alignment may be vertical, but in later stages (7-21 days) both fibroblasts and capillaries line up horizontally across the incision. | ||
| + | ** This dermal repair forms the major portion of strength between the two sides at this time. | ||
| + | *** Gains in strength over a long period of time as the collagen contracts and remodels according to the stresses imposed upon it. | ||
| + | |||
| + | ====Factors Inhibiting Healing==== | ||
| + | * Factors inhibiting proper wound healing include: | ||
| + | *# '''Protein deficiency''' | ||
| + | *#* May be absolute, as in starvation, or resolute, as in some of the endocrine deficiencies. | ||
| + | *#** E.g. [[Thyroid Gland - Pathology#Hypothyroidism|hypothyroidism]] | ||
| + | *# '''Vitamin C deficiency ''' | ||
| + | *#* Vitamin C is essential for fibroplasia and to maintain the integrity of endothelial and epithelial cells. | ||
| + | *# '''Cold''' | ||
| + | *# '''Ageing''' | ||
| + | *# '''Contamination''' | ||
| + | *#* Infection tends not to be a complication as bacteria are generally excluded. | ||
| + | *#** Retained foreign material such as hair portions or suture material inadvertently left in the wound will cause infection and/or a foreign body reaction. | ||
| + | *# '''Movement''' | ||
| + | *#* Gives persistent trauma. | ||
| + | |||
| + | ===Healing by Second Intention=== | ||
| + | * Healing by second intention occurs when the gap between the ends of the incision is too wide to allow close approximation of the ends. | ||
| + | * This process of granulation tissue repair in a large wound is also the underlying process in the repair of: | ||
| + | ** Infarcts and thrombi in vessels. | ||
| + | ** Surface ulcers and diphtheresis. | ||
| + | ** Pyogenic membrane in abscesses. | ||
| + | ** Diffuse fibrosis ( cirrhosis ) in the [[Liver - Anatomy & Physiology|liver]]. | ||
| + | |||
| + | ====Process==== | ||
| + | * In comparison to healing by first intention, there is a more massive fibroblastic and endothelial proliferation in the wound which fills and repairs the defect. | ||
| + | * There is also considerable surface exudation. | ||
| + | ** The exudate is composed of fibrinous fluid and numerous inflammatory cells, mainly [[Neutrophils|neutrophils]] and macrophages. | ||
| + | *** The cells are scavengers, and engulf necrotic debris and any bacteria present | ||
| + | *** Macrophages and their secretions are also important for the promotion of fibroplasia. | ||
| + | * The fibroblasts tend to align themselves roughly horizontal to the surface, but the endothelium is perpendicular to the surface. | ||
| + | ** The upper vessels form loops near to the surface. | ||
| + | *** Gives the gross appearance of red granules - this is [[Granulation Tissue|granulation tissue]]. | ||
| + | * Well-formed granulation tissue tends to be fairly resistant to surface infection; however, it is rather delicated and so susceptible to trauma and subsequent introduction of infection. | ||
| + | ** Infection is therefore a common complication in the early stages of healing. | ||
| + | * Once the gap has been filled with granulation tissue and is free of infection, the epithelium migrates across. | ||
| + | ** As it migrates, the epithelium secretes collagenolytic substances. | ||
| + | * The epidermis is usually hypopigmented and lacks hair follicles unless they have survived in the granulation tissue. | ||
| + | |||
| + | ==== Factors Inhibiting Healing==== | ||
| + | * Several factors inhibit healing by second intention. | ||
| + | *# '''Movement''' | ||
| + | *#* Movement before sufficient strength has been attained in the bond between the edges can inhibit healing. | ||
| + | *# '''Infections''' | ||
| + | *# '''Corticosteroids''' | ||
| + | *#* Prevent proper collagen matrix formation. | ||
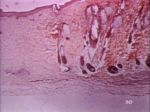
| + | *#* Inhibit leukocyte emigration and phagocytosis.[[Image:scar tissue.jpg|thumb|right|150px|Scar tissue (Courtesy of BioMed Archive)]] | ||
| + | *#* Diminish any acute inflammatory response by generally stabilising cellular membranes. | ||
| + | |||
| + | ====Scarring==== | ||
| + | * As the fibroblasts mature into fibrocytes, the collagen also matures and contracts and there may be extensive scar formation. | ||
| + | ** There may be considerable depression of the surface in such a scar. | ||
| + | ** The scar may interfere with movement in the area. | ||
| + | * The scar tends to diminish in size over a long period of time, as the underlying collagen remodels according to the stresses imposed upon the area. | ||
| + | |||
| + | ==Repair in the Bones== | ||
| + | ===Causes of Fracture=== | ||
| + | * The causes of fracture fit into two distinct categories: | ||
| + | *# '''Fracture of trauma''' | ||
| + | *#* Breakage of normal healthy bone due to excessive stress pressure of short duration. | ||
| + | *# '''Pathological fracture''' | ||
| + | *#* Breakage of bone weakened by some underlying metabolic, inflammatory or neoplastic condition. | ||
| + | |||
| + | ===Description of a Fracture=== | ||
| + | * There are various terms to describe a fracture's appearance. | ||
| + | * Separation of the ends of the fracture may be '''complete''' or '''incomplete'''. | ||
| + | * When there is no penetration of the overlying skin, a the fracture is described as '''closed'''. | ||
| + | * When the sharp ends penetrate the overlying skin, the fracture is '''compound'''. | ||
| + | ** In this scenario there is the danger of introducing infection. | ||
| + | *'''Comminuted''' describes a fracture where there are multiple small fragments of bone at the site of breakage. | ||
| + | * Where the edges of the fracture are impacted into each other, the fracture is said to be '''compressed'''. | ||
| + | * When one side of the fracture is depressed below the plane of the other, the term '''depressed''' is used. | ||
| + | ** This occurs in the flat bones of the skull. | ||
| + | * '''Microfractures''' are fractures that are only visible on histological section as cracks in the bone. | ||
| + | ** Grossly, there might be evidence of some haemorrhage in the area. | ||
| + | |||
| + | ===Fracture Repair=== | ||
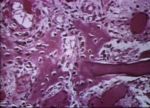
| + | [[Image:fracture repair.jpg|thumb|right|150px|Fracture repair (Courtesy of BioMed Archive)]] | ||
| + | * On breakage, there is rupture of the periosteal, cortical and medullary vessels, causing: | ||
| + | ** A blood clot in the breakage area. | ||
| + | *** Fibrin is the important component. | ||
| + | ** Local necrosis of tissue supplied by these vessels. | ||
| + | *** This lowers the local pH. | ||
| + | * The fate of the blood clot depends upon its location. | ||
| + | ** The periosteal portion is lysed and disappears; | ||
| + | ** The medullary portion is removed by macrophages. | ||
| + | * The necrotic material is removed by phagocytosis. | ||
| + | ** Necrotic [[Bone Marrow - Anatomy & Physiology|bone marrow]] is removed by [[Macrophages|macrophages]]. | ||
| + | *** This is a fairly rapid process. | ||
| + | ** Osteoclasts remove necrotic bone. | ||
| + | *** This is a slow process. | ||
| + | * On the periosteal side, the periosteum proliferates into the clot. | ||
| + | ** Forms a fibrous collar around the bone called the soft callus. | ||
| + | * The cells in the inner aspect of the soft callus, particularly those near the fracture fragments, differentiate into osteoblasts. [[Image:fracture callus.jpg|thumb|right|150px|Fracture callus (Courtesy of BioMed Archive)]] | ||
| + | ** Grow across the divide between the two fragments, laying down coarse woven bone. | ||
| + | * The woven bone laid is known as the hard callus. | ||
| + | ** This periosteal coarse bone is of utmost importance in repair. | ||
| + | *** It is responsible for much of the strength of the fracture repair. | ||
| + | ** This is replaced over a period of time by mature compact bone. | ||
| + | *** Aligns itself according to the stresses applied to it. | ||
| + | * Periosteal cells that are further away from the fracture fragments differentiate into cartilage-producing cells. | ||
| + | ** Produce a cone of cartilage between the two fragments. | ||
| + | *** As the local pH changes to more alkaline conditions, this cartilage undergoes calcification, with invasion by blood vessels and osteoblasts. | ||
| + | **** The cartilage is replaced by bone - endochondral ossification. | ||
| + | * On the medullary side, the endosteum proliferates and invades the clot, laying down bone. | ||
| + | ** This bone may totally occlude the medulla and is later remodelled to reconstitute a patent lumen. | ||
| + | |||
| + | ===Complications=== | ||
| + | * There are several possible complications that may arise in the repair of bone. | ||
| + | # Inadequate immobilisation of the fractured ends will lead to incomplete repair by callus formation. | ||
| + | #* An intervening mass of fibrocartilage remains, forming a false joint. | ||
| + | #** In some cases the false joint can even appear to form a synovial lining. | ||
| + | #* If the fractured ends are sufficiently far apart, no substantial callus forms. | ||
| + | #** The intervening space is taken up by connective tissue organisation. | ||
| + | # Failure to align the fractured ends in proper apposition to one another will produce excessive callus. | ||
| + | #* This takes a longer time to be remodelled by the adult compact bone. | ||
| + | # [[Healing and Repair - Pathology#Description of a Fracture|Comminution]] delays healing due to persistent irritation. | ||
| + | # Infection delays healing due to the effects of the toxins on theproliferating cells. | ||
| + | #* May give rise to a systemic infection affecting the rest of the body. | ||
==Repair in the Respiratory Tract== | ==Repair in the Respiratory Tract== | ||
| Line 73: | Line 223: | ||
* Infectious droplets tend to deposit in the anterior ventral portions of the lobes. | * Infectious droplets tend to deposit in the anterior ventral portions of the lobes. | ||
** I.e. in the apical, cardiac and anterior portions of the diaphragmatic lobes. | ** I.e. in the apical, cardiac and anterior portions of the diaphragmatic lobes. | ||
| − | * Airborne agents produce | + | * Airborne agents produce '''bronchopneumonia'''. |
** So-called because the inflammation is initiated and centred upon the airways. | ** So-called because the inflammation is initiated and centred upon the airways. | ||
* The usual appearance of bronchopneumonia in ruminants and the pig is as the name suggests. | * The usual appearance of bronchopneumonia in ruminants and the pig is as the name suggests. | ||
| Line 83: | Line 233: | ||
*** Air trapped distal to the blockage is gradually absorbed into the bloodstream. | *** Air trapped distal to the blockage is gradually absorbed into the bloodstream. | ||
**** This causes increased pressure on the injured wall, dilating it further. | **** This causes increased pressure on the injured wall, dilating it further. | ||
| − | *** This is a progressive process and results in irreversible dilatation of the airway lumen and is called | + | *** This is a progressive process and results in irreversible dilatation of the airway lumen and is called '''bronchiectasis'''. |
* Bronchopneumonia in the dog and cat often tends to be more diffusely spread. | * Bronchopneumonia in the dog and cat often tends to be more diffusely spread. | ||
** These species have a poorly-developed interlobular septum and collateral ventilation between alveoli from different respiratory units. | ** These species have a poorly-developed interlobular septum and collateral ventilation between alveoli from different respiratory units. | ||
| Line 90: | Line 240: | ||
===Blood-borne Agents=== | ===Blood-borne Agents=== | ||
* Blood-bourne agents tend to have a patchy distribution throughout the lung. | * Blood-bourne agents tend to have a patchy distribution throughout the lung. | ||
| − | * Cause | + | * Cause '''interstitial pneumonia'''. |
====Circulating Toxins==== | ====Circulating Toxins==== | ||
| − | * For example, | + | * For example, "Fog Fever" in adult cattle. |
** Interstitial emphysema. | ** Interstitial emphysema. | ||
** 3-methyl indole is selectively toxic to Type 1 alveolar epithelium. | ** 3-methyl indole is selectively toxic to Type 1 alveolar epithelium. | ||
| Line 226: | Line 376: | ||
**# Chronic mastitis. | **# Chronic mastitis. | ||
**#* Results in progressive destruction of the glandular tissue and replacement by fibrous tissue. | **#* Results in progressive destruction of the glandular tissue and replacement by fibrous tissue. | ||
| − | **#* E.g. [[Streptococcal | + | **#* E.g. [[Streptococcal mastitis - bovine|''Streptococcus agalactiae'']]. |
** Some organisms such as [[Staphylococcus aureus|''Staphylococcus aureus'']] can cause gangrenous, acute and chronic mastitis. | ** Some organisms such as [[Staphylococcus aureus|''Staphylococcus aureus'']] can cause gangrenous, acute and chronic mastitis. | ||
| Line 251: | Line 401: | ||
** Purulent meningitis follows haematogenous spread of infection from umbilical infections and certain septicaemias. | ** Purulent meningitis follows haematogenous spread of infection from umbilical infections and certain septicaemias. | ||
[[Category:Inflammation|B]] | [[Category:Inflammation|B]] | ||
| − | |||
Revision as of 19:09, 1 November 2010
| This article has been peer reviewed but is awaiting expert review. If you would like to help with this, please see more information about expert reviewing. |
Introduction
- There are several factors on which the ability to heal and repair depends:
- Species
- The ability of the species to cope with that particular inflammation .
- For example, peritonitis.
- In cattle, it is often successfully walled off at the initial injury site, preventing spread throughout the whole cavity.
- In the horse peritonitis is not walled off, and is generally rapidly fatal.
- Age
- Repair is generally more successful in younger animals than older animals.
- However, in young animals the immune system may still be immature.
- For example, Pseudorabies virus is more often fatal in pigs under three weeks old, even in the presence of maternal antibody.
- Tissue and extent of damage
- Highly specialised tissue rarely repairs successfully apart from in mild injury.
- If the functional reserve of the damaged tissue is exceeded, clinical signs of disease related to this insufficiency will occur.
- When there is substantial fibrosis in the tissue, the tissue may continue to be progressively destroyed.
- This is due the maturation and contraction of fibrous tissue causing further injury to the adjacent normal tissue.
- E.g. the liver in cirrhosis, and the kidney in chronic renal disease.
- Highly specialised tissue rarely repairs successfully apart from in mild injury.
- Species
Repair
- Repair occurs through one of two mechanisms:
- Regeneration
- Replacement
Regeneration
- In mammals, only epithelial and connective tissues regenerate extensively.
- The ability of tissue to regenerate depends upon whether the tissue is
- Labile
- Stable
- Permanent.
Labile Tissues
- Labile tissues constantly replenish their cells throughout life.
- For example skin and mucous epithelia normally desquamate their outer layer of cells during life, maintaining their overall composition by division of their basal layers.
- Other examples include bone marrow and fat.
- These tissues regenerate well.
- Provided the basement membrane is not breached during the inflammatory process, the epithelium migrates to cover the surface defect.
Stable Tissues
- Stable tissues have a limited ability to replace themselves.
- They retain the ability to
- Replace cells that have undergone programmed cell death when the cells age and cannot continue their function.
- For example, the liver, some endocrine glands and the renal tubular epithelium.
- Respond to greater need for their function in the body.
- Replace cells that have undergone programmed cell death when the cells age and cannot continue their function.
- Blood vessels and fibroblasts are also stable tissues.
- Have great potential to divide and proliferate.
- Are the important tissue cells in repair by replacement.
Permanent
- Permanent tissues have poor or no regenerative capacity.
- This group includes tissues in which the cells are highly specialised and generally have only one function, for example:
- Neuronal cell bodies in the CNS
- The retina of the eye
- The cells responsible for hearing in the ear.
- Axons in the peripheral nervous system can regenerate to a limited extent when severed.
- Cardiac muscle myofibres have very poor regenerative capacity, and undergo repair by
fibrosis or fat replacement.
Replacement
- Replacement is essentially endothelial and fibrous tissue proliferation to replace severely damaged tissue.
- This classical dual replacement gives rise to granulation tissue.
Repair in the Skin
Back to Integumentary System Pathology
- Healing of a wound or surgical incision may be by:
- First intention
- Second intention.
Healing by First Intention
- Healing by first intention occurs when the incised ends remain in close apposition to each other anf bacterial contamination is minimal.
- This may be induced by suturing.
- For example, a surgical incision.
- Results in minimal scarring.
Process
- Initially, the incision ruptures the dermal blood vessels.
- The exuded blood forms a fibrinous clot between and above the incision.
- The clot functions to:
- Stem the flow of blood from the injured site.
- Adhere the two ends together.
- Prevent infection from entering the injured area.
- The clot functions to:
- The exuded blood forms a fibrinous clot between and above the incision.
- The basal layer of epithelium wthin 1mm of the wound edge begins to lose its connections with adjacent basal and overlying epithelium.
- Undergoes mitosis.
- Begins to migrate down both sides of the wound under the clot using pseudopodia.
- As they are migrating, cells differentiate to some degree to form more superficial layers of the epithelium.
- Gives a rather thick, if not very strong, barrier of epidermis.
- In the area of migration, the skin is usually hypopigmented and lacks hair follicles.
- As they are migrating, cells differentiate to some degree to form more superficial layers of the epithelium.
- Within 2-4 days, the migrating basal layer of epithelium from either side meet together under the clot.
- It is thought that there is passage of substances, from one side to another that prevents further migration and mitosis.
- This gives reconstituion of an intact barrier to micro-organisms.
- While the epithelial changes are occuring, there is a sudden proliferation of local fibroblasts and accompanying endothelial cells in the dermis surrounding the incision.
- These grow across the narrow divide from each side and link up in the middle.
- Takes about 12 hours to accomplish.
- In the early stages (days 4-7), their alignment may be vertical, but in later stages (7-21 days) both fibroblasts and capillaries line up horizontally across the incision.
- This dermal repair forms the major portion of strength between the two sides at this time.
- Gains in strength over a long period of time as the collagen contracts and remodels according to the stresses imposed upon it.
- These grow across the narrow divide from each side and link up in the middle.
Factors Inhibiting Healing
- Factors inhibiting proper wound healing include:
- Protein deficiency
- May be absolute, as in starvation, or resolute, as in some of the endocrine deficiencies.
- E.g. hypothyroidism
- May be absolute, as in starvation, or resolute, as in some of the endocrine deficiencies.
- Vitamin C deficiency
- Vitamin C is essential for fibroplasia and to maintain the integrity of endothelial and epithelial cells.
- Cold
- Ageing
- Contamination
- Infection tends not to be a complication as bacteria are generally excluded.
- Retained foreign material such as hair portions or suture material inadvertently left in the wound will cause infection and/or a foreign body reaction.
- Infection tends not to be a complication as bacteria are generally excluded.
- Movement
- Gives persistent trauma.
- Protein deficiency
Healing by Second Intention
- Healing by second intention occurs when the gap between the ends of the incision is too wide to allow close approximation of the ends.
- This process of granulation tissue repair in a large wound is also the underlying process in the repair of:
- Infarcts and thrombi in vessels.
- Surface ulcers and diphtheresis.
- Pyogenic membrane in abscesses.
- Diffuse fibrosis ( cirrhosis ) in the liver.
Process
- In comparison to healing by first intention, there is a more massive fibroblastic and endothelial proliferation in the wound which fills and repairs the defect.
- There is also considerable surface exudation.
- The exudate is composed of fibrinous fluid and numerous inflammatory cells, mainly neutrophils and macrophages.
- The cells are scavengers, and engulf necrotic debris and any bacteria present
- Macrophages and their secretions are also important for the promotion of fibroplasia.
- The exudate is composed of fibrinous fluid and numerous inflammatory cells, mainly neutrophils and macrophages.
- The fibroblasts tend to align themselves roughly horizontal to the surface, but the endothelium is perpendicular to the surface.
- The upper vessels form loops near to the surface.
- Gives the gross appearance of red granules - this is granulation tissue.
- The upper vessels form loops near to the surface.
- Well-formed granulation tissue tends to be fairly resistant to surface infection; however, it is rather delicated and so susceptible to trauma and subsequent introduction of infection.
- Infection is therefore a common complication in the early stages of healing.
- Once the gap has been filled with granulation tissue and is free of infection, the epithelium migrates across.
- As it migrates, the epithelium secretes collagenolytic substances.
- The epidermis is usually hypopigmented and lacks hair follicles unless they have survived in the granulation tissue.
Factors Inhibiting Healing
- Several factors inhibit healing by second intention.
- Movement
- Movement before sufficient strength has been attained in the bond between the edges can inhibit healing.
- Infections
- Corticosteroids
- Prevent proper collagen matrix formation.
- Inhibit leukocyte emigration and phagocytosis.
- Diminish any acute inflammatory response by generally stabilising cellular membranes.
- Movement
Scarring
- As the fibroblasts mature into fibrocytes, the collagen also matures and contracts and there may be extensive scar formation.
- There may be considerable depression of the surface in such a scar.
- The scar may interfere with movement in the area.
- The scar tends to diminish in size over a long period of time, as the underlying collagen remodels according to the stresses imposed upon the area.
Repair in the Bones
Causes of Fracture
- The causes of fracture fit into two distinct categories:
- Fracture of trauma
- Breakage of normal healthy bone due to excessive stress pressure of short duration.
- Pathological fracture
- Breakage of bone weakened by some underlying metabolic, inflammatory or neoplastic condition.
- Fracture of trauma
Description of a Fracture
- There are various terms to describe a fracture's appearance.
- Separation of the ends of the fracture may be complete or incomplete.
- When there is no penetration of the overlying skin, a the fracture is described as closed.
- When the sharp ends penetrate the overlying skin, the fracture is compound.
- In this scenario there is the danger of introducing infection.
- Comminuted describes a fracture where there are multiple small fragments of bone at the site of breakage.
- Where the edges of the fracture are impacted into each other, the fracture is said to be compressed.
- When one side of the fracture is depressed below the plane of the other, the term depressed is used.
- This occurs in the flat bones of the skull.
- Microfractures are fractures that are only visible on histological section as cracks in the bone.
- Grossly, there might be evidence of some haemorrhage in the area.
Fracture Repair
- On breakage, there is rupture of the periosteal, cortical and medullary vessels, causing:
- A blood clot in the breakage area.
- Fibrin is the important component.
- Local necrosis of tissue supplied by these vessels.
- This lowers the local pH.
- A blood clot in the breakage area.
- The fate of the blood clot depends upon its location.
- The periosteal portion is lysed and disappears;
- The medullary portion is removed by macrophages.
- The necrotic material is removed by phagocytosis.
- Necrotic bone marrow is removed by macrophages.
- This is a fairly rapid process.
- Osteoclasts remove necrotic bone.
- This is a slow process.
- Necrotic bone marrow is removed by macrophages.
- On the periosteal side, the periosteum proliferates into the clot.
- Forms a fibrous collar around the bone called the soft callus.
- The cells in the inner aspect of the soft callus, particularly those near the fracture fragments, differentiate into osteoblasts.
- Grow across the divide between the two fragments, laying down coarse woven bone.
- The woven bone laid is known as the hard callus.
- This periosteal coarse bone is of utmost importance in repair.
- It is responsible for much of the strength of the fracture repair.
- This is replaced over a period of time by mature compact bone.
- Aligns itself according to the stresses applied to it.
- This periosteal coarse bone is of utmost importance in repair.
- Periosteal cells that are further away from the fracture fragments differentiate into cartilage-producing cells.
- Produce a cone of cartilage between the two fragments.
- As the local pH changes to more alkaline conditions, this cartilage undergoes calcification, with invasion by blood vessels and osteoblasts.
- The cartilage is replaced by bone - endochondral ossification.
- As the local pH changes to more alkaline conditions, this cartilage undergoes calcification, with invasion by blood vessels and osteoblasts.
- Produce a cone of cartilage between the two fragments.
- On the medullary side, the endosteum proliferates and invades the clot, laying down bone.
- This bone may totally occlude the medulla and is later remodelled to reconstitute a patent lumen.
Complications
- There are several possible complications that may arise in the repair of bone.
- Inadequate immobilisation of the fractured ends will lead to incomplete repair by callus formation.
- An intervening mass of fibrocartilage remains, forming a false joint.
- In some cases the false joint can even appear to form a synovial lining.
- If the fractured ends are sufficiently far apart, no substantial callus forms.
- The intervening space is taken up by connective tissue organisation.
- An intervening mass of fibrocartilage remains, forming a false joint.
- Failure to align the fractured ends in proper apposition to one another will produce excessive callus.
- This takes a longer time to be remodelled by the adult compact bone.
- Comminution delays healing due to persistent irritation.
- Infection delays healing due to the effects of the toxins on theproliferating cells.
- May give rise to a systemic infection affecting the rest of the body.
Repair in the Respiratory Tract
- Severe damage to the alveolar wall results in fibrous tissue organisation of the entire alveolus.
- The appearance of inflammation in the respiratory tract varies with the route of entry of the agent.
Airborne Agents
- Infectious droplets tend to deposit in the anterior ventral portions of the lobes.
- I.e. in the apical, cardiac and anterior portions of the diaphragmatic lobes.
- Airborne agents produce bronchopneumonia.
- So-called because the inflammation is initiated and centred upon the airways.
- The usual appearance of bronchopneumonia in ruminants and the pig is as the name suggests.
- These species have a well developed interstitial septum between groups of lobules, and little or no connection between alveoli from different terminal bronchioles.
- Therefore, one lobule may show extensive pneumonic changes while the adjacent lobule is free from inflammation.
- The inflammatory exudate commonly gets stuck in the lower airways.
- Invokes an inflammatory response in the smooth muscle of the wall of the airway.
- The wall is weakened, causing it to dilate somewhat.
- Air trapped distal to the blockage is gradually absorbed into the bloodstream.
- This causes increased pressure on the injured wall, dilating it further.
- This is a progressive process and results in irreversible dilatation of the airway lumen and is called bronchiectasis.
- Invokes an inflammatory response in the smooth muscle of the wall of the airway.
- These species have a well developed interstitial septum between groups of lobules, and little or no connection between alveoli from different terminal bronchioles.
- Bronchopneumonia in the dog and cat often tends to be more diffusely spread.
- These species have a poorly-developed interlobular septum and collateral ventilation between alveoli from different respiratory units.
- Resolution of bronchopneumonia in the dog and cat is often more or less complete.
Blood-borne Agents
- Blood-bourne agents tend to have a patchy distribution throughout the lung.
- Cause interstitial pneumonia.
Circulating Toxins
- For example, "Fog Fever" in adult cattle.
- Interstitial emphysema.
- 3-methyl indole is selectively toxic to Type 1 alveolar epithelium.
- Derived from excess tryptophan in autumn grass.
Micro-organisms
- A predominantly mononuclear reaction in the alveolar wall can be caused by:
- Viruses
- E.g. Canine Distemper
- Bacteria
- E.g. Salmonella
- Protozoa
- E.g. Toxoplasma gondii
- Viruses
Parasites
- Lungworms (Dictyocaulus vivipara) tend to affect the dorsocaudal areas of the diaphragmatic lobes in their invasion stage as larvae in the blood.
- Later adult stages irritate the airways and also release larvae which are inhaled deeper into the lung.
- In natural outbreaks, both types of lesions are seen.
- May be complicated by bacterial infection.
Traumatic Implantation
- Traumatic implantation is fairly rare.
- Initially causes a pleural inflammation, with some extension to the adjacent lung tissue.
- For example:
- Stake wounds in horses.
- Usually fatal and cause extensive purulent, smelly inflammation.
- Purulent pleuritis in dogs and cats due to Category:Nocardia species from a distant wound.
- Not uncommon in cats.
- May take some time to develop fully after the initial wound or cause has healed.
- Generally fatal.
- Clinical signs only developing when the lesions have become very extensive.
- Stake wounds in horses.
Repair in the Alimentary Tract
The Gut
- The gut is quite prone to infections.
- These are generally kept at bay by the profuse gut associated lymphoid tissue and the continuous movement of ingesta.
- In mild infections, the inflammation is usually catarrhal.
- Particularly in the large intestine where there are numerous goblet cells.
- There is rapid repair by mucosal epithelium.
- More severe infections may damage the structure of the mucosa.
- The villi may be stunted following repair.
- There is a reduced water absorption compounded by loss of electrolytes - malabsorption.
- Results in diarrhoea and progressive loss of weight.
- E.g. in Johne's Disease.
- There is a reduced water absorption compounded by loss of electrolytes - malabsorption.
- The villi may be stunted following repair.
The Liver
- The liver retains limited powers to regenerate and has considerable functional reserve.
- Acute inflammation is often due to viruses and bacteria.
- E.g. Infectious Canine Hepatitis and Salmonellosis in young livestock.
- The liver is swollen and may display hyperaemia.
- Small pinpoint foci of necrosis may be seen through the surface.
- Chronic liver damage results in fibrosis - cirrhosis.
- Generally the sequel to ingestion of a toxic substance over a long period of time.
- E.g Aspergillosis.
- Grossly, the liver shows varying fibrosis imparting a pale or greyish colour.
- In some cases, there may be attempts at nodular regeneration of the hepatic parenchyma.
- Ragwort poisoning has a fairly similar appearance.
- The insidious deposition of fibrous tissue eventually becomes self-perpetuating, causing further damage to remaining hepatocytes as it matures and contracts.
- Eventually neural signs referable to loss of hepatic detoxifying function occur.
The Pancreas
- The pancreas suffers both acute and chronic disease.
- The acute form called acute pancreatic necrosis is the important type in dogs.
- The aetiology is obscure.
- The mechanism involves the release of pancreatic enzymes into the surrounding fatty connective tissue.
- Commonly affects obese females.
- Animals may either die soon after the initial painful episode, or the inflammation smoulders on, often without clinical signs, until there is little pancreatic tissue left.
- Diabetes mellitus or pancreatic insufficiency are common sequelae.
- Chronic pancreatitis is seen in the cat.
- A slow disease often associated with inflammation of both the pancreatic and biliary ducts. *** Fuse before entering the duodenum in cats.
- Grossly, there is reduction in size and sometimes quite extensive periductal fibrosis and inflammation.
Repair in the Urinary Tract
- The kidney has a great functional reserve.
- Only 30% of the tissue is required to function properly.
Glomerulonephritis
- Glomerulonephritis and glomerular deposition of amyloid may cause loss of substantial quantities of protein into the urine.
- Oedema develops in the body, generally first in the back legs, then the ventral subcutis, and perhaps in the abdominal cavity.
- This is called the Nephrotic Syndrome
- Inflammation can arise in the glomeruli, interstitial tissue and in the renal pelvis.
- In the later stages of chronic inflammation, it may be difficult to determine the initial site of the inflammation.
- In severe chronic inflammation, substantial fibrosis of repair can become self-perpetuating.
- Produces more and more damage until the whole kidney appears shrunken and distorted .
- Called "end stage".
- Produces more and more damage until the whole kidney appears shrunken and distorted .
- Signs of uraemia develop once the functional reserve has been exceeded.
- There are also characteristic (though inconsistent) lesions present in other tissues, i.e. the remote effects.
- Inflammation of the tongue and stomach
- Atrial endocarditis
- Parathyroid hyperplasia
- Widespread calcium deposition
- Grossly noticeable intercostal muscles from the pleural aspect.
- Anaemia
- Hypertrophy of the left ventricle of the heart
- Facial loss of bone
- There are also characteristic (though inconsistent) lesions present in other tissues, i.e. the remote effects.
Pyelonephritis
- Important in the cow and sow.
- It tends to be quite acute in the sow, and chronic in the cow.
- Arises from infection ascending the urinary tract.
- There is progressive loss of tissue.
- Starts with necrosis in the pelvic area, then the inflammation spreads up into the cortex.
- Poor prognosis even with therapy.
Cystitis
- Bladder inflammation.
- Common in females.
- A feature of inflammation in the bladder is the considerable dilation of the submucosal vessels - vascular ectasia.
- Bracken fern poisoning initially causes vascular ectasia and inflammation, but can progress
to tumour formation in the bladder.
Repair in the Genital Tract
Female
- Inflammation of the uterus in livestock can take place at two periods:
- At service.
- Mild.
- An endometritis.
- At parturition.
- Can be very severe and life threatening.
- Particularly occurs in assisted parturition.
- Causes a metritis, involving the whole wall.
- At service.
- Pyometra
- Pus in the uterus.
- Occurs commonly in bitches.
- Is life threatening
- Mastitis
- Inflammation of the mammary gland.
- There are several forms of mastitis.
- Life threatening mastitis.
- Occurs shortly after parturition.
- E.g. gangrenous mastitis due to Staphylococcus aureus, and Coliform mastitis.
- Chronic mastitis.
- Results in progressive destruction of the glandular tissue and replacement by fibrous tissue.
- E.g. Streptococcus agalactiae.
- Life threatening mastitis.
- Some organisms such as Staphylococcus aureus can cause gangrenous, acute and chronic mastitis.
Male
- Prostatitis
- Inflammation of the prostate.
- Common in dogs.
- Causes a bag of pus in the tissue.
- Results from an ascending infection of the tract.
- Orchitis
- Inflammation of the testis.
- Rather uncommon.
- In bulls, a granulomatous inflammation occurs with Brucella abortus.
Repair in the Central Nervous System
- Encephalitis
- Inflammation of neural tissue of the brain.
- Repairs by the proliferation of astrocytes.
- Astrocytes are the brain's form of fibrous tissue.
- Called gliosis.
- Perivascular lymphocytic cuffing accompanies neural damage in the brain parenchyma.
- Meningitis
- Inflammation of the meninges.
- Purulent meningitis follows haematogenous spread of infection from umbilical infections and certain septicaemias.