T cells
Also called T lymphocytes
So named as they differentiate in the thymus. They are long lived and are involved in cell mediated immunity. They represent 60-80% of the circulating lymphocytes and all express the markers CD2, CD3 and CD7 as well as having T cell receptors (TCR). Each T cell has 30,000 TCRs each of which is identical and recognises antigens and MHC II.
Functionally they are divided into three subsets that are distinguished by presence or absence of CD4 or CD8 markers. CD4 and CD8 cells have α/β antigen receptors while the γδ cells have the γ/δ antigens receptors.
- T-cell receptors are the antigen-specific receptors for T-lymphocytes
- T-cell receptors are a combination of either αβ chains or γδ chains
- One T-cell will express either αβ OR γδ TCR
- The antigen-binding site of the TCR is produced by a combination of the V domains of either 1α and 1β chain or 1γ and 1δchain
- Like antibody, the specificity of TCR is determined by the amino acid composition of the variable domains
- TCR are always linked to the cell membrane
- Like antibody, TCR consist of a distal domain and a membrane proximal constant domain
- Structurally, they look like a single arm of an antibody molecule
Helper CD4+
These T cells express the marker CD4 and are categorised into two groups, Th1 and Th2, which are distinguished by the cytokines they produce. T helper cells recognise antigens bound to MHC II complex.
- Th1 cells produce Il-2, IFN-γ and TNF-α
- Th2 cells produce Il-4, Il-5, Il-10 and Il-13
Th1 cells interact with CD8+, NK and dendritic cells and Th2 cells interact with B cells. Th1 cells are involved with the control of intracellular pathogens and Th2 cells extracellular pathogens. Il-2 produced by Th1 cells stimulates further proliferation of CD4+ cells.
Th0 populations are CD4+ cells that have yet to differentiate into Th1 or Th2 cells and they secrete Il-2, IL-4, Il-5, IFN-γ. In the presence of Il-4 they develop into Th2 cells while in the presence of Il-12 they develop into Th1 cells. In the abscence of Il-12 Th1 cells will change into Th2 cells.
Th1 cells have two populations. One that secretes IFN-γ and is short lived, and the other that doesn’t secrete IFN-γ and is long lived. The IFN-γ- cells are termed memory T cells (This relationship is not the case for Il-4+ and Il-4- Th2 cells).
For more information on T helper cells click here
Cytotoxic CD8+
These T cells express the marker CD8 and once fully mature seek and destroy target cells (infected or cancer forming cells). When the cytotoxic T cell recognises the MHC I complex on the target cell (MHC I binds to TCR) the T cell kills that cell e.g. viral peptides associate with MHC I and the CD8+ T cell recognises this and binds to the cell. Only two pathways are used by cytotoxic T cells to kill cells:
- One pathway uses the CD95 (death receptor) which triggers apoptosis in the target cell (usually other T cells)
- The other pathway uses perforins and granzymes which form pores in the target cell membrane causing cell lysis
- Perforins are structurally related to complement factor C9
- Granzymes are proteolytic enzymes that target cell nucleases and cause apoptosis
In both cases direct contact is required between the T cell and target cell, and cell killing can take several minutes.
Cytotoxic T cells secrete a pattern of cytokines similar to that of TH1 cells i.e. IFN-γ but not IL-2. IFN-γ shifts the balance of the immune response in favour of TH1 cells giving an increased level of T cell proliferation. The initiation of the immune response via cytotoxic T cells leads to the selective proliferation of cytotoxic T cells enhancing the main mechanism of killing infected cells.
γδ cells
Information on these cells is varied.
They do not express CD4 or CD8 and have γδ antigen receptors rather than α/β like other T cells. They develop in the thymus and migrate to epithelial tissues where they remain. The number present in an individual varies greatly but is generally greatest in immature ruminants and pigs.
The cells can be divided into two subsets:
- One with restricted antigen binding, that act as first line defence against invading organisms and recognises antigens bound to MHC I complex
- The other subset doesn’t require the MHC complex and this subset has a further two subsets
- One producing cytokines and chemokines (Th1 and Th2)
- The other having cytotoxic effects.
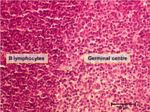
B Cells
Also called B lymphocytes
So named as they were initially found in the Bursa of Fabricius. They produce antibodies (Ig’s) and are associated with humoral immunity. They represent 20-30% of circulating lymphocytes. B cells have B cell receptors (BCR), or antigen binding sites. This is IgM when the B cell is immature, changing to IgD when the cell is mature. B cells also express MHC II, CD9, CD,19, CD20 and CD24.
Under antigenic stimulation they differentiate into plasma cells and memory cells.
B-cells also act as Antigen-Presenting Cells (APCs) by presenting digested fragments to T-cells on MHC II.
For more on B cell differentiation, see here.
Natural Killer (NK) cells
NK cells can be classified as lymphocytes because they are capable of recognising antigen, however they are more often associated with the innate immune response. They target cells by monitoring MHC production, which is expressed by healthy cells to present antigen to T-cells. Low MHC levels can be used as a marker for a cell whose machinery is compromised by a replicating virus. When MHC levels drop, it acts as a danger signal to the NK cells, which then release enzymes to kill the infected cells.
NK cells do not develop in the thymus and represent 5-10% of the circulating lymphocytes. They recognise and kill transformed cells by releasing perforins and granzymes which create channels in the target cell membrane causing lysis. They express the markers CD16, CD56 and CD94.
Natural Killer cells also play a role in Antibody-Dependent Cell-mediated Cytotoxicity
NK Receptors
- Some viruses down-regulate MHC expression of the infected cell
- This is used as a protection against the host immune system
- Lack of MHC inhibits normal T-cell activity
- This is used as a protection against the host immune system
- NK cells can counteract the down-regulation tactic
- They are mainly associated with activity against virus-infected cells and tumour cells, which can also have lowered MHC expression
- The receptors on NK cells do not act like antigen-specific receptors
- Although they trigger functional activity of the cell, they do not stimulate proliferation
- There is no clonal expansion of NK cells
- Although they trigger functional activity of the cell, they do not stimulate proliferation
- NK cells work through two different types of receptors
- Activating receptors, R1
- Recognise pathogen-associated glycolipids or Fc receptors
- E.g. CD16 recognises Ig that is bound to pathogen antigens
- Recognise pathogen-associated glycolipids or Fc receptors
- Suppressing receptors, R2
- Recognise target cell MHC molecules
- Activating receptors, R1
- When an NK cell interacts with a target cell it will be activated via R1
- If the target cell expresses MHC this will be seen by R2
- R2 suppresses the activities of the NK cells
- Therefore, NK cells do not affect normal cells
- R2 suppresses the activities of the NK cells
- If the target cell does not express MHC, the suppressing receptors are not engaged
- Cell activity is not suppressed
- The engagement of R1 therefore causes activation of the NK cells
- Cell activity is not suppressed
- If the target cell expresses MHC this will be seen by R2
When NK cells are activated, they:
- Secrete a range of cytokines, including:
- Tumour necrosis factor alpha; (TNFα)
- A potent stimulator of acute inflammation
- Can cause target cell killing directly and also via stimulated macrophages
- Interferon gamma; (IFNγ)
- Stimulates macrophages
- Active against the target cells
- Stimulates target cell expression of MHC
- Makes target cells susceptible to normal T-cell killing.
- Tumour necrosis factor alpha; (TNFα)
- Initiate killing of the target cell
Lymphocyte Surveillance
About two thirds of lymphocytes (all immunocompetent) are circulating in the blood and lymph systems. Most of these are T cell and long lived. In the lymphatic system they survey tissues. The other third do not circulate and are either short lived or immature, or can be specific cells destined for certain tissues i.e. cells that line connective tissue under the epithelium of respiratory, intestinal and urogential systems.
High Endothelial Venules (HEV) are used for lymphocytes to access the lymph nodes from the bloodstream. Once inside the lymph node, the naive lymphocytes search for antigen. If there is no antigen present, the naive lymphocytes leave via the efferent lymphatic vessel and return back to the bloodstream. Each lymphocyte can search several secondary lymphoid organs each day. This process is called surveillance.
If a naive lymphocyte recognises an antigen then it differentiates into its adult (mature) form. Interdigitating dendritic cells present antigen to T cells and follicular dendritic cells present antigen to B cells.
B cells proliferate into plasma cells in germinal centres, producing antibody.
T cells leave the lymph node in attack mode to locate the infectious organism. The surface molecule L-selectin (which allows the naive lymphocyte to enter the lymph node via an HEV) is replaced by the adhesion molecule VLA-4. At the site of inflammation, the VLA-4 receptor recognises VCAM-1 on endothelial cells and the T cell enters the site of disease. CD4+ T cells search for infected macrophages and CD8+ T cells look for virus infected cells creating an immune response. After the infection has been defeated, memory cells develop which express L-selectin (rather than VLA-4) and continue to search the body in surveillance mode in case the host is re-infected with the disease producing organism.
Additional Resources
Websites
Pages in category "Lymphocytes"
The following 7 pages are in this category, out of 7 total.