Difference between revisions of "Liver - Anatomy & Physiology"
Rachelmcl13 (talk | contribs) m (→Histology) |
Fiorecastro (talk | contribs) |
||
| Line 65: | Line 65: | ||
==Bile Acids== | ==Bile Acids== | ||
| − | Bile acids are composed of cholesterol, bile acids and steroids. The main bile acid is '''cholic acid''' (C24). Conjugated to taurine or glycine in the liver to reduce pKa so they exist in an ionised form as bile salts. Bile salts conjugate with cholesterol and phospholipids and are then secreted into the bile. | + | Bile acids are synthesised in the liver from cholesterol and are conjugated with taurine or glycine before excretion as bile salts into the bile. Once fat absorption in the small intestine has been completed bile acids are re-absorbed in the ileum. Bacterial action in the intestine deconjugates some to bile acids and converts the rest to secondary bile salts. Around 95% of bile acids and salts are re-absorbed, these products enter the portal circulation and are extracted and recycled by the hepatocytes (enterohepatic circulation). This is normally a highly efficient process but when there is reduced hepatic function some of these bile acids are not extracted and can be measured in the peripheral blood. References: [[NationWide Laboratories]] |
| + | |||
| + | Bile acids are composed of cholesterol, bile acids and steroids. The main bile acid is '''cholic acid''' (C24). Conjugated to taurine or glycine in the liver to reduce pKa so they exist in an ionised form as bile salts. Bile salts conjugate with cholesterol and phospholipids and are then secreted into the bile. They emulsify fats which helps absorb fat soluble vitamins. In aqueous solution, they form micelles which are amphiphilic and can transport free fatty acids across the brush border. | ||
| + | |||
| + | === Small animals === | ||
| + | The measurement of fasting bile acid levels is at least as sensitive as either the bromsulphthalein clearance test or the ammonia tolerance test as a measure of hepatic function. Pre and post feeding bile acids are measured on a 8-12 hour fasted sample and a sample taken 2 hours post feeding. This is more sensitive than a single fasted sample. However, it can be difficult to balance the quantity of food required to stimulate gallbladder contraction with the presence of postprandial lipaemia which interferes with the assay, and is noted if a large amount of food is given. Feeding a normal meal is recommended, but this approach may need to be tailored for individual patients. A fatty meal or oil supplementation is not required to stimulate gallbladder contraction. | ||
| + | |||
| + | The measurement of bile acids is useful in the investigation of hepatic disease, but the interpretation can be complex and a number of factors should be considered | ||
| + | |||
| + | * The bile acid result does not provide specific information regarding the nature or reversibility of hepatic changes | ||
| + | |||
| + | * The degree of increase does not correlate well with the severity of disease | ||
| + | |||
| + | * Increases are noted with extrahepatic disease for example, intestinal disease, etc. Commonly the increase in bile acids is only mild, but increases up to 100μmol/l have been noted occasionally | ||
| + | |||
| + | * Concentrations above 30μmol/l correlate with the presence of histological changes in the liver but these could be associated with primary or secondary hepatopathies | ||
| + | |||
| + | * Some authors suggest that increases above 40μmol/l correlate well with the presence of primary hepatic disease, but the cut-off is a matter of controversy | ||
| + | |||
| + | * It is not necessary to measure bile acids where there is hyperbilirubinaemia secondary to cholestasis | ||
| + | |||
| + | * A postprandial result lower than the one on the fasted sample is seen in some cases. The cause is not always clear (for example, failure of stomach to empty or gall bladder to contract, too fast or too slow intestinal transit, SIBO) but it is recommended to interpret the higher of the results. | ||
| + | |||
| + | ===== Causes of increased bile acids ===== | ||
| + | |||
| + | * Congenital or acquired portosystemic shunt | ||
| + | * Reduced hepatocellular function (decreased hepatocellular mass) | ||
| + | * Cholestasis | ||
| + | |||
| + | ===== Complementary tests ===== | ||
| + | Tests for cholestasis (ALP, GGT and bilirubin) and hepatic function (albumin, urea, glucose, cholesterol) are indicated along with tests for hepatocellular damage (ALT, AST and GLDH). | ||
| + | |||
| + | === Equine === | ||
| + | As in the dog and cat, bile acids are conjugated largely with taurine. The rate of enterohepatic circulation is fairly constant and horses do not possess a gall bladder, therefore fasting and stimulation testing is not required. | ||
| + | |||
| + | ===== Causes of increased bile acids ===== | ||
| + | |||
| + | * Hepatic insufficiency | ||
| + | |||
| + | * Cholestasis | ||
| + | |||
| + | * Portosystemic shunt | ||
| + | |||
| + | ===== Complementary tests ===== | ||
| + | Tests for cholestasis (ALP, GGT and bilirubin) and hepatocellular damage (AST and GLDH). Albumin is less useful as an indicator of hepatic insufficiency in the horse than in small animals due to its long half life (hypoalbuminaemia is only seen in advanced liver failure). Liver biopsy and ultrasound examination may be required to confirm the aetiology and provide prognostic information. | ||
| + | |||
| + | Small animal and Equine references: [[NationWide Laboratories]] | ||
==Species Differences== | ==Species Differences== | ||
| Line 113: | Line 159: | ||
**Zone 3 - centrilobular (periacinar), bordering the hepatic venules | **Zone 3 - centrilobular (periacinar), bordering the hepatic venules | ||
NB: blood enters from Zone 1 to Zone 3 and thus becomes less and less oxygenated | NB: blood enters from Zone 1 to Zone 3 and thus becomes less and less oxygenated | ||
| + | |||
| + | == References == | ||
| + | Text referenced 'Nationwide Laboratories': [[NationWide Laboratories]] | ||
==Links== | ==Links== | ||
Revision as of 18:35, 15 March 2022
Introduction
The liver (hepar) is an extremely important organ in the body of mammals and vertebrates as it provides functions essential for life. It is the largest internal organ and has numerous functions including production of bile and protein, fat and carbohydrate metabolism. During foetal development, the liver has an important haemopoetic function, producing red and white blood cells from tissue between the hepatic cells and vessel walls.
The size of the liver varies due to its role in metabolism. In carnivores the liver weighs about 3-5% of body weight, in omnivores 2-3% and in herbivores 1.5%. the liver is much heavier in young animals than older animals as it atrophies with age.
The liver is derived from an outpocketing of endoderm epithelium on the ventral duodenum from the caudal part of the foregut. The connection to the gut narrows to become the bile duct. The parenchymal tissue of the liver is formed from proliferating epithelial cords or strands which integrate with the blood sinuses of the umbilical and vitelline veins. The mesoderm of the septum transversum forms the venous sinosoids and connective tissue of the liver.
Structure
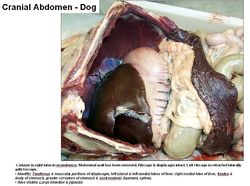
The liver is located in the cranial part of the abdomen. It is immediately caudal to the diaphragm and cranial to the stomach and intestines. Generally the bulk of the liver is on the right of the midline. It is divided into lobes by fissures. Cranially the liver is convex, called the diaphragmatic surface. Caudally the liver is concave, called the visceral surface. The caudate lobe has a renal impression from the right kidney. The gastric impression occupies the whole of the left half of the visceral face. The duodenal impression at the junction of the right and quadrate lobes continues onto the right lateral and caudate lobes. Passages or notches on the median plane allow the caudal vena cava and oesophagus to pass by. The gall bladder is located between the right medial and quadrate lobes. Reticular fibres (collagen type III, proteoglycans and glycoproteins) support the hepatocytes and walls of the sinusoids. Interlobular spaces support bile ducts and blood vessels. The lesser omentum (often fat filled) is on the visceral surface between the left lateral lobe, heptic porta and lesser curvature of the stomach. There is a oesophageal notch where the oesophagus passes over the liver.
Divisions of the Liver
The liver can be divided into lobes, lobules, hepatocytes and sinusoids.
Lobes of the Liver
The lobes of the liver include the left lateral, left medial, right lateral, right medial, quadrate, caudate and papillary.
Ligaments
The coronary ligament attaches the liver (from the diaphragmatic surface) to the diaphragm. It is an irregular fold of peritoneum. It surrounds the triangular base of the diaphragmatic surface. It is continuous with outer most layer of the caudal vena cava. The falciform ligament is ventral to the coronary ligament. It is a fat filled embryological remnant of the fetal blood vessels from the placenta. It causes problems for surgical entry into the abdomen. It is located cranial to the umbilicus and is a vestige of the umbilical vein. The triangular ligament is on the right and left sides of the coronary ligament.
Function
Production of bile see Bile Formation.
Nearly all the blood circulated around the abdomen flows back through the portal vein to the liver where it comes in contact with the liver cells, ensuring the products of digestion are presented to the hepatic cells before entering the general circulation. Other functions include carbohydrate metabolism, glycogenesis, glyconeolysis, gluconeogenesis and the breakdown of insulin and other hormones. Protein metabolism produces soluble mediators of the clotting cascade, Albumin and hormone transporting globulins. The liver is also involved in lipid metabolism, lipogenesis and the synthesis of cholesterol.
The liver has a role in hormonal control of the following; Insulin and glucagon, Glucocortocoids, Catecholamines and the synthesis of other important hormones (see Endocrine System). It also has a role in immunoregulation via kupfer cells and the complement synthesis and metabolism.
The liver is important in storage of water soluble vitamins, fat soluble vitamins, iron, triglyceride and glycogen.
The liver breaks down haemoglobin and toxic substances through drug metabolism. It converts ammonia to urea and allows the management of endogenous waste, e.g haem (Hb, cytochromes, Mb) and ammonia (amino acids).
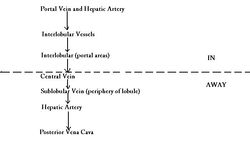
Vasculature
The liver has a dual blood supply. 70-80% via the hepatic portal vein (nutrient rich) and 20-30% via the hepatic artery (oxygen rich). It has a large blood supply (nearly a 1/3 of cardiac output passes through the liver).
The hepatic artery is a branch of the caeliac artery. The portal vein is formed by tributaries draining the spleen, pancreas and digestive tract. Intrahepatic arteries combine with portal vein branches to supply the connective tissue and hepatic sinusoids of the liver. Blood flows from the portal areas into the central vein. The central vein is lined by simple squamous epithelium. The bile duct, blood vessels (including the important hepatic vein) and nerves enter and leave the liver at the hepatic porta. Blood from the central vein opens into the caudal vena cava. Liver circulation is controlled by interarterial, intervenous, arteriovenous, and by sphincter mechanisms, allowing careful regulation.
Innervation
The liver is innervated by sympathetic nerves from the periarterial plexuses and parasympathetic nerves from the vagal trunk.
Lymphatics
Efferent vessels pass to hepatic nodes around the hepatic porta. The lymph drains into the visceral cysterna chyli. Some lymph travels to the accessory hepatic and caudal mediastinal lymph nodes on the caudal vena cava.
Hepatic Duct Systems
There are canaliculi within lobules. Canaliculi open into larger ductules then into a few large hapatic ducts. Before and shortly after leaving the hepatic porta, the ducts combine into a single trunk which runs to the duodenum. The cystic duct runs from common trunk to the gall bladder transporting bile from the liver to the gall bladder. Distal to the cystic duct is the bile duct (ductus choledochus) which transports bile from the gall bladder into the duodenum. There are no valves, so bile may flow in either direction.
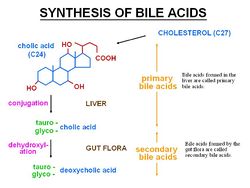
Bile Acids
Bile acids are synthesised in the liver from cholesterol and are conjugated with taurine or glycine before excretion as bile salts into the bile. Once fat absorption in the small intestine has been completed bile acids are re-absorbed in the ileum. Bacterial action in the intestine deconjugates some to bile acids and converts the rest to secondary bile salts. Around 95% of bile acids and salts are re-absorbed, these products enter the portal circulation and are extracted and recycled by the hepatocytes (enterohepatic circulation). This is normally a highly efficient process but when there is reduced hepatic function some of these bile acids are not extracted and can be measured in the peripheral blood. References: NationWide Laboratories
Bile acids are composed of cholesterol, bile acids and steroids. The main bile acid is cholic acid (C24). Conjugated to taurine or glycine in the liver to reduce pKa so they exist in an ionised form as bile salts. Bile salts conjugate with cholesterol and phospholipids and are then secreted into the bile. They emulsify fats which helps absorb fat soluble vitamins. In aqueous solution, they form micelles which are amphiphilic and can transport free fatty acids across the brush border.
Small animals
The measurement of fasting bile acid levels is at least as sensitive as either the bromsulphthalein clearance test or the ammonia tolerance test as a measure of hepatic function. Pre and post feeding bile acids are measured on a 8-12 hour fasted sample and a sample taken 2 hours post feeding. This is more sensitive than a single fasted sample. However, it can be difficult to balance the quantity of food required to stimulate gallbladder contraction with the presence of postprandial lipaemia which interferes with the assay, and is noted if a large amount of food is given. Feeding a normal meal is recommended, but this approach may need to be tailored for individual patients. A fatty meal or oil supplementation is not required to stimulate gallbladder contraction.
The measurement of bile acids is useful in the investigation of hepatic disease, but the interpretation can be complex and a number of factors should be considered
- The bile acid result does not provide specific information regarding the nature or reversibility of hepatic changes
- The degree of increase does not correlate well with the severity of disease
- Increases are noted with extrahepatic disease for example, intestinal disease, etc. Commonly the increase in bile acids is only mild, but increases up to 100μmol/l have been noted occasionally
- Concentrations above 30μmol/l correlate with the presence of histological changes in the liver but these could be associated with primary or secondary hepatopathies
- Some authors suggest that increases above 40μmol/l correlate well with the presence of primary hepatic disease, but the cut-off is a matter of controversy
- It is not necessary to measure bile acids where there is hyperbilirubinaemia secondary to cholestasis
- A postprandial result lower than the one on the fasted sample is seen in some cases. The cause is not always clear (for example, failure of stomach to empty or gall bladder to contract, too fast or too slow intestinal transit, SIBO) but it is recommended to interpret the higher of the results.
Causes of increased bile acids
- Congenital or acquired portosystemic shunt
- Reduced hepatocellular function (decreased hepatocellular mass)
- Cholestasis
Complementary tests
Tests for cholestasis (ALP, GGT and bilirubin) and hepatic function (albumin, urea, glucose, cholesterol) are indicated along with tests for hepatocellular damage (ALT, AST and GLDH).
Equine
As in the dog and cat, bile acids are conjugated largely with taurine. The rate of enterohepatic circulation is fairly constant and horses do not possess a gall bladder, therefore fasting and stimulation testing is not required.
Causes of increased bile acids
- Hepatic insufficiency
- Cholestasis
- Portosystemic shunt
Complementary tests
Tests for cholestasis (ALP, GGT and bilirubin) and hepatocellular damage (AST and GLDH). Albumin is less useful as an indicator of hepatic insufficiency in the horse than in small animals due to its long half life (hypoalbuminaemia is only seen in advanced liver failure). Liver biopsy and ultrasound examination may be required to confirm the aetiology and provide prognostic information.
Small animal and Equine references: NationWide Laboratories
Species Differences
Canine & Feline
Both the left and right lobes are subdivided. Complete obstruction of the hepatic artery is fatal. The liver is almost entirely intra-thoracic. An enlarged caudate process contacts the right kidney.
Equine
The liver is contained entirely within the rib cage, to the right of the midline. It is less lobated. There is no gall bladder and the left lobe is subdivided. There is no papillary lobe. In the foal, the liver is larger and more symmetrical. The bile duct opens into the duodenum at the same papillae as the major pancreatic duct. Bile is constantly secreted.
Porcine
The liver has deep interlobular fissures and a large amount of interlobular connective tissue. It has a mottled appearance. A Deep interlobular fissure divides the liver into 4 lobes- the left, right, medial and lateral. There is a small caudate lobe (which does not contact the kidney so no renal impression). It is mostly on the right of the midline and has no papillary lobe.
Ruminants
The liver is entirely displaced to right of the midline. It has fused lobes.
Small Ruminants Sheep have a deeper umbilical fissure than cows. Sheep also have a smaller caudate lobe than cows and have two papillary processes.
Avian
See avian liver
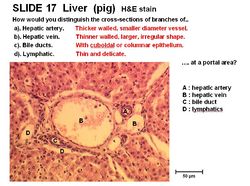
Histology
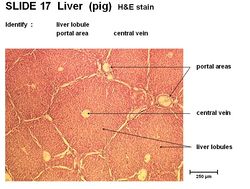
The larger liver cells are called lobules. Each lobule contains an opening for the central vein and contains portal areas. The lobules are composed of liver cords called hepatocytes. Sinusoids are present between hepatocytes containing red blood cells. There is a connective tissue capsule around each liver lobule. A thin mesothelium covers the connective tissue layer.
The portal area present in the lobules contains the hepatic artery, which has thick walls and a small diameter and the hepatic vein, which has thin walls and a large and irregular shape. It also contains bile ducts, with cuboidal or columnar epithelium and lymphatics that are small and delicate.
Hepatocytes are the smaller liver cells in the lobules. They contain glycogen granules and have a spherical nucleus. They form cords called branching plates (lamellae). The upper and lower margins are tight junctions. They have 3 functioning surfaces. Kupfer macrophages are present near the lining of the sinusoids. The hepatocytes stain pink as they are eosinophilic.
Acinus
- the smallest functional unit of the liver - this unit stresses the dependence of the liver on its afferent blood vessels and efferent bile ducts
- a roughly diamond shaped parenchymal mass surrounding and supplied by the portal area
- consists of 3 zones:
- Zone 1 - periportal (centroacinar), around the portal areas
- Zone 2 - midzonal
- Zone 3 - centrilobular (periacinar), bordering the hepatic venules
NB: blood enters from Zone 1 to Zone 3 and thus becomes less and less oxygenated
References
Text referenced 'Nationwide Laboratories': NationWide Laboratories
Links
Click here for information on pathology of the Liver
Click here for information on Hepatic Stellate Cells
Click here for information on Bile Formation
Click here for information on portosystemic shunting
| Liver - Anatomy & Physiology Learning Resources | |
|---|---|
To reach the Vetstream content, please select |
Canis, Felis, Lapis or Equis |
 Test your knowledge using drag and drop boxes |
Compare liver structure in different species |
 Test your knowledge using flashcard type questions |
Liver - Anatomy & Physiology - Flashcards |
 Selection of relevant videos |
Bovine liver potcast Bovine liver potcast 2 Ovine liver with hepatitis cysticercosa potcast Equine liver with hydatid cysts potcast Equine liver potcast Liver lobes of the Horse Liver lobes of the Cow |
 Selection of relevant PowerPoint tutorials |
Histology of the liver - see part 2 |
Error in widget FBRecommend: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt662d0276e865d6_65772572 Error in widget google+: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt662d0276eb87d1_17068850 Error in widget TwitterTweet: unable to write file /var/www/wikivet.net/extensions/Widgets/compiled_templates/wrt662d0276eea914_16915708
|
| WikiVet® Introduction - Help WikiVet - Report a Problem |