Difference between revisions of "Thyroid Gland - Anatomy & Physiology"
Fiorecastro (talk | contribs) |
|||
| (10 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
| − | + | [[Image:Thyroid Gland Low Power.jpg|right|thumb|300px|©RVC 2008]] | |
| − | |||
| − | |||
== Embryological Origin == | == Embryological Origin == | ||
| − | The thyroid gland is a downgrowth from the pharyngeal endoderm of the developing | + | The thyroid gland is a downgrowth from the pharyngeal endoderm of the developing tongue. |
| + | |||
| + | <br> | ||
==Anatomy== | ==Anatomy== | ||
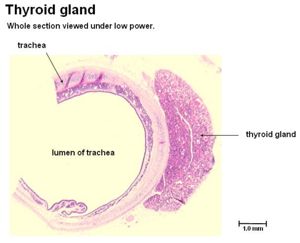
The thyroid gland consists of two lobes (dog, horse), one on each lateral side of the cranial [[Trachea - Anatomy & Physiology|trachea]]. In the pig the lobes are connected by an ''isthmus'' with a small, central ''pyramidal lobe'' as part of that structure. Cattle have a particularly wide isthmus. | The thyroid gland consists of two lobes (dog, horse), one on each lateral side of the cranial [[Trachea - Anatomy & Physiology|trachea]]. In the pig the lobes are connected by an ''isthmus'' with a small, central ''pyramidal lobe'' as part of that structure. Cattle have a particularly wide isthmus. | ||
| + | <br> | ||
===Location=== | ===Location=== | ||
| − | The thyroid gland is located adjacent to the cranial | + | The thyroid gland is located adjacent to the cranial trachea. Close to the ''Recurrent Laryngeal nerve'', carotid sheath and Sternohyoid and Sternothyroid muscles. The [[Parathyroid Glands - Anatomy & Physiology|'''Parathyroid Glands''']] are located dorsally to, or within the thyroid gland itself. |
| + | <br> | ||
===Supply=== | ===Supply=== | ||
| − | The thyroid gland is supplied by the ''' | + | The thyroid gland is supplied by the '''Cranial Thyroid artery''' which is a branch of the common carotid artery. A subsidiary supply is provided by the '''Caudal Thyroid artery'''. The cranial and caudal thyroid arteries are united by substantial anastamoses along their caudal edge. Venous drainage is provided by the Internal Jugular vein and [[Lymph - Anatomy & Physiology|Lymph]] drains into the cranial Deep Cervical nodes. |
| + | <br> | ||
===Ultrastructure and Histology=== | ===Ultrastructure and Histology=== | ||
| − | The gland consists of varying sized follicles | + | [[Image:Thyroid Gland Labelled.jpg|right|thumb|300px|'''Normal Thyroid Gland. ©RVC 2008]] |
| − | + | <br> | |
| − | Within the connective tissue close to the follicles are '''C- | + | The gland consists of varying sized follicles. These are a single layer of cuboidal epithelial cells: '''Follicular Cells''' surrounding a central lumen filled with a protein rich colloid (thyrogloblin). The apical surface of the cell membranes is covered with numerous micovilli to increase surface area. The follicular cells are connected by tight junctions, and have a dense capillary network. |
| + | <br> | ||
| + | Within the connective tissue close to the follicles are '''C-Cells''' alternatively known as '''Parafollicular Cells'''. These secrete ''Calcitonin'', a hormone which acts to lower plasma Ca2+ levels. | ||
| + | <br> | ||
| + | ====Histology==== | ||
<center><gallery> | <center><gallery> | ||
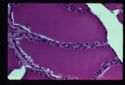
Image:Thyroid Gland Low Power.jpg|<p>''' Thyroid Gland Low Power 1'''</P><sup>©RVC 2008</sup> | Image:Thyroid Gland Low Power.jpg|<p>''' Thyroid Gland Low Power 1'''</P><sup>©RVC 2008</sup> | ||
| Line 29: | Line 36: | ||
</gallery></center> | </gallery></center> | ||
| + | <br> | ||
==Thyroid Hormone Physiology== | ==Thyroid Hormone Physiology== | ||
| − | Follicular cells synthesize ''' | + | Follicular cells synthesize '''Thyroglobulin''' in their golgi apparatus. This is a glycoprotein consisting of 70 linked tyrosine molecules, 10% of which are ''iodinated'', and is stored in the colloid. |
| − | + | <br> | |
| − | The thyroglobulin is then split to form the two amino acid derivative [[Hormones - Anatomy & Physiology|hormones]] produced in the thyroid gland which are | + | The thyroglobulin is then split to form the two amino acid derivative [[Hormones - Anatomy & Physiology|hormones]] produced in the thyroid gland which are Triiodothyronine (T3) and Thyroxine (T4). Thyroxine contains 4 iodine atoms, triiodothyronine contains 3. Creation of these two [[Hormones - Anatomy & Physiology|hormones]] is the only role of iodine in the body. |
| − | + | <br> | |
The majority (90%) of hormone produced by the follicular cells is T4. T4 can only be made in the thyroid gland. It can then be converted by other tissues into T3. | The majority (90%) of hormone produced by the follicular cells is T4. T4 can only be made in the thyroid gland. It can then be converted by other tissues into T3. | ||
| + | <br> | ||
===Iodine Uptake=== | ===Iodine Uptake=== | ||
| − | Iodine circulates within the blood as | + | Iodine circulates within the blood as Iodide (I-). It is actively transported into the follicular cells by an Na+/I- symport in the basal membrane. This pump concentrates iodine in the colloid at a level up to 250x greater than the plasma level. This process is known as ''Iodide Trapping.'' The pump is activated by Thyroid Stimulating Hormone (TSH) a hormone from the [[Pituitary Gland - Anatomy & Physiology|pituitary gland]]. |
| − | |||
Any excess iodide is excreted via the [[Urinary System Overview - Anatomy & Physiology#Upper Urinary Tract|kidneys]]. | Any excess iodide is excreted via the [[Urinary System Overview - Anatomy & Physiology#Upper Urinary Tract|kidneys]]. | ||
| + | <br> | ||
===Secretion of Thyroid Hormones=== | ===Secretion of Thyroid Hormones=== | ||
Colloid uptake into the follicular cells takes place by endocytosis. The intracellular vesicles containing the colloid then fuse with lysosomes, where enzymes split the thyroglobulin into T3 and T4. The hormones diffuse across the basal plasma membrane into the interstitium (they are lipid soluble hormones). | Colloid uptake into the follicular cells takes place by endocytosis. The intracellular vesicles containing the colloid then fuse with lysosomes, where enzymes split the thyroglobulin into T3 and T4. The hormones diffuse across the basal plasma membrane into the interstitium (they are lipid soluble hormones). | ||
| + | <br> | ||
===Transport=== | ===Transport=== | ||
| − | Thyroid hormones are lipid soluble, thus need a transporting protein in order to travel in the blood. Half-life in the blood is 1 day for T3, 6 days for T4. 99% of thyroid hormones in circulation are bound. | + | Thyroid hormones are lipid soluble, thus need a transporting protein in order to travel in the blood.Half-life in the blood is 1 day for T3, 6 days for T4. |
| − | + | 99% of thyroid hormones in circulation are bound. | |
| − | The primary transport protein for thyroid hormones is ''' | + | The primary transport protein for thyroid hormones is '''Thyroid Binding Globulin''' (TBG). Synthesized in the [[Liver - Anatomy & Physiology|liver]], this protein binds 70-80% of the circulating thyroid hormones. |
| − | + | <br> | |
| − | The remainder are carried by ''' | + | The remainder are carried by '''Thyroxine-binding prealbumin''' or '''albumin'''. |
| + | <br> | ||
===Degradation=== | ===Degradation=== | ||
Only free T3 and free T4 can enter cells to exert their actions. T4 is deiodinated to T3 in many cells of the body, particularly the liver and kidneys. | Only free T3 and free T4 can enter cells to exert their actions. T4 is deiodinated to T3 in many cells of the body, particularly the liver and kidneys. | ||
| − | + | <br> | |
| − | The thyroid secretes 90% T4, with 50% of this being deiodinated to T3. The remainder is converted to | + | The thyroid secretes 90% T4, with 50% of this being deiodinated to T3. The remainder is converted to Reverse T3 (rT3). This is an inactive form of T3, and so creation of it is a regulatory mechanism. More rT3 is created when the body needs to reduce the action of T3 and T4. |
| − | + | <br> | |
The hormones are further deiodinated to diiodothyronine and monoiodothyronine in the liver and kidneys. Iodine is recycled or excreted in the urine. | The hormones are further deiodinated to diiodothyronine and monoiodothyronine in the liver and kidneys. Iodine is recycled or excreted in the urine. | ||
| + | <br> | ||
===Regulation=== | ===Regulation=== | ||
| − | + | The Hypothalamus releases '''Thyrotropin Releasing Hormone''' (TRH) which stimulates the adenohypophysis (anterior [[Pituitary Gland - Anatomy & Physiology|pituitary gland]]) to release '''Thyroid Stimulating Hormone''' (TSH). This water soluble hormone travels in the blood to activate the thyroid gland by 5 actions: | |
| − | The | ||
#Increased endocytosis and proteolysis of thyroglobulin from colloid | #Increased endocytosis and proteolysis of thyroglobulin from colloid | ||
| − | #Increased activity of the Na | + | #Increased activity of the Na+/I- Symport |
#Increased iodination of tyrosine | #Increased iodination of tyrosine | ||
#Increased size and secretory activity of thyroid follicular cells | #Increased size and secretory activity of thyroid follicular cells | ||
#Increased number of follicular cells | #Increased number of follicular cells | ||
| + | |||
| + | [[Image:HypothalamicPituitaryThyroidAxis.jpg|thumb|240px|center|'''Schematic Diagram of the Hypothalamic - Pituitary - Thyroid Axis]] | ||
| + | <br> | ||
===Thyroid Hormone Actions=== | ===Thyroid Hormone Actions=== | ||
| − | T3 and T4 have effects on all body systems and at all stages of life. These include | + | T3 and T4 have effects on all body systems and at all stages of life. These include '''Development''' where thyroid hormones are vital during the fetal period and the first few months after birth. T3 and T4 are the hormones for metamorphosis in frogs. Thyroid hormones also promote '''Growth''' as they enhance amino acid uptake by tissues and enzymatic systems involved in protein syntheis, promotes bone growth. They also help with metabolic actions such as '''Carbohydrate metabolism''', as thyroid hormones stimulate glucose uptake, glycogenolysis, gluconeogenesis. In '''Fat metabolism''' they mobilise lipids from adipose stores and accelerate oxidation of lipids to produce energy (occurs within mitochondria), as well as increasing the size and number of mitochondria. Thyroid hormones also '''Increase Basal Metabolic Rate''' (BMR) in all tissues except brain, spleen and gonads. The results in increased heat production, increased oxygen consumption. This increased metabolic rate also results in increased utilisation of energy substrates causing weight loss. Some of thyroid hormones [[Cardiorespiratory System Overview - Anatomy & Physiology#Cardiovascular System|'''Cardiovascular actions''']] are to increase cardiac output, heart rate and contractility. They affect the [[Cardiorespiratory System Overview - Anatomy & Physiology#Upper Respiratory Tract|'''Respiratory system''']] indirectly through increased BMR causing increased demand for oxygen and increased excretion of carbon dioxide. In the [[Nervous and Special Senses - Anatomy & Physiology#Nervous System|'''Nervous system''']] thyroid hormones are required for myelination of [[PNS Structure - Anatomy & Physiology#Neurons|neurons]] during the development of this system. They also enhance the sympathetic nervous system (by increasing epinephrine receptors). [[Reproductive System Overview - Anatomy & Physiology|'''Reproductive System''']] is affected if thyroid hormone levels decrease reduced levels of thyroid hormone causes irregular cycling, decreased libido. Finally, in the [[Alimentary System Overview - Anatomy & Physiology|'''Alimentary System''']] - Thyroid hormone increases appetite and feed intake, increases secretion of [[Pancreas - Anatomy & Physiology|pancreatic]] enzymes and increases motility. |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | <br> | |
| − | |||
| − | + | ==Problems associated with the Thyroid Gland== | |
| − | + | Problems with the thyroid gland include enlargement, or [[Goitre|Goitre]] and also the effects of increased level of hormones in [[Hyperthyroidism|Hyperthyroidism]] or decreased levels of hormones in [[Hypothyroidism|Hypothyroidism]]. | |
| − | |||
| − | |||
| − | |||
| − | + | <br> | |
| − | ''' | + | ==Functional Anatomy (summary)== |
| − | + | The thyroid gland lies in the neck, in front of the upper part of the trachea. Two types of hormones are produced, which are the iodine containing hormones; '''Tri-iodothyronine'''(T3) and '''Thyroxine''' (T4). Thyroid hormones regulate the basal metabolic rate and are important in the regulation of growth of tissues, particularly nervous tissue. Release stimulated by TSH from the pituitary. The second type of hormone produced from the thyroid gland is '''Calcitonin''', which regulates blood calcium levels along with parathyroid hormone and acts to reduce blood calcium by inhibiting its removal from bone. | |
| − | Thyroid | + | <br> |
| − | + | The majority of the gland is derived from a downgrowth of the foetal tongue. The calcitonin producing cells are different and are derived from the fourth branchial pouch. | |
| − | + | [[Image:Normal thyroid.jpg|right|thumb|125px|<small><center>'''Normal Thyroid'''. Courtesy of A. Jefferies</center></small>]] | |
| − | + | The throid gland is divided into follicles which are bounded by a single layer of cuboidal epithelial cells and a basement membrane. Follicles contain a homogenous colloid material called '''thyroglobulin'''. This is a store of thyroid hormones prior to secretion. The thyroid gland is the only endocrine gland to store its hormone in large quantities. | |
| + | <br> | ||
| + | In the active gland colloid is diminished and epithelial cells are tall and columnar. | ||
| + | <br> | ||
| + | '''Parafollicular''' cells are found in clusters in the interfollicular space and are also known as '''clear''' cells as their cytoplasm doesn't stain with H and E. | ||
| + | These cells synthesise and secrete calcitonin in response to raised plasma calcium. | ||
| − | + | <br> | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| + | ==Test yourself with the Thyroid Gland Flashcards== | ||
| + | [[Thyroid_Gland_Flash_Cards_- Anatomy & Physiology|Thyroid Gland Flashcards]] | ||
| − | |||
| − | |||
| − | |||
[[Category:Endocrine System - Anatomy & Physiology]] | [[Category:Endocrine System - Anatomy & Physiology]] | ||
| − | [[Category: | + | [[Category:To Do - Review]] |
Revision as of 14:28, 8 April 2011
Embryological Origin
The thyroid gland is a downgrowth from the pharyngeal endoderm of the developing tongue.
Anatomy
The thyroid gland consists of two lobes (dog, horse), one on each lateral side of the cranial trachea. In the pig the lobes are connected by an isthmus with a small, central pyramidal lobe as part of that structure. Cattle have a particularly wide isthmus.
Location
The thyroid gland is located adjacent to the cranial trachea. Close to the Recurrent Laryngeal nerve, carotid sheath and Sternohyoid and Sternothyroid muscles. The Parathyroid Glands are located dorsally to, or within the thyroid gland itself.
Supply
The thyroid gland is supplied by the Cranial Thyroid artery which is a branch of the common carotid artery. A subsidiary supply is provided by the Caudal Thyroid artery. The cranial and caudal thyroid arteries are united by substantial anastamoses along their caudal edge. Venous drainage is provided by the Internal Jugular vein and Lymph drains into the cranial Deep Cervical nodes.
Ultrastructure and Histology
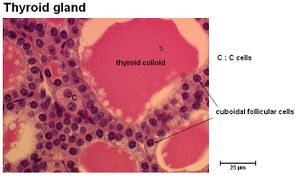
The gland consists of varying sized follicles. These are a single layer of cuboidal epithelial cells: Follicular Cells surrounding a central lumen filled with a protein rich colloid (thyrogloblin). The apical surface of the cell membranes is covered with numerous micovilli to increase surface area. The follicular cells are connected by tight junctions, and have a dense capillary network.
Within the connective tissue close to the follicles are C-Cells alternatively known as Parafollicular Cells. These secrete Calcitonin, a hormone which acts to lower plasma Ca2+ levels.
Histology
Thyroid Hormone Physiology
Follicular cells synthesize Thyroglobulin in their golgi apparatus. This is a glycoprotein consisting of 70 linked tyrosine molecules, 10% of which are iodinated, and is stored in the colloid.
The thyroglobulin is then split to form the two amino acid derivative hormones produced in the thyroid gland which are Triiodothyronine (T3) and Thyroxine (T4). Thyroxine contains 4 iodine atoms, triiodothyronine contains 3. Creation of these two hormones is the only role of iodine in the body.
The majority (90%) of hormone produced by the follicular cells is T4. T4 can only be made in the thyroid gland. It can then be converted by other tissues into T3.
Iodine Uptake
Iodine circulates within the blood as Iodide (I-). It is actively transported into the follicular cells by an Na+/I- symport in the basal membrane. This pump concentrates iodine in the colloid at a level up to 250x greater than the plasma level. This process is known as Iodide Trapping. The pump is activated by Thyroid Stimulating Hormone (TSH) a hormone from the pituitary gland.
Any excess iodide is excreted via the kidneys.
Secretion of Thyroid Hormones
Colloid uptake into the follicular cells takes place by endocytosis. The intracellular vesicles containing the colloid then fuse with lysosomes, where enzymes split the thyroglobulin into T3 and T4. The hormones diffuse across the basal plasma membrane into the interstitium (they are lipid soluble hormones).
Transport
Thyroid hormones are lipid soluble, thus need a transporting protein in order to travel in the blood.Half-life in the blood is 1 day for T3, 6 days for T4.
99% of thyroid hormones in circulation are bound.
The primary transport protein for thyroid hormones is Thyroid Binding Globulin (TBG). Synthesized in the liver, this protein binds 70-80% of the circulating thyroid hormones.
The remainder are carried by Thyroxine-binding prealbumin or albumin.
Degradation
Only free T3 and free T4 can enter cells to exert their actions. T4 is deiodinated to T3 in many cells of the body, particularly the liver and kidneys.
The thyroid secretes 90% T4, with 50% of this being deiodinated to T3. The remainder is converted to Reverse T3 (rT3). This is an inactive form of T3, and so creation of it is a regulatory mechanism. More rT3 is created when the body needs to reduce the action of T3 and T4.
The hormones are further deiodinated to diiodothyronine and monoiodothyronine in the liver and kidneys. Iodine is recycled or excreted in the urine.
Regulation
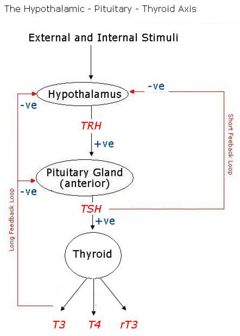
The Hypothalamus releases Thyrotropin Releasing Hormone (TRH) which stimulates the adenohypophysis (anterior pituitary gland) to release Thyroid Stimulating Hormone (TSH). This water soluble hormone travels in the blood to activate the thyroid gland by 5 actions:
- Increased endocytosis and proteolysis of thyroglobulin from colloid
- Increased activity of the Na+/I- Symport
- Increased iodination of tyrosine
- Increased size and secretory activity of thyroid follicular cells
- Increased number of follicular cells
Thyroid Hormone Actions
T3 and T4 have effects on all body systems and at all stages of life. These include Development where thyroid hormones are vital during the fetal period and the first few months after birth. T3 and T4 are the hormones for metamorphosis in frogs. Thyroid hormones also promote Growth as they enhance amino acid uptake by tissues and enzymatic systems involved in protein syntheis, promotes bone growth. They also help with metabolic actions such as Carbohydrate metabolism, as thyroid hormones stimulate glucose uptake, glycogenolysis, gluconeogenesis. In Fat metabolism they mobilise lipids from adipose stores and accelerate oxidation of lipids to produce energy (occurs within mitochondria), as well as increasing the size and number of mitochondria. Thyroid hormones also Increase Basal Metabolic Rate (BMR) in all tissues except brain, spleen and gonads. The results in increased heat production, increased oxygen consumption. This increased metabolic rate also results in increased utilisation of energy substrates causing weight loss. Some of thyroid hormones Cardiovascular actions are to increase cardiac output, heart rate and contractility. They affect the Respiratory system indirectly through increased BMR causing increased demand for oxygen and increased excretion of carbon dioxide. In the Nervous system thyroid hormones are required for myelination of neurons during the development of this system. They also enhance the sympathetic nervous system (by increasing epinephrine receptors). Reproductive System is affected if thyroid hormone levels decrease reduced levels of thyroid hormone causes irregular cycling, decreased libido. Finally, in the Alimentary System - Thyroid hormone increases appetite and feed intake, increases secretion of pancreatic enzymes and increases motility.
Problems associated with the Thyroid Gland
Problems with the thyroid gland include enlargement, or Goitre and also the effects of increased level of hormones in Hyperthyroidism or decreased levels of hormones in Hypothyroidism.
Functional Anatomy (summary)
The thyroid gland lies in the neck, in front of the upper part of the trachea. Two types of hormones are produced, which are the iodine containing hormones; Tri-iodothyronine(T3) and Thyroxine (T4). Thyroid hormones regulate the basal metabolic rate and are important in the regulation of growth of tissues, particularly nervous tissue. Release stimulated by TSH from the pituitary. The second type of hormone produced from the thyroid gland is Calcitonin, which regulates blood calcium levels along with parathyroid hormone and acts to reduce blood calcium by inhibiting its removal from bone.
The majority of the gland is derived from a downgrowth of the foetal tongue. The calcitonin producing cells are different and are derived from the fourth branchial pouch.
The throid gland is divided into follicles which are bounded by a single layer of cuboidal epithelial cells and a basement membrane. Follicles contain a homogenous colloid material called thyroglobulin. This is a store of thyroid hormones prior to secretion. The thyroid gland is the only endocrine gland to store its hormone in large quantities.
In the active gland colloid is diminished and epithelial cells are tall and columnar.
Parafollicular cells are found in clusters in the interfollicular space and are also known as clear cells as their cytoplasm doesn't stain with H and E.
These cells synthesise and secrete calcitonin in response to raised plasma calcium.